Psychoneuroendocrineimmunology (PNEI) brings together knowledge acquired since the 1930s from endocrinology, immunology, neuroscience, and psychology. With PNEI, a model of research and interpretation of health and disease is emerging, which sees the human body as a structured and interconnected unit, where the psychological and biological systems are mutually coordinated. In the PNEI view, many factors could influence mental health, with the endocrine system involved in mediating the effects of environmental stress on mental health and inflammation in the onset and course of psychiatric disorders as a result of individual and collective conditions and behaviors. PNEI paradigm configures the possibilities of going beyond the historical and philosophical contrast between mind and body, as well as the scientific antithesis of the twentieth century, between medicine and psychology, overcoming their respective reductionism, which assigns the body to the first and the psyche to the second.
- food
- physical activity
- psychiatry
- inflammation
- depression
- body-mind
- integrated care
- pnei paradigm
- stress and disease
- epigenetics
[1][2][3][4][5][6][7][8][9][10][11][12][13][14][15][16][17][18][19][20][15][21][20][22][23][24][25][26][27][28][29][30][28][31][32][33][34][32][35][36][37][38][39][40][41]1. Historical background
THE INTERACTION BETWEEN THE NERVOUS AND IMMUNE SYSTEMS
Traditionally, two ideas hindered the conceptualization of neuroendocrine-immune relations. The first: the brain is an organ in itself, it is an exception, and it is not an organ like any other. In traditional physiological thinking, the brain was conceived as mainly inaccessible to the immune system. The brain is an immunologically privileged place, protected by the blood-brain barrier: this dogma, which still echoes here and there in medical congresses and some university departments, has been affected by the experiments of Hugo Besedovsky in the early 1980s and then demolished by research in the 1990s and then knocked down by the discovery of the cerebral lymphatic system in 2015.
The second conceptual obstacle can be summarized as follows: the immune system is made up of mobile and iridescent cells. How is a relationship between a highly differentiated static system and a mobile one, in perennial cellular maturation possible? The research was responsible for demonstrating first, that the immune system while being mobile and changing follows precise patterns of activation and control, and therefore it can be defined as a system and not a set of automatic and parcelled reactions; secondly, the central nervous system, although morphologically well structured, is not static; indeed, it is incredibly dynamic not only in functional but also morphological terms, as the manual you are reading extensively demonstrates.
But these prejudices of the dualist and reductionist paradigm have not prevented scientists, curious and oriented by other ideas, to look for the experimental evidence of the connections between the great systems of physiological regulation.
The box marks the main stages of these discoveries covering the last 40 years, of which we will now see the salient points and characters.
|
1975-1986. Systems interface. The first tests:
1987-1995. The paths of communication:
1996-2021. The vision of the entire network and the study of diseases:
Reprinted with permission from: F. Bottaccioli, and A.G. Bottaccioli (2020). Copyright 2020 Edra. |
Those discoveries the American experimental psychologist Robert Ader and the immunophysiologist, born in Argentina and German by adoption, Hugo Besedovsky are parallel research that first demonstrated the bidirectional communication between
the central nervous system and the immune system.
Ader, in the mid-seventies, together with Nicholas Cohen, immunologist, showed that the animal brain can influence the immune system. The model they used is that of classical conditioning (also called Pavlovian). The animal that receives, together with the conditioned stimulus (sugar), an immunosuppressant, after conditioning, to the administration
of the sugar presents immunosuppression [1].
This proves, albeit indirectly that the brain has connection lines to the immune system. Besedovsky, in those years, tried to demonstrate the inverse communication; that between immunity and the brain.
And indeed in 1981, then definitively in 1986, he showed that the products of the immune system, such as interleukin-1, could activate the stress axis with the final production of cortisol[2][3].
Research showed that the brain, during infection experimentally induced in the animal, is directly informed by the immune system through inflammatory cytokines, which reach the brain and especially the hypothalamus from the periphery of the body. At the time, the identified cytokine messenger was interleukin-1 (IL-1).
The neuropeptides, in fact, which are released by the fibers of the peripheral nervous tissue, or rather by the autonomic (sympathetic and parasympathetic) and the somatosensory nervous system, are the widespread communicators of the local relationships between the nervous system and immunity.
In the 1980s research on the molecular basis of communication between systems, taking advantage of the remarkable development that molecular immunology in those years focused on the structure of the lymphocyte membrane.
These studies showed that this fundamental class of immune cells has receptors for the essential hormones and transmitters produced by the brain.
A crucial point in this line of research is represented by an extensive written review, in 1989, by Edwin Blalock, the physiologist at the University of Alabama, in Birmingham, USA. In this paper [4], Blalock used the tools of molecular biology to show that the immune cells have receptors for the most important products of the central nervous system and that, at the same time, these cells can produce identical or similar substances to those of the brain. Thus, the molecular basis of the bidirectional nervous system-immunity interface was demonstrated for the first time. Research of the 1990s, centered on these links, provided considerable advancement in understanding inflammatory diseases by elaborating the concept of “neurogenic inflammation” produced by the nerve.
2. The study how Psychological stress influences biological systems
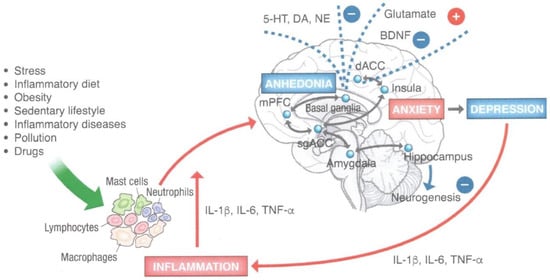
Research by the McEwen group [5] and other related groups aim to learn about the effects of chronic stress on the brain.
A series of studies, both animal and human, show that some brain areas undergo a process of neuronal loss, becoming atrophic, while in other regions the morphology of neurons changes, increase dendritic arborization and synaptic connections,
causing hypertrophy. The most important brain areas that undergo atrophy are the hippocampus and prefrontal cortices, both lateral and media. Relevant is the fact that chronic stress blocks the activity of stem cells in the hippocampus, from which it would be possible to replace lost neurons.
Therefore, neurogenesis of the hippocampus is blocked, as we have already mentioned above. The amygdala, on the other hand, becomes hypertrophic. The emotional-cognitive interweaving that accompanies and, at the same time, supports these
structural brain changes is characterized by anxiety and depression (amygdala), behavioral and executive changes (prefrontal cortices), and memory (hippocampus).
Spouses Ronald Glaser and Janice Kiecolt-Glaser, immunologist and psychologist respectively, both professors at Ohio University and members of the Institute of Medicine of the National Academy of Sciences of the United States, have been carrying out varied and highly active research for years on the effects of living conditions, behaviors and emotions on the immune system.
They have studied the immune systems of people who take care of the chronically ill, such as patients with Alzheimer’s, students in exam sessions and married couples, as well as the influence of depression and social isolation, and abuse in childhood. The considerable amount of data collected, both with observational and experimental studies shows that chronic psychic stress is a dominant factor that alters the immune dynamics, causing suppression and/or dysregulation, which can be the source of many significant diseases in which the immune system plays a central role [6].
In the following chapters, we will see the molecular biology of some of the relational dynamics that closely link emotions and immunities.
The stress axis influences all other endocrine axes, altering growth, sexuality, thyroid activity, and metabolic activities in general. One of the scholars who has been making an all-around contribution for three decades is the Greek scientist
George Chrousos, director of the Department of Paediatrics and Head of the Endocrinology Department at the University of Athens. The scientist’s prolificity can be seen in a large number of publications, the decades-long collaboration with the research programs of the American National Health Institutes, and the variety of research interests, which are all connected with a continuous thread: the study of the human being in its entirety.
His work documents that chronic hyperactivation of the stress, axis has significant repercussions even on apparently unreliable pathologies, such as metabolic disorders (dyslipidemia, hyperglycemia, diabetes, metabolic syndrome) and female fertility disorders, such as polycystic ovarian syndrome[7].
These studies have raised researchers’ awareness of the centrality of stress concerning devastating epidemics, such as obesity and diabetes, occurring in all the rich countries and also in those eastern countries that are following the Western model in forced stages.
3. The study how biological systems influence the psyche
4. A New Psychopathological Model
5. Stress Management and Psychological Interventions
New Frontiers
diagnostic tools that aim to capture the unbalanced factors of a person in their entirety, thus investigating both the psychological and the biological dimensions. Only new and more efficient diagnostic tools, in fact, can provide the basis for a treatment approach, which consists of prevention and therapy, to make it truly integrated and to provide qualified advice on lifestyles, which are then the primary determinants of health, to offer a treatment program that works on both the psychic
and the biological dimensions, to guarantee the use of therapeutic devices not restricted to synthetic pharmacology[41][42]
This entry is adapted from the peer-reviewed paper 10.3390/endocrines2030022
References
- Ader R., Cohen N. Behaviorally conditioned immunosuppression. Psychosomatic Medicine 1975, 37, 333-340
- Besedovsk y H.O., del Rey A., Sorkin E. Lymphokine-containing supernatants from con A-stimulated cells increase corticosterone blood levels. J Immunol 1981, 126, 385-387
- Besedovsk y H.O., del Rey A., Sorkin E. et al. Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science 1986, 233, 652-654.
- Blalock J.E. A molecular basis for bidirectional communication between the immune and neuroendocrine systems. Physiol. Rev. 1989, 69(1), 1-32.
- McEwen B.S., Morrison J.H. Brain on stress: vulnerability and plasticity of the prefrontal cortex over the life course. Neuron 2013, 79, 16-29.
- Glaser R., Kiecolt-Glaser J.K. Stress-induced immune dysfunction: implications for health. Nature Reviews Immunology 2005, 5, 243-251;
- Chrousos G. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009, 5(7), 374-81. doi: 10.1038/nrendo. 2009.106. Epub 2009 Jun 2.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; APA: Washington, DC, USA, 2013.
- Angell, M. The epidemic of mental illness: Why? N. Y. Rev. 2011, 58, 20–22.
- Gardner, C.; Kleinman, A. Medicine and the Mind—The Consequences of Psychiatry’s Identity Crisis. N. Engl. J. Med. 2019, 381, 1697–1699.
- Voineskos, A.N.; Mulsant, B.H.; Dickie, E.W.; Neufeld, N.H.; Rothschild, A.J.; Whyte, E.M.; Meyers, B.S.; Alexopoulos, G.S.; Hoptman, M.J.; Lerch, J.P.; et al. Effects of Antipsychotic Medication on Brain Structure in Patients with Major Depressive Disorder and Psychotic Features. JAMA Psychiatry 2020, 77, 674–683.
- Anderson, K.N.; Lind, J.N.; Simeone, R.M.; Bobo, W.V.; Mitchell, A.A.; Riehle-Colarusso, T.; Polen, K.N.; Reefhuis, J. Maternal Use of Specific Antidepressant Medications During Early Pregnancy and the Risk of Selected Birth Defects. JAMA Psychiatry 2020, 77, 1246–1255.
- Bottaccioli, F.; Bottaccioli, A.G. Psychoneuroendocrineimmunology and Science of Integrated Care. The Manual; Edra: Palm Beach, FL, USA, 2020.
- Dossett, M.L.; Fricchione, G.L.; Benson, H. A New Era for Mind-Body Medicine. N. Engl. J. Med. 2020, 382, 1390–1391.
- Tong, J.; Satyanarayanan, S.K.; Su, H. Nutraceuticals and probiotics in the management of psychiatric and neurological disorders: A focus on microbiota-gut-brain-immune axis. Brain Behav. Immun. 2020, 90, 403–419.
- Sarris, J.; Logan, A.C.; Akbaraly, T.N.; Amminger, G.P.; Balanzá-Martínez, V.; Freeman, M.P.; Hibbeln, J.; Matsuoka, Y.; Mischoulon, D.; Mizoue, T.; et al. Nutritional medicine as mainstream in psychiatry. Lancet Psychiatry 2015, 2, 271–274.
- Sarris, J. Nutritional Psychiatry: From Concept to the Clinic. Drugs 2019, 79, 929–934.
- Mandolesi, L.; Polverino, A.; Montuori, S.; Foti, F.; Ferraioli, G.; Sorrentino, P.; Sorrentino, G.; Mandolesi, L.; Polverino, A.; Montuori, S.; et al. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front. Psychol. 2018, 9, 509.
- Szyf, M. The epigenetics of perinatal stress. Dialogues Clin. Neurosci. 2019, 21, 369–378.
- Mattson, M.P. An Evolutionary Perspective on Why Food Overconsumption Impairs Cognition. Trends Cogn. Sci. 2019, 23, 200–212.
- Khan, A.; Plana-Ripoll, O.; Antonsen, S.; Brandt, J.; Geels, C.; Landecker, H.; Sullivan, P.F.; Pedersen, C.B.; Rzhetsky, A. Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLoS Biol. 2019, 17, e3000353.
- Zhai, L.; Zhang, Y.; Zhang, D. Sedentary behaviour and the risk of depression: A meta-analysis. Br. J. Sports Med. 2014, 49, 705–709
- McDowell, C.P.; Dishman, R.K.; Gordon, B.; Herring, M.P. Physical Activity and Anxiety: A Systematic Review and Meta-analysis of Prospective Cohort Studies. Am. J. Prev. Med. 2019, 57, 545–556.
- Stewart-Brown, S.; Samaraweera, P.C.; Taggart, F.; Kandala, N.-B.; Stranges, S. Socioeconomic gradients and mental health: Implications for public health. Br. J. Psychiatry 2015, 206, 461–465.
- Giebel, C.; Corcoran, R.; Goodall, M.; Campbell, N.; Gabbay, M.; Daras, K.; Barr, B.; Wilson, T.; Kullu, C. Do people living in disadvantaged circumstances receive different mental health treatments than those from less disadvantaged backgrounds? BMC Public Health 2020, 20, 1–10.
- Shoaff, J.R.; Coull, B.; Weuve, J.; Bellinger, D.C.; Calafat, A.M.; Schantz, S.L.; Korrick, S.A. Association of Exposure to Endocrine-Disrupting Chemicals During Adolescence with Attention-Deficit/Hyperactivity Disorder–Related Behaviors. JAMA Netw. Open 2020, 3, e2015041
- Shi, Y.; Qi, W.; Xu, Q.; Wang, Z.; Cao, X.; Zhou, L.; Ye, L. The role of epigenetics in the reproductive toxicity of environmental endocrine disruptors. Environ. Mol. Mutagen. 2020, 62, 78–88
- McEwen, B.S. Neurobiological and Systemic Effects of Chronic Stress. Chronic Stress 2017, 1.
- McEwen, B.S.; Nasca, C.; Gray, J.D. Stress Effects on Neuronal Structure: Hippocampus, Amygdala, and Prefrontal Cortex. Neuropsychopharmacology 2015, 41, 3–23.
- Slavich, G.M. Psychoneuroimmunology of Stress and Mental Health. In The Oxford Handbook of Stress and Mental Health; Oxford Handbooks Online; Oxford University Press: Oxford, UK, 2020
- Schiele, M.; Gottschalk, M.; Domschke, K. The applied implications of epigenetics in anxiety, affective and stress-related disorders—A review and synthesis on psychosocial stress, psychotherapy and prevention. Clin. Psychol. Rev. 2020, 77, 101830.
- Yehuda, R.; Daskalakis, N.P.; Desarnaud, F.; Makotkine, I.; Lehrner, A.L.; Koch, E.; Flory, J.D.; Buxbaum, J.D.; Meaney, M.J.; Bierer, L.M. Epigenetic Biomarkers as Predictors and Correlates of Symptom Improvement Following Psychotherapy in Combat Veterans with PTSD. Front. Psychiatry 2013, 4, 118.
- Bottaccioli, A.G.; Bottaccioli, F.; Minelli, A. Stress and the psyche-brain-immune network in psychiatric diseases based on psychoneuroendocrineimmunology: A concise review. Ann. N. Y. Acad. Sci. 2018, 1437, 31–42
- Miller, C.W.T. Epigenetic and Neural Circuitry Landscape of Psychotherapeutic Interventions. Psychiatry J. 2017, 2017, 1–38.
- Vinkers, C.H.; Geuze, E.; van Rooij, S.J.H.; Kennis, M.; Schür, R.R.; Nispeling, D.M.; Smith, A.K.; Nievergelt, C.M.; Uddin, M.; Rutten, B.P.F.; et al. Successful treatment of post-traumatic stress disorder reverses DNA methylation marks. Mol. Psychiatry 2019, 26, 1264–1271.
- Bower, J.E.; Irwin, M.R. Mind–body therapies and control of inflammatory biology: A descriptive review. Brain Behav. Immun. 2016, 51, 1–11
- Bottaccioli, F.; Carosella, A.; Cardone, R.; Mambelli, M.; Cemin, M.; D’Errico, M.M.; Ponzio, E.; Bottaccioli, A.G.; Minelli, A. Brief Training of Psychoneuroendocrinoimmunology-Based Meditation (PNEIMED) Reduces Stress Symptom Ratings and Improves Control on Salivary Cortisol Secretion Under Basal and Stimulated Conditions. Explor. J. Sci. Health 2014, 10, 170–179.
- Bottaccioli AG, Bottaccioli F, Carosella A, Cofini V, Muzi P, Bologna M. Psychoneuroendocrinoimmunology-based meditation (PNEIMED) training reduces salivary cortisol under basal and stressful conditions in healthy university students: Results of a randomized controlled study. Explore (NY). 2020 May-Jun;16(3):189-198. doi: 10.1016/j.explore.2019.10.006. Epub 2019 Nov 14. PMID: 31982328.
- Kiecolt-Glaser J. Psychoneuroimmunology. Psychology’s gateway to the biomedical future. Perspectives in Psychological Science 2009, 4: 367-369.
- McEwen B.S. Integrative medicine: Breaking down silos of knowledge and practice an epigenetic approach. Metabolism 2017, 69S:S21-S29. doi: 10.1016/j.metabol.2017.01.018. Epub 2017 Jan 11
- Bottaccioli, F.; Bottaccioli, A.G.; Marzola, E.; Longo, P.; Minelli, A.; Abbate-Daga, G. Nutrition, Exercise, and Stress Management for Treatment and Prevention of Psychiatric Disorders. A Narrative Review Psychoneuroendocrineimmunology-Based. Endocrines 2021, 2, 226-240. https://doi.org/10.3390/endocrines2030022
