Diagonal earlobe crease is a wrinkle extending obliquely from the tragus towards the border of the earlobe. It was firstly described by Frank in 1973 in the New England Journal of Medicine in a case series of patients with coronary artery disease. Since then, there have been many reports published regarding its association mainly with atherosclerosis, especially coronary artery disease.
- coronary artery disease
- coronary syndromes
- diagonal earlobe crease
- Frank’s sign
1. Introduction
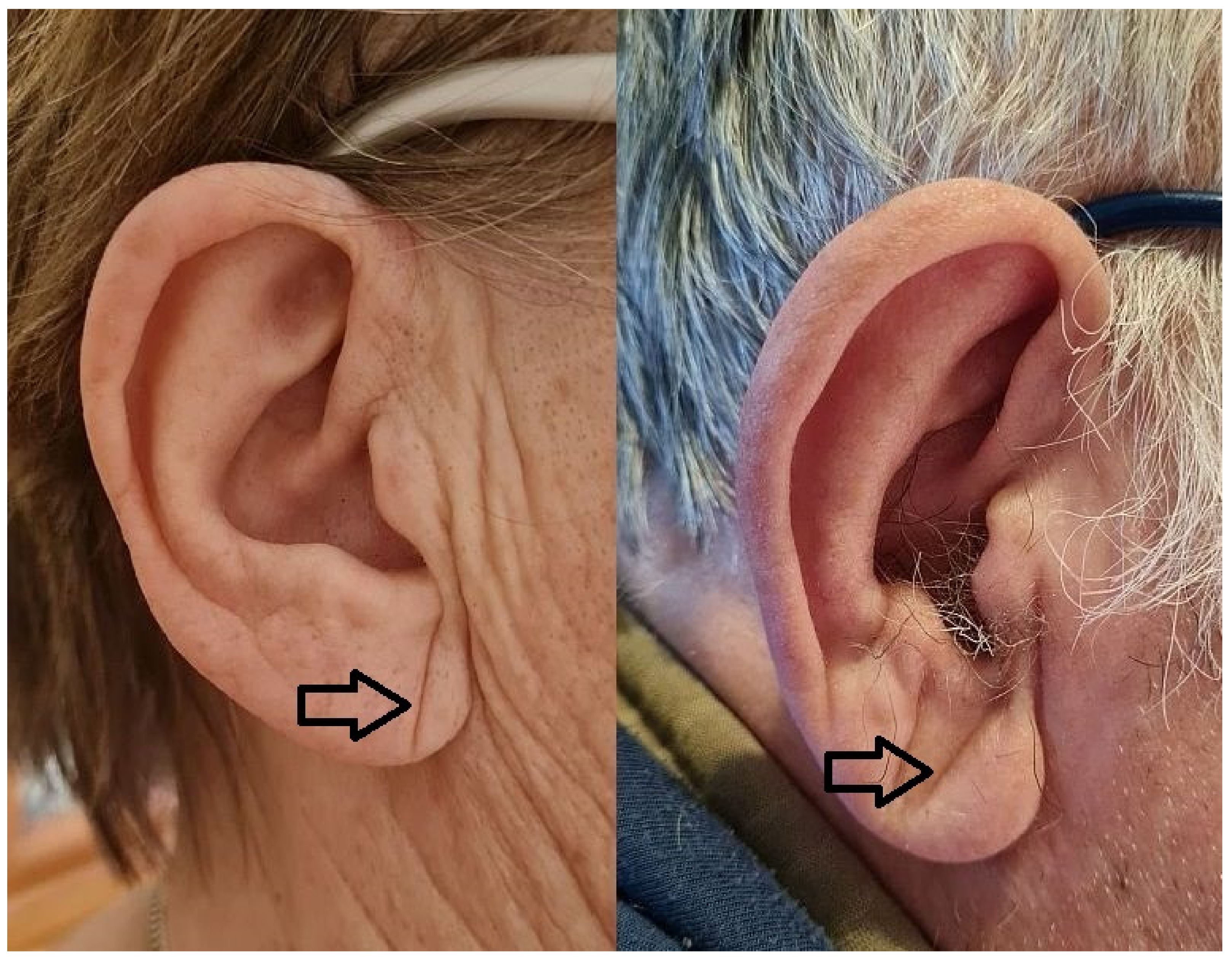 Figure 1. Diagonal earlobe crease in a woman without coronary artery disease and a man with coronary artery disease.
Figure 1. Diagonal earlobe crease in a woman without coronary artery disease and a man with coronary artery disease.2. Diagonal Earlobe Crease for Diagnosis of Coronary Artery Disease
Generally, most studies defined diagonal earlobe crease as at least a unilateral sign, in two papers bilateral sign was required to be considered as a positive, and another two presented results for both definitions. Two studies showed no more than information of diagonal creasing of earlobe without any other details. In another study, only the word “significant” was added to the positive sign description. One accepted any crease, whereas others provided detailed thresholds of the relation of the crease to the whole length of the earlobe which varied from more than one-third, at least half, at least two-thirds, or 100%. The combination of these approaches leads to the finding that DELC was defined in nine different ways.
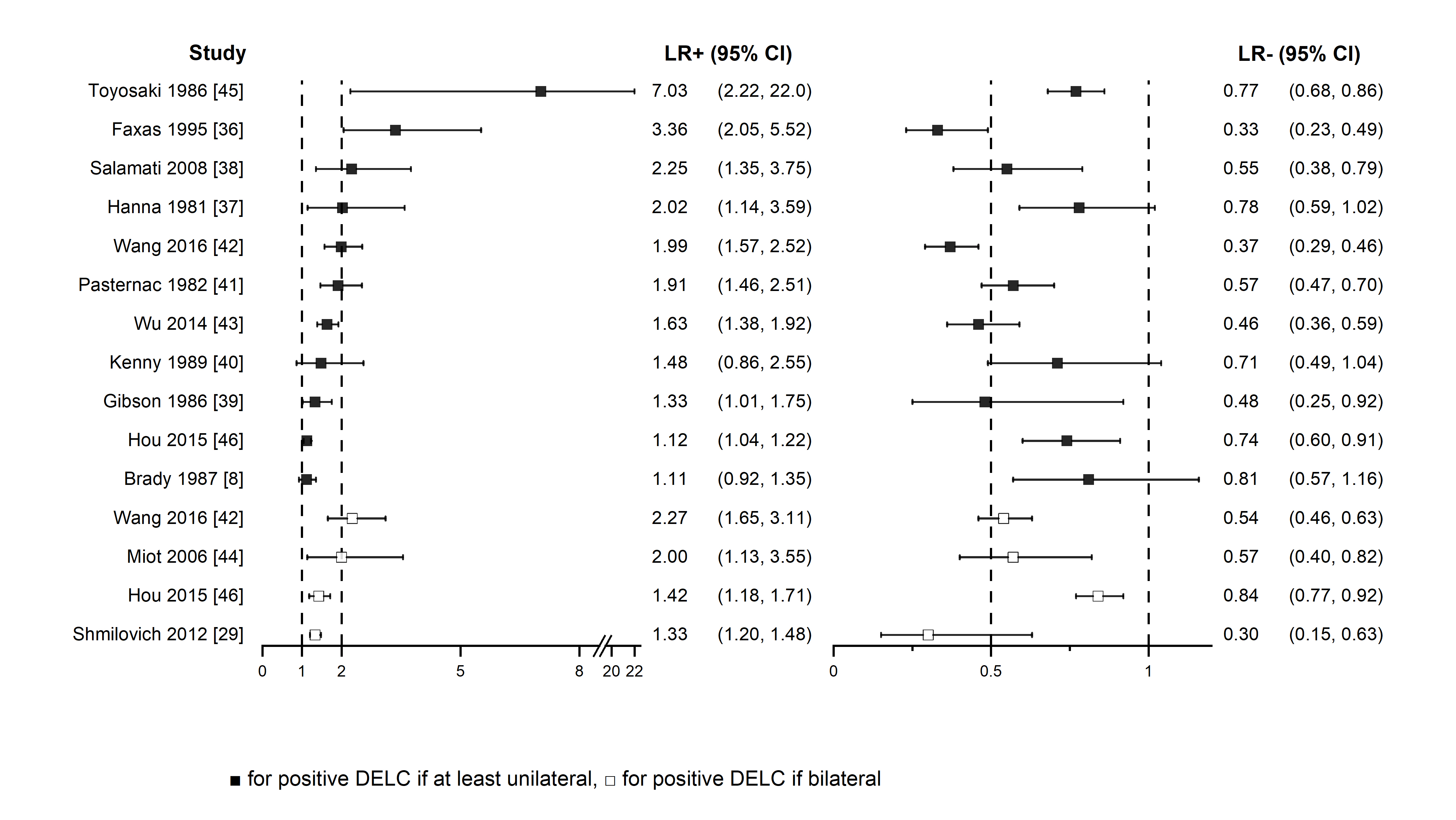 Figure 2. Positive and negative likelihood ratios forest plot
Figure 2. Positive and negative likelihood ratios forest plot3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/jcm10132799
References
- Sanchis-Gomar, F.; Perez-Quilis, C.; Leischik, R.; Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann. Transl. Med. 2016, 4, 256.
- Libby, P.; Theroux, P. Pathophysiology of Coronary Artery Disease. Circulation 2005, 111, 3481–3488.
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2019, 41, 407–477.
- Boudoulas, K.D.; Triposkiadis, F.; Geleris, P.; Boudoulas, H. Coronary Atherosclerosis: Pathophysiologic Basis for Diagnosis and Management. Prog. Cardiovasc. Dis. 2016, 58, 676–692.
- Frank, S.T. Aural Sign of Coronary-Artery Disease. N. Engl. J. Med. 1973, 289, 327–328.
- Pellen, J.-C. Frank’s Sign and Manifestations of Atherosclerosis: A Systematic Review of Literature. Master’s Thesis, Université Paris Diderot, Paris, France, 2014.
- Stoyanov, G.S.; Dzhenkov, D.; Petkova, L.; Sapundzhiev, N.; Georgiev, S. The histological basis of Frank’s sign. Head Neck Pathol. 2020, 15, 402–407.
- Brady, P.M.; Zive, M.A.; Goldberg, R.J.; Gore, J.M.; Dalen, J.E. A New Wrinkle to the Earlobe Crease. Arch. Intern. Med. 1987, 147, 65–66.
- Kaukola, S. The diagonal ear-lobe crease, a physical sign associated with coronary heart disease. Acta Med. Scand. Suppl. 1978, 619, 1–49.
- Higuchi, Y.; Maeda, T.; Guan, J.-Z.; Oyama, J.; Sugano, M.; Makino, N. Diagonal Earlobe Crease are Associated With Shorter Telomere in Male Japanese Patients With Metabolic Syndrome A Pilot Study. Circ. J. 2009, 73, 274–279.
- McGee, S. Simplifying likelihood ratios. J. Gen. Intern. Med. 2002, 17, 647–650.
- Tonino, P.A.L.; Fearon, W.F.; De Bruyne, B.; Oldroyd, K.G.; Leesar, M.A.; Ver Lee, P.N.; Maccarthy, P.A.; Van’t Veer, M.; Pijls, N.H. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J. Am. Coll. Cardiol. 2010, 55, 2816–2821.
