Venous thromboembolism, which includes both deep venous thrombosis and pulmonary embolism, is a major cause of morbidity and mortality among patients with cancer. The impact of ABO blood type in the development of venous thromboembolism in cancer patients remains controversial. To develop a sense of current opinion in this area, we conducted a systematic review and meta-analysis. Our systematic review and meta-analysis show that non-O blood type is associated with higher risk of development of venous thromboembolism among patients with cancer. Blood type is routinely determined preoperatively by objective and standardized methods, and our results suggest that these blood type results are useful for risk stratification and potentially for encouraging appropriate strategies for implementation of prophylactic treatment strategy in venous thromboembolism management.
1. Introduction
Venous thromboembolism, which includes both deep venous thrombosis and pulmonary embolism, is a major cause of morbidity and mortality among patients with cancer [
1,
2]. In particular, venous thromboembolism is a serious and frequent complication of pelvic surgery for malignancy and is the most common cause of mortality in patients who die within 30 days after surgery [
3,
4].
Although our references reported several types of genetic predisposition to venous thromboembolism, such as single-nucleotide polymorphisms (SNPs), most of those variations were encountered so rarely that their clinical importance remains controversial [
5]. It is thus important to characterize predisposing factors for venous thromboembolism, so that risk can be stratified accurately and prophylactic treatment strategies can be implemented effectively.
Previous hematologic studies have reported that ABO blood type is a significant genetic risk factor for venous thromboembolism [
6,
7]. Specifically, among the four blood groups (A, B, AB, and O), the risk of venous thromboembolism has been found to be significantly higher for non-O blood types than for type O [
6,
7]. However, no systematic assessment has been conducted of the relationship between blood type and venous thromboembolism risk in patients with cancer.
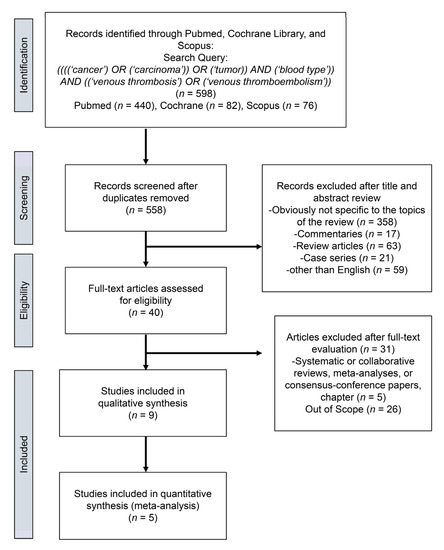
2. Study Selection
We found a total of 598 studies for an initial assessment. From these, we removed 40 duplicates and excluded non-relevant studies, review articles, meeting abstracts, case reports, replies, editorials or commentaries, and studies in languages other than English. This left 40 studies for review, from which we identified nine studies for systematic review [
13,
14,
15,
16,
17,
18,
19,
20,
21] and five studies [
14,
15,
17,
18,
19] for qualitative meta-analysis (
Figure 1).
Figure 1. Preferred Reporting Items from the Systematic Review and Meta-Analysis (PRISMA) flow chart showing the process of article selection.
3. Characteristics of the Included Studies
Table 1 lists the general characteristics of the eligible studies. All studies had a retrospective design and were published between 2004 and 2020. Patients were enrolled from Europe in 1 study, from North America in 7 studies, and from Asia in 1 study. Overall, 1118 of 25,884 patients developed venous thromboembolism. The treatment details were reported for seven studies in 24,996 patients: 24,473 of those patients (97.9%) underwent a surgical procedure (biopsy or surgical resection). The rate of development of venous thromboembolism in patients whose blood type was O and non-O was 9.2% and 13.6%, respectively. All of the eligible studies were retrospective, so pharmacologic prophylaxis was not standardized. In addition, the timing of diagnostic evaluation of patients for venous thromboembolism was based on symptom presentation and/or clinical evaluation, and most of the studies did not follow a precise protocol. Multivariate logistic regression analyses were not performed in three studies [
13,
16,
20], and although Wang et al. evaluated the association of venous thromboembolism with ABO blood type, they reported a higher risk of each non-O blood type (A/B/AB) compared to O blood type (OR (95% CI); A: 2.072 (1.204–3.566), B: 1.944 (1.020–3.873), AB: 2.706 (1.432–5.114)). These four studies were excluded from our meta-analysis.
Table 1. Characteristics of all articles included in the study.
| VTE |
|
| First Author of Study and [Ref.] |
Country |
Recruitment Period |
Study Design |
Total |
Yes |
No |
NOS |
| Streiff et al. [13] |
USA |
1991–2001 |
Cohort, retrospective |
130 |
28 |
102 |
6 |
| Tollefson et al. [14] |
USA |
1987–2010 |
Cohort, retrospective |
18472 |
271 |
18201 |
7 |
| Wang J et al. [15] |
USA |
1980–2005 |
Cohort, retrospective |
2076 |
216 |
2060 |
7 |
| Mizrahi et al. [16] |
Canada |
1995–2013 |
Cohort, retrospective |
523 |
56 |
467 |
6 |
| Li et al. [17] |
USA |
NR |
Cohort, retrospective |
670 |
236 |
434 |
6 |
| Spavor et al. [18] |
Canada |
NR |
Cohort, retrospective |
218 |
63 |
155 |
6 |
| Bhanvadia et al. [19] |
USA |
2003–2015 |
Cohort, retrospective |
1341 |
90 |
1251 |
7 |
| Heenkenda et al. [20] |
Sweden |
NR |
Cohort, retrospective |
139 |
47 |
92 |
6 |
| Wang G et al. [21] |
China |
2018–2019 |
Cohort, retrospective |
2315 |
131 |
2174 |
7 |
NOS, Newcastle-Ottawa Scale; VTE, venous thromboembolism; NR, not reported.
4. Meta-Analysis
The association of ABO blood type with development of venous thromboembolism in patients with cancers.
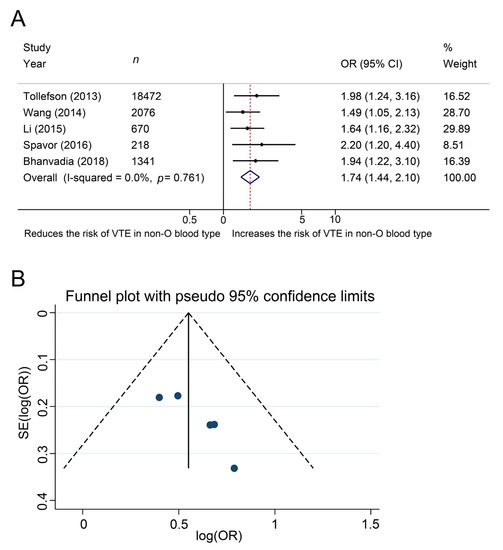
The impact of ABO blood type on the development of venous thromboembolism was investigated in five studies, in a total of 22,777 patients with cancer. The Cochrane Q test (chi-square 1.86, p = 0.761) and the I2 test (I2 = 0.0%) showed no heterogeneity, so we used a fixed-effect model. The forest plots indicated a significant association between non-O blood type and the development of venous thromboembolism (pooled OR: 1.74, 95% CI, 1.44–2.10, z = 5.70, Figure 2A). The funnel plots showed no studies exceeding the pseudo 95% CI (Figure 2B).
Figure 2. Forest (A) and funnel (B) plot showing the association of ABO blood type with the development of venous thromboembolism among patients with cancer.
5. Additional Analysis
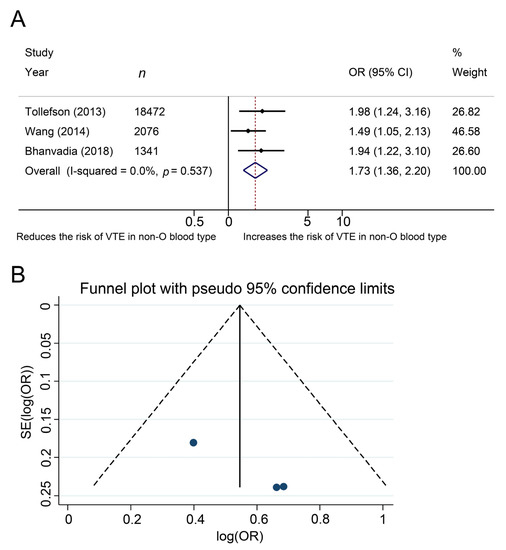
The association of ABO blood type with the development of venous thromboembolism in patients after pelvic surgery for malignancy.
The effects of ABO blood type on the development of venous thromboembolism was investigated in three studies, in a total of 21,889 patients with cancer after pelvic surgery. The Cochrane Q test (chi-square 1.24, p = 0.537) and the I2 test (I2 = 0.0%) showed no heterogeneity, so we used a fixed-effect model. The forest plots demonstrated that non-O blood type was significantly associated with the development of venous thromboembolism (pooled OR: 1.73, 95% CI, 1.36–2.20, z = 4.43, Figure 3A). The funnel plots did not demonstrate any study over the pseudo 95% CI (Figure 3B).
Figure 3. Forest (A) and funnel (B) plot showing the association of ABO blood type with the development of venous thromboembolism among patients who underwent pelvic surgery for urological cancer.
This entry is adapted from the peer-reviewed paper 10.3390/jcm10163692