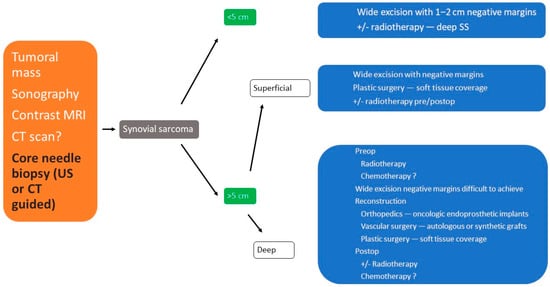
2.1. Clinical Presentation
Soft tissue sarcomas may appear anywhere in the body, with the majority of them being located at the level of the lower limb, mostly around the knee or hip joint. The nomenclature of synovial sarcoma might be confusing since their origin is not the synovial tissue but the primitive mesenchymal cells [
10].
In the early stages, small synovial sarcomas may cause insignificant signs or symptoms. As the tumor grows larger, the patient may notice a mass or swelling of the affected region. In some cases, the tumor can limit the range of motion or cause numbness and/or pain if it presses on nearby nerves [
11]. The common clinical appearance is a slow-growing painless mass and may give the false impression of being benign. Based on the tumor location, some functional impairment may appear. Sometimes, the symptoms of a synovial sarcoma can be mistaken with other inflammatory conditions, such as bursitis and synovitis, or it may go unnoticed for a long time. Plain radiographs often show small calcifications within the mass. This finding should alert the physician to the diagnosis [
12].
Synovial sarcoma may first be suspected in the presence of characteristic signs and symptoms. Additional tests may be required in order to determine the correct diagnosis and the severity of the condition.
2.2. Imaging Examinations
X-ray: Simple X-rays are not sensitive enough for the diagnosis of SS. Usually, an X-ray is the first imaging study performed as a routine procedure in the presence of an overgrown tumoral mass in an extremity. Calcifications, which can mimic myositis ossificans, and bone involvement (erosions, osteolysis) may be observed on plain X-rays (Figure 1).
Figure 1. Synovial sarcoma, F, 40 YO—radiological AP view of the right hip and proximal thigh (prior to CT exam) reveals the presence of soft tissue calcifications medial to the lesser trochanter.
Magnetic resonance imaging (MRI) with contrast should be considered for tumors exceeding 2–3 cm and is probably the imaging method of choice for synovial sarcomas. MRI will provide valuable information regarding the extent of the tumor and the relationship with the surrounding anatomical structures; the use of a gadolinium contrast will enhance the amount of information that can be obtained since it is able to differentiate between hemorrhagic areas and solid tumoral tissue.
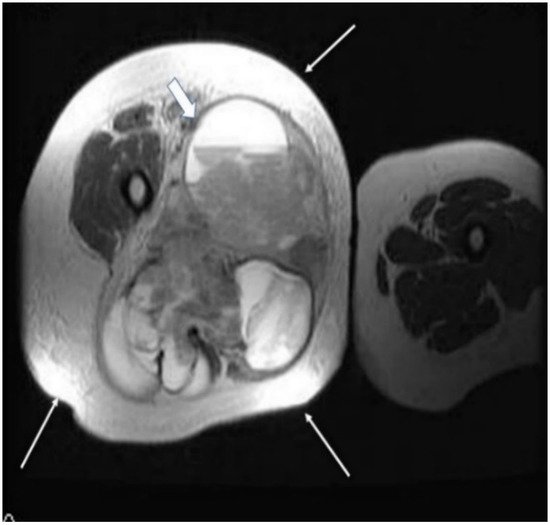
The T2 sequences are more specific for the diagnosis of soft tissue sarcomas and can reveal an inhomogeneous tumor, mainly with a hyperintense signal, in contrast with muscles, and the specific “triple sign” is present, representing a mixture of solid parts (medium hemorrhage and/or necrosis (high signal intensity) and calcifications or/and fibrotic areas (low signal intensity). The heterogeneity is completed by the presence of cystic parts with an aspect of fluid–fluid levels due to blood sedimentation (Figure 2 and Figure 3).
Figure 2. A 40-year old female patient with synovial sarcoma. Image represents an axial MRI of the proximal right thigh—axial T2 FSE (fast spin echo) and FATSAT (fat saturation). There is an increased diameter of the right thigh because of a soft tissue mass (thin arrows), where an inhomogeneous mixture of solid and cystic areas is shown (block arrow).
Figure 3. Same patient as in Figure 1 and Figure 2, MR image, coronal T2 STIR (short-time inversion recovery): heterogeneous soft tissue mass showing a mixture of solid areas (line arrow), hemorrhage and/or necrosis (block arrow), calcifications or fibrosis, cystic elements and infiltration of adjacent fat. Furthermore, fluid–fluid levels (block arrow) can be observed in this figure.
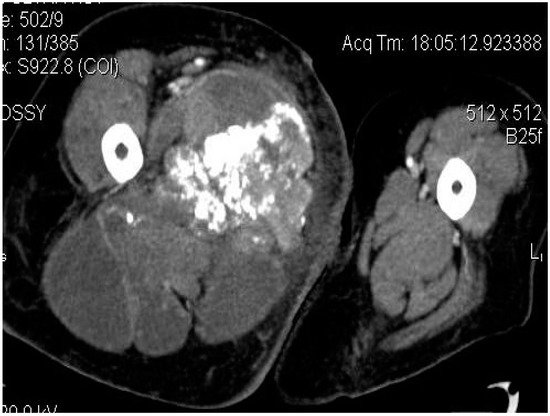
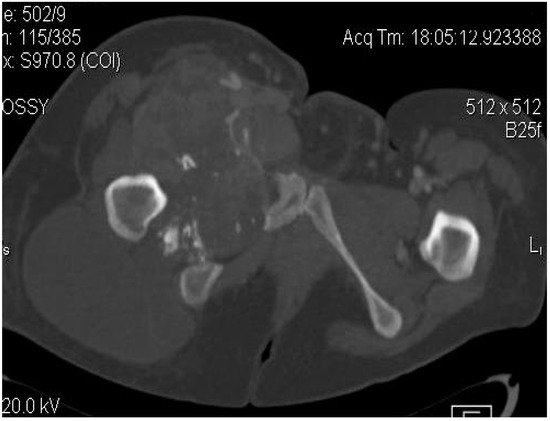
Computed tomography (CT) is usually performed either if the MRI is contraindicated (e.g., due to the presence of orthopedic implants), is unavailable or if the radiologists need additional information regarding the local bone involvement or better visualization of the intratumoral calcifications (Figure 4, Figure 5 and Figure 6).
Figure 4. Axial CT-scan: evident enlargement of the right thigh; heterogeneous soft-tissue mass with calcifications, adjacent fat infiltration and skin thickening—synovial sarcoma, M, 26 YO patient.
Figure 5. Synovial sarcoma, F, 31 YO patient—CT image, axial section: soft-tissue mass with heterogeneous content, showing necrotic areas alternating with calcifications and cystic areas.
Figure 6. Synovial sarcoma, F, 31 YO patient, CT image, axial section, with contrast—bone window: osteolytic area in the right ischio-pubic rami.
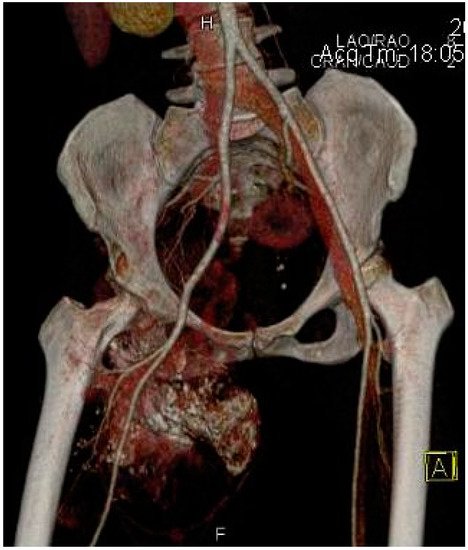
Other imaging examinations may be required. For example, a bone scan may be useful in detecting possible metastatic lesions or an Angio-CT may be requested by the oncologic surgeon, especially for deep synovial sarcomas in order to understand the relationship of the tumor with the neurovascular structures for appropriate preoperative planning (Figure 7).
Figure 7. Angio-CT with 3D reconstruction indicating the relationship of the synovial sarcoma with the major arterial vessels and the tumoral vascularization.
2.3. Biopsy
A biopsy is mandatory for a proper diagnosis in patients with synovial sarcoma; moreover, it will allow the morphopathologist to differentiate this tumor, especially from other soft tissue sarcomas, and to define the tumor staging.
In order to harvest a representative sample of tumoral tissue, there are several options available, including: a fine needle aspiration, a core needle biopsy (with or without imaging guidance) and an incisional biopsy.
At this point, a core needle biopsy is considered to probably be the best choice, especially if it is performed under ultrasonographic or tomographic guidance for deep, nonpalpable tumors. The major advantage of a core needle biopsy is the amount of tissue that can be retrieved compared to a fine needle aspiration and the small rate of complications compared to an incisional biopsy [
11,
13].
An incisional biopsy should be performed by a musculoskeletal oncologist or after consulting them, where the size of the incision should be as small as possible and it should be in line with the planned incision for the tumoral excision. A good surgical technique is required with careful hemostasis in order to avoid hematoma formation.
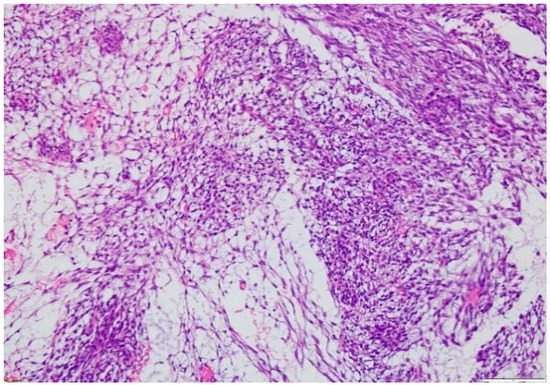
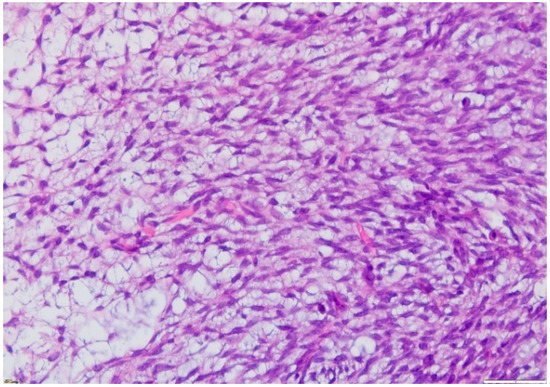
The microscopic exam of the synovial sarcoma will indicate one of the three possible variants: monophasic, biphasic or poorly differentiated. For the first variant, the cellularity is represented by spindle cells, whereas in a biphasic synovial sarcoma, there may also be epithelial cells present (Figure 8 and Figure 9). Furthermore, the microscopic exam may reveal the presence of calcifications/ossification areas in up to one-third of cases.
Figure 8. Microscopic findings—classical synovial sarcoma with two main subtypes: biphasic and monophasic appearance, and with two typical cell types: spindle cells and epithelial cells (fusocellular proliferation with myxoid areas, detail), which is rare (HE staining, 20×).
Figure 9. Microscopic finding—monophasic subtype of a synovial sarcoma with mesenchymal spindle cell elements and fusocellular proliferation (HE staining, 40×).