1. Introduction
Regardless of the initiating insult, vital organ functions, not necessarily affected primarily, fall victim to a dysregulated host response [1]. The cytokine storm originating from the immune over-response determines impairment of the vascular tone and systemic vasodilation, which manifests as hemodynamic instability. In its most serious form as vasoplegic circulatory shock, hemodynamic instability can be life-threatening; consequently, reversing shock as soon as possible is a lifesaving measure of utmost importance to avoid the devastating effects of hypoxemic organ damage [3]. The therapy has the potential to effectively remove cytokines originating from the cytokine storm [4,5], and thus can mitigate systemic hyperinflammation, contribute to early shock reversal, and last but not least, improve clinical outcomes.
Shock is currently defined by the task force from the European Society of Intensive Care Medicine (ESICM) as a “life-threatening, generalized form of acute circulatory failure associated with inadequate oxygen utilization by the cells” [6]. Generally, this means an imbalance between oxygen delivery (DO2) and oxygen consumption (VO2). DO2depends on cardiac output (CO) and the arterial oxygen content (CaO2), and VO2depends on mixed venous oxygen content ) − (Hb × 1.34 × SvO2+0.003 × PvO2),(1) where DO2is oxygen delivery; CO is cardiac output; Hb is hemoglobin; SaO2is arterial oxygen saturation; PaO2is partial pressure of oxygen in the arterial blood; CaO2is arterial oxygen content; VO2is oxygen consumption; SvO2is mixed venous oxygen saturation; CvO2is mixed venous oxygen content; PvO2is mixed venous oxygen tension.
Adequate oxygen supply is paramount for preserving organ viability and is dependent on adequate tissue perfusion. The latter is commonly assessed by mean arterial pressure (MAP), which is mainly determined by vascular tone (systemic vascular resistance—SVR). The relationship between SVR, MAP, central venous pressure (CVP) and CO is described below, based on Ohm’s law:(2)SVR=MAP−CVPCO
Loss of vascular tone (i.e., sepsis, hyperinflammation) results in low SVR, low MAP and preload deficit (i.e., vasoplegic shock). The different underlying mechanisms of hemodynamic instability also correspond to potential therapeutic options to be targeted, including fluids, inotropes, oxygen supplementation, and vasopressors to increase vascular tone, hence tissue perfusion. The differential diagnosis of hemodynamic instability or shock requires a skilled assessment of the complete clinical picture, which ranges from a simple measurement of vital signs such as heart rate and blood pressure, to complex, advanced hemodynamic monitoring [8]. The connection of inflammatory response–vasoplegia–tissue hypoperfusion–cytokine removal is depicted inFigure 1.
Different types of shock require different management strategies. However, hemodynamic stabilization always represents a main goal due to its role in reestablishing adequate aerobic metabolism in the cells and tissues, and in regaining control over the oxygen debt. Oxygen debt also accumulates during the resuscitation period, suggesting that shorter resuscitation times translate into lesser oxygen debts. Experimental studies suggest that both the severity and duration of hemodynamic instability are associated with poor outcomes [9].
In the past, the clinical and biochemical characteristics of vasoplegic shock were often defined within the domain of “septic shock”. However, similar features are also observed in non-infective inflammatory states, such as in acute necrotizing pancreatitis, after major trauma, major surgery, and in other conditions without an obvious infectious component. Interestingly, very similar observations were made many years before by Sir William Osler in the context of bacterial infections [11], and Hans Janos Selye in the context of stress [12]. Based on our current understanding, the term “hyperinflammatory shock” is preferred over “septic shock”, since it describes the pathophysiology more accurately and is applicable to both infectious and non-infectious etiologies.
The term “refractory shock” is commonly used to describe the most severe cases of hyperinflammatory shock. Although there is no clear consensus as to the exact definition for refractory shock, it is generally intended as shock persisting for more than 6 h despite initiation of full standard therapy, and is indicated by the following:Elevated lactate levels (>2.9 mmol/L) [13];High norepinephrine (NE) requirements ( >0.3 µg/kg/min)
Up to one-third of patients admitted to the intensive care unit (ICU) are in circulatory shock [14]. As noted already, the expert community now recommends the terms “hyperinflammatory” or “vasoplegic” shock over “septic shock” to better reflect the underlying pathophysiology of a “dysregulated host response” [1,5]. Accordingly, current Surviving Sepsis Guidelines recommend early and aggressive resuscitation within the first hours of the onset of sepsis and septic shock [18]. However, especially in vasoplegic shock, which is characterized by low SVR and consequently low diastolic blood pressure, a fluid challenge alone is often insufficient to improve tissue perfusion [19,20].
Vasopressors exert their effect by either mimicking the effect of the sympathetic nervous system (sympathomimetic amines) or by raising extracellular ionized calcium concentrations (calcium chloride). Sympathomimetic amines can be divided into either catecholamines or non-catecholamines. Commonly used catecholamines with a prominent agonist activity include epinephrine (also known as adrenaline), norepinephrine (noradrenaline) and dopamine. Norepinephrine is recommended as first line treatment of septic shock by the Surviving Sepsis campaign, but the combined use of vasopressors including both vasopressin and norepinephrine is also suggested to limit adrenoceptor desensitization due to sympathetic hyperactivation [23,24].
In patients with severe hyperinflammatory shock, neither vasopressors nor fluid resuscitation are effective in quickly reversing shock. Given the pathophysiological background, cytokine removal through hemoadsorption might be beneficial for patients showing resistance to resuscitation, i.e., not stabilized after 6 h of resuscitation and organ support. Cytokine removal can attenuate hyperinflammation and hence vasoplegia, leading to quicker hemodynamic stabilization and shock reversal. The most frequently used criteria to define shock reversal include normalization of serum lactate (<2.2 mmol/L) coupled with a significant (≥90%) reduction in norepinephrine dose requirements [13,25].
2. Results from Clinical Articles
Out of the 163 clinical articles available in PubMed, 58 were identified that mentioned “catecholamines and/or vasopressors”. In total, 25 papers were excluded; 12 because of non-comparability of the measurement scales [
25,
26,
27,
28,
29,
30,
31,
32,
33,
34,
35,
36]; 4 because the type and dose of vasopressors were not specified [
37,
38,
39,
40]; 1 that reported combined norepinephrine and epinephrine doses [
41]; 1 that only reported on patients that had survived [
42]; and 7 where there were no measurements pre- and post-adsorber use in the same patient [
43,
44,
45,
46,
47,
48,
49]. The remaining 33 articles were summarized without considering different study designs or duration of treatment. Overall, data on 353 patients treated with Cytosorb were collected.
Table A1 in
Appendix A depicts details from articles included in our review [
13,
50,
51,
52,
53,
54,
55,
56,
57,
58,
59,
60,
61,
62,
63,
64,
65,
66,
67,
68,
69,
70,
71,
72,
73,
74,
75,
76,
77,
78,
79,
80,
81]. From these papers, four were selected for a pooled comparative analysis due to their inclusion of both Cytosorb and a control cohort [
64,
75,
77,
79].
The highest and the lowest administered doses of norepinephrine for each day were reported at 24, 48, 72 or 96 h after the start of Cytosorb treatment, depending on the specific study. We assumed as the pre-Cytosorb value the dose administered before the start of the therapy or the highest dose recorded during the first 24 h before the start of hemoadsorption, depending on data availability, and the post-Cytosorb value as the lowest dose of norepinephrine administered and recorded during the last reported day. We assumed the last available norepinephrine dose measurement to be at the end of Cytosorb therapy for all patients in all studies analyzed. However, we are aware of at least one study [
13] wherein the norepinephrine dose was measured and recorded only during the first day, while the therapy was used for an additional two days. We still used the lowest available dose to determine norepinephrine requirements after hemoadsorption treatment.
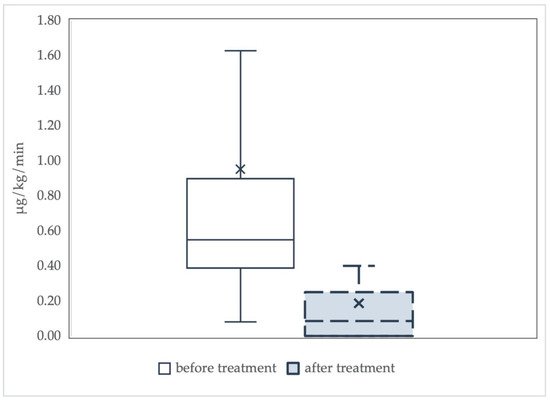
The descriptive analysis comprised 21 case reports, 11 case series and one randomized trial, and did not consider differences in the number of adsorbers used or the duration of treatment sessions. The results of the analysis are summarized in Figure 2.
Figure 2. Norepinephrine requirements before and after treatment with Cytosorb. Data are summarized as boxplots. The “x” in the box represents the mean value. There is a significant decline in median norepinephrine requirements before and after hemoadsorption with Cytosorb (from 0.55 (0.39–0.9) µg/kg/min to 0.09 (0.0–0.25) µg/kg/min, p < 0.001).
In 14 articles, including three case series, norepinephrine was weaned off after treatment with Cytosorb. Norepinephrine dosage was higher than 0.5 μg/kg/min at the end of the treatment with Cytosorb in one case report [
74], and in two case series [
12,
78]. The median dosage of norepinephrine required decreased by a full order of magnitude at the end of Cytosorb therapy. Overall, the available evidence shows that the norepinephrine dose requirements were markedly lower after Cytosorb treatment.
2.1. Analysis of Studies with Control Cohorts
Four of the articles reported norepinephrine requirements in patients treated with Cytosorb as well as in a control cohort not treated with Cytosorb (Table 1).
Table 1. Studies with Cytosorb and control cohorts.
| Study |
Design |
Indication |
Cytosorb, n |
Control, n |
Total |
| Mehta et al. [77] |
Observational |
Aortic surgery |
8 |
8 |
16 |
| Hawchar et al. [64] |
Randomized |
Septic shock |
10 |
10 |
20 |
| Akil et al. [75] |
Observational |
Septic shock |
13 |
7 |
20 |
| Rugg et al. [79] |
Observational |
Septic shock |
42 |
42 |
84 |
| Total |
- |
- |
73 |
67 |
140 |
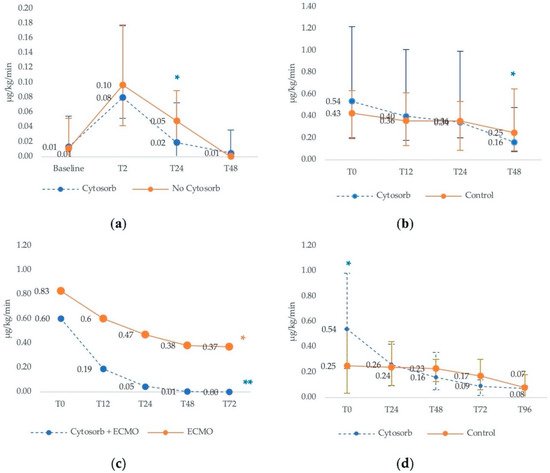
Mehta et al. [
77] compared outcomes between patients undergoing aortic surgery with Cytosorb installed in the cardiopulmonary bypass circuit with patients undergoing conventional surgery without Cytosorb adsorber. At baseline, after the induction of anesthesia, there was no difference in the median dosage of norepinephrine in the Cytosorb or control groups, and vasopressor requirements remained similar at 2 h after discontinuation of CPB (
Figure 3a). However, by 24 h after surgery, the median need for vasopressor dose was significantly lower in the Cytosorb group compared to controls. After 48 h, all patients were either weaned off or only had minimal vasopressor requirements.
Figure 3. Median vasopressor therapy requirements in Cytosorb and control cohorts. (
a) Median vasopressor therapy requirements in aortic surgery patients. Based on Mehta et al. [
77]. *
p < 0.05 for NE dose of Cytosorb vs. no Cytosorb at T24. (
b) Median vasopressor therapy requirements in septic patients. Based on Hawchar et al. [
64]. T
0 is measured right after inclusion (control) or start of hemoadsorption. T
12, T
24 and T
48 were measured 12, 24 and 48 h later. *
p < 0.05 vs. T
0 in the Cytosorb group. (
c) Mean vasopressor therapy requirements in patient with pneumonia-derived sepsis. Based on Akil et al. [
29]. Timepoints represent hours after the initial dose administered at the entrance into the ICU. *
p = 0.05 at T
48 and T
72 in the ECMO group. **
p < 0.005 at T
12, T
24, T
48 and T
72 in the Cytosorb group. (
d) Median vasopressor therapy requirements in septic shock patients requiring CRRT. Based on Rugg et al. [
79]. Baseline is defined as the day of Cytosorb mounting in the treatment group. Data are presented as median and interquartile ranges. *
p = 0.014 as compared to baseline. For explanation see text.
The remaining three articles included septic shock patients, and in all of these the use of Cytosorb was associated with a quicker reduction in norepinephrine needs [
64,
75].
In Hawchar et al. [
64], 20 patients with early onset sepsis were randomly assigned to receive either Cytosorb (
n = 10) or standard care (
n = 10). All patients were mechanically ventilated and on hemodynamic monitoring-guided norepinephrine. Although norepinephrine requirements declined in both groups over time, the decline after 48 h was only significant in the Cytosorb group. Specifically, in the Cytosorb group, norepinephrine doses declined at a steady rate and significantly over 48 h (
Figure 3b). In the control group, lesser and slower declines in norepinephrine requirements over time were observed, with the overall trend not being significant. The mean change (Δ) in norepineprine requirements between baseline and 48 h was also significantly greater in the Cytosorb group (0.67 μg/kg/min vs. 0.10 μg/kg/min;
p = 0.047).
In another study investigating the role of Cytosorb in septic patients, Akil and colleagues [
75] prospectively compared 13 patients who developed acute respiratory distress syndrome (ARDS) from pneumonia-derived sepsis and were treated with veno-venous extracorporeal membrane oxygenation (ECMO) plus Cytosorb to a historical cohort of 7 pulmonary sepsis patients treated with ECMO alone. At the time of admission to the ICU, norepinephrine dose was slightly lower in the Cytosorb group compared to controls, but both patient groups required high vasopressor support (
Figure 3c).
Although reductions in vasopressor requirements were observed in both groups, the decline in the hemoadsorption group was more rapid and more pronounced. Specifically, median norepinephrine dose was significantly reduced after 12, 24 and 48 h of treatment compared to the initial dose required at the time of admission in the ICU. After 72 h, none of the Cytosorb patients required norepinephrine, while in the control group, high norepinephrine doses were still needed after 12, 24, 48 and 72 h after admission to the ICU (Figure 3c).
Finally, in a retrospective study of Cytosorb in septic shock patients, Rugg and colleagues [
79] compared the catecholamine requirements of 42 septic shock patients treated with Cytosorb and continuous renal replacement therapy (CRRT) to a genetic-matched control of 42 patients receiving CRRT alone. Baseline catecholamine requirements were significantly lower in the control group compared with the Cytosorb group, suggesting that the latter patients were sicker. However, within 24 h of Cytosorb initiation, norepinephrine doses were halved, while no change was seen in the control group. By 96 h, the vasopressor requirements were similar in both groups, but the overall reduction in patients not receiving Cytosorb therapy was modest and very slow (
Figure 3d).
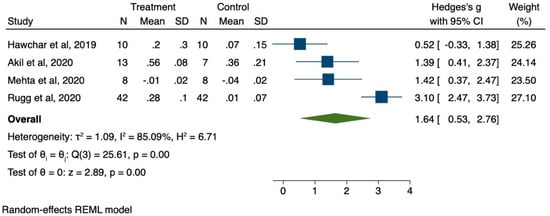
2.2. Pooled Analysis
We pooled together the results from the four studies with control cohorts to estimate the effect size of the benefit associated with the use of Cytosorb treatment, expressed in terms of reduced need of vasopressor support at 24 h.
The meta-analysis was run on STATA 16 [
82] using the meta command. The effect size was estimated as the standardized mean difference of the relative reduction in the need for vasopressor support from baseline to 24 h. We used Hedge’s g statistical method, which is preferred for estimates on small samples. The effect size according to Hedge’s g is interpreted following a rule of thumb:
-
Small effect = 0.2;
-
Medium effect = 0.5;
-
Large effect = 0.8.
Figure 4 below summarizes the results of the pooled analysis.
Figure 4. Forest plot for efficacy of CS therapy to reduce NE requirements at 24 h.
The pooled effect size at 24 h was large and statistically significant. Despite the consistency in the direction of the treatment effect, the I2 statistic suggests a high degree of heterogeneity in the size of the treatment effect between the studies.
3. Insights into Cytosorb
Despite advancements in critical care medicine, critical illness and hyperinflammatory shock are still characterized by high mortality all over the world, and create a huge demand for advancements in critical care. The available therapeutic strategies aim at supporting the impaired organ function and at re-establishing hemodynamic stability.
Fluid resuscitation and vasopressor therapies represent important first-line options in these patients. However, both excessive fluid administration and high doses or prolonged usage of vasopressors can lead to potential patient harm [
19]. First, fluid overload can trigger respiratory and cardiac strain, both manifesting in worsening hypoxemia and myocardial ischemia. For this reason, fluid “
de-resuscitation” should be aggressively pursued after hemodynamic stabilization is established. Second, vasopressors may cause vasoconstriction in the arterioles, and thus decrease microvascular perfusion, an effect demonstrated in both healthy subjects [
83] and critically ill patients [
84,
85]. The potentially serious adverse effects of high-dose vasopressor administration include digital ischemia, tachyarrhythmias, facilitation of bacterial growth, and compromised host resistance to bacteria [
86] (
Table 2).
Table 2. Studies with CytoSorb and control cohorts.
Importantly, several retrospective studies have concluded that the prolonged use of high-dose norepinephrine is associated with poor outcomes, and is also a strong predictor of death [
87,
88]. Although one could argue that high-dose vasopressors are simply a surrogate marker of disease severity in these patients, these results suggest that reducing the need for vasopressor support in terms of both time and dosage could be beneficial for patients.
These findings emphasize the importance of shock reversal with concomitant “
de-catecholamisation”, to be performed as quickly as possible [
89,
90,
91,
92].
Cytosorb is a European CE-marked therapy able to adsorb and thus remove cytokines from the blood, attenuating the devastating effects of the cytokine storm. In this review, we have found a significant decline in vasopressor support requirements after treatment with hemoadsorption in the critically ill. In addition, based on a pooled analysis of studies including data on control cohorts, we have found evidence of a large treatment effect of the therapy at 24 h from baseline. This finding was characterized by large heterogeneity, indicating variability among studies.
This entry is adapted from the peer-reviewed paper 10.3390/biomedicines9070768