The diagnosis and treatment of sepsis have always been a challenge for the physician, especially in critical care setting such as emergency department (ED), and currently sepsis remains one of the major causes of mortality. Although the traditional definition of sepsis based on systemic inflammatory response syndrome (SIRS) criteria changed in 2016, replaced by the new criteria of SEPSIS-3 based on organ failure evaluation, early identification and consequent early appropriated therapy remain the primary goal of sepsis treatment. Unfortunately, currently there is a lack of a foolproof system for making early sepsis diagnosis because conventional diagnostic tools like cultures take a long time and are often burdened with false negatives, while molecular techniques require specific equipment and have high costs. In this context, biomarkers, such as C-Reactive Protein (CRP) and Procalcitonin (PCT), are very useful tools to distinguish between normal and pathological conditions, graduate the disease severity, guide treatment, monitor therapeutic responses and predict prognosis.
- Presepsin
- sepsis
- emergency department
- critical care
- ICU
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
1. Introduction
2. Current Data on Presepsin as a Biomarker for Sepsis
2.1. Presepsin
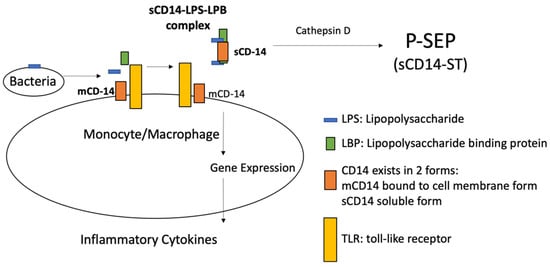
2.2. Presepsin Measurement
2.3. Diagnostic Significance of Presepsin in Sepsis
2.4. Prognostic Significance of Presepsin in Sepsis
2.5. Presepsin Compared to C-RP and PCT: Alone or in Company?
2.6. Presepsin in Pediatric Bacterial Infection
2.7. Presepsin in Fungal Infection
2.8. Presepsin Significance in SARS-CoV-2 Infection
2.9. Presepsin in Emergency Department
2.10. Presepsin Use Caveat
This entry is adapted from the peer-reviewed paper 10.3390/medicina57080770
