Primary malignant cardiac tumors are rare, with a prevalence of about 0.01% among all cancer histotypes. At least 60% of them are primary soft tissue sarcomas of the heart (pSTS-h) that represent almost 1% of all STSs. The cardiac site of origin is the best way to classify pSTS-h as it is directly linked to the surgical approach for cancer removal. Indeed, histological differentiation should integrate the classification to provide insights into prognosis and survival expectancy of the patients. The prognosis of pSTS-h is severe and mostly influenced by the primary localization of the tumor, the difficulty in achieving complete surgical and pharmacological eradication, and the aggressive biological features of malignant cells.
1. Introduction
Primary soft tissue sarcomas of the heart (pSTS-h) are rare and represent an interesting chapter in cardio-oncology [
1]. Autoptic data revealed a prevalence of pSTS-h ranging from 0.001% to 0.03% [
2,
3,
4]. The pSTS-h are difficult to be diagnosed, and retrospective data exploring 7,384,580 cases of cancer included in the Surveillance, Epidemiology and End Results (SEER)-18 database from the United States National Cancer Institute from 1973 to 2015 revealed about a 0.01% prevalence [
5]. Other epidemiologic investigations [
1], however, outlined a 10.8% prevalence of pSTS-h among 8800 patients with primary cardiac tumors. Despite their rarity, primary heart cancers show high mortality with almost 15% of deaths [
1], and STS is the most common histotype [
5], which includes at least 1% of all sarcomas [
6]. The prognosis is severe and mostly influenced by the localization of the tumor, its biological aggressiveness, and the difficulty in obtaining surgical radicality, whereas chemotherapy exerts a modest role [
7]. The one-year overall survival of pSTS-h is 25% [
8], whereas angiosarcoma, leiomyosarcoma, and poorly differentiated sarcoma are the most aggressive variants, showing worse prognosis and risk of death in more than 70% of patients [
8]. In this context, radical surgery, chemotherapy, and radiotherapy may improve both progression-free survival (PFS) and overall survival (OS) [
8], although the majority of data have been collected from single-center experience or retrospective analyses.
2. Classification, Pathological Features, and Molecular Features
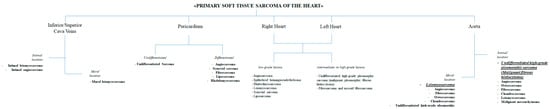
The classification of pSTS-h is still under debate. The rarity of the disease and the lack of tailored clinical studies render the evaluation of rare histotypes less comprehensive. The pSTS-h classification is based on the cardiac site of origin, such as those arising from the right, left chamber, pericardium, or cava vein and aorta [
9,
10,
11,
12,
13]. The early detection of the sarcoma mass is critical for planning the best surgical approach, and thus the proposal to combine surgery and histologic evaluation (
Figure 1), accordingly with the 5th Edition of the World Health Organization (WHO) Classification, is a relevant strategy for planning the best treatment of pSTS-h.
Figure 1. Classification of the primary soft tissue sarcoma of the heart. The figure gathers the combination of the surgical and histologic approach to the classification of these neoplasms. Cardiac sarcomas are differentiated according to the site of origin into cardiac chambers and great arteries/veins; then, sarcomas are identified in agreement with their own histologic nature.
Briefly, the STSs from the great vessels (aorta/great veins) are differentiated into (i) mural and (ii) intimal in relation to their development from the mid-layer/adventitia of the vascular wall or the intima, respectively [
9,
12]. Moreover, lesions arising from the intima usually invade the lumen of the vessels, while mural pSTSs tend to outer extension. Furthermore, intimal STSs often show poorly differentiated histology that negatively impacts outcomes in the majority of patients [
9,
12]. On the basis of the grade of differentiation (
Figure 1), one can subdivide the pSTSs of the right and left chambers of the heart into low, intermediate, and high grades.
The difficulties in diagnosis and the aggressiveness of these mass induce the outer cells to widely disseminate to different organs. Lungs are the main site for metastases from pSTS-h, followed by lymph nodes, bones, liver, and the central nervous system [
14]. This is in agreement with other forms of sarcomas arising from tissues other than the heart: the main final destination of the metastasis still remains the lungs, but all the organs and tissues may become the target of disseminated cells of sarcoma.
2.1. Angiosarcoma
Angiosarcoma (A-SRC) is the most frequent histologic variant characterized by an incidence of 7.3–8.5% among all tumors [
3,
15,
16]. Epidemiologic data from the Japanese Circulation Society and the Japanese Association for Thoracic Surgery reported incidences of 8.2% and 9.5% during the last decade [
15,
17]. A-SRCs preferentially develop from the endothelial layer of the cardiac chambers [
17,
18,
19], and Leduc et al. [
20] outlined that they are most likely to arise from the right atrium followed by epicardium and right ventricle. They may grow up to 10 cm in diameter, often infiltrating the borders, thus resulting in difficulty in being distinguished from the cardiac wall [
20]. Accordingly with morphology and invasiveness, A-SRCs may develop from the cardiac chambers as large, bleeding, or necrotic lesions showing a high propensity to infiltrate the pericardium and surrounding structures [
18,
21]. The cardiac A-SRCs can effectively invade the cardiac chambers, thus provoking obstruction and heart failure as well as clinical complications related to the compression of the great veins or invasion of the pericardium [
4,
22]. Malignant cells from A-SRCs usually show pleiomorphic nuclei and high mitotic count [
23]. Spindle-cell is the most common histotype, although epithelioid cells [
20] showing a focal distribution of cytokeratins are frequently found [
20]. Indeed, vascular markers, such as ERG (erythroblast transformation-specific (ETS)-related gene), a member of the ETS family of transcription factors such as both the avian v-ets erythroblastosis virus E26 oncogene homolog and [
24] the friend leukemia virus integration-1 (FLI-1), as well as CD31 frequently characterize A-SRC of the heart [
20,
23]. The molecular cytogenetic landscape does not foster a definite and specific diagnosis [
20]. However, trisomy of chromosomes 4, 8, 11, 17, and 20 have been previously demonstrated in parallel to the amplification in
MYC,
PIK3C2B/MDM4, and
KIT [
20].
2.2. Undifferentiated High-Grade Pleomorphic Sarcoma
Undifferentiated high-grade pleomorphic cardiac sarcomas (UHGPC-SRCSs, also named as malignant fibrous histiocytomas) are the second pSTS-h (Table 1).
Table 1. Mean incidence in primary cardiac sarcomas among all cardiac tumors according to international registries. Data were from the Armed Forces Institute of Pathology (AIFP), the Japanese Circulation Society (JCS), and the Japanese Association for Thoracic Surgery (JATS) registries [
3,
17,
18,
19]. The French Sarcoma Group registry reported the percentage of patients each kind of sarcoma among all of the primary cardiac sarcomas (PCSs) collected by the group [
8].
| Type of Sarcoma |
AFIP Registry
Period: <1974–1993 |
JCS Registry
Period: 1999–2010 |
JATS Registry
Period: 1999–2010 |
French Sarcoma Group
Period: 1977–2010
% among PCSs |
| Angiosarcoma |
7.3–8.5% |
9.5% |
8.2% |
32.3% |
| Undifferentiated high grade pleomorphic sarcoma |
4.1–8.5%% |
3.3% |
4.3% |
36.3% |
| Leiomyosarcoma |
0.19–3.1% |
1.9% |
2.2% |
12.9% |
| Rhabdomyosarcoma |
1.6–4.9% |
0.8% |
0.45% |
18.6% |
| Synovial sarcoma |
0.19–1.4% |
0.8% |
0.9% |
| Liposarcoma |
0.19–0.5% |
1.1% |
0.9% |
| Fibrosarcoma and myxoid fibrosarcoma |
2.3–3.2% |
0.3% |
0% |
| Osteosarcoma/Chondrosarcoma |
0.94–4.7% |
0–0.8% |
0.45–1.3% |
Among the pSTS-h cases from the French experience, 36% were UHGPC-SRCSs [
8]. They deeply invade the myocardium and surrounding structures, often generating large necrotic areas. It can appear as a sessile or pedunculated mass [
19]. The cytology is characterized by the presence of different cells with spindle and epithelioid or giant features. Such cells often display a higher number of mitoses and nuclear polymorphism, while others undergo late apoptosis and necrosis. Moreover, UHGPC-SRCSs are formed by poorly differentiated mesenchymal or chondromatous phenotypes that confer a high degree of malignancy [
7]. The heterogeneous features of these neoplasms make the definite diagnosis difficult [
25]. Indeed, the classification of UHGPC-SRCSs requires immunohistochemistry, and vimentin expression is considered reliable for this type of pSTS-h [
8], as well as α-smooth muscle actin and cytokeratins [
8]. In addition, chromosomal defects of
AKT2 and
RUNX2, mutation of
PDGFRB, and a higher number of chromosomal aberrations have been described in these rare variants of SRCs [
26].
2.3. Rhabdomyosarcoma
The rhabdomyosarcoma of the heart (RMS) mostly occurs in children and adolescents, showing the highest incidence in 15-year-olds [
22]. In adulthood, the Armed Forces Institute of Pathology (AFIP) registry revealed an incidence ranging from 1.6% to 4.9%, although the identification of such neoplasms after surgical excision was 0.07%, the incidence ratio being higher in children < 16 years old (5.4%) [
3,
15,
16]. Indeed, the Japanese experience outlined the lowest incidence, ranging from 0.45% to 0.8% [
15,
17]. As this sarcoma seems to originate from the degeneration of embryonic cells, its frequency in younger age [
7,
22] is, at least in part, explained. There is no specific cardiac location for RMS, although they may often arise from the myocardium of the ventricle—the left in particular—but rarely from the atria [
7,
27]. The mass may develop throughout the heart, therein involving the cardiac valves and/or the pericardium, where it may appear as a nodule [
21,
22]. Macroscopically, RMS arises from the myocardium as large, irregular, infiltrative masses, also characterized by necrotic areas [
21], while the infiltration of the pericardium may lead to hemorrhagic infiltration [
23]. Microscopically, RMS is usually formed by cells that resemble the rhabdomyoblasts with pleiomorphic nuclei frequently resulting in positive to α-smooth muscle actin, desmin, myogenin, and vimentin [
7].
2.4. Leiomyosarcoma
Cardiac leiomyosarcoma (LMS) is rare, and the French experience reported a 12.9% prevalence [
8]. Most LMSs are located in the left atrium [
19]. Indeed, these sarcomas promptly disseminate to pulmonary veins or invade mitral leaflets [
28]. This can account for the symptoms of patients, while the survival rate remains poor [
29]. The histological pattern can reveal the presence of abnormal smooth muscle cells, which appear as spindle cells with blunt-ended or “cigar-shaped” nuclei [
7,
28]. Necrotic and pleomorphic areas can often be detected [
7,
28]. As the cardiac LMSs are neoplasms arising from the smooth muscle cells and still keep their differentiation status, histology can point out positivity to desmin, α-smooth muscle actin, and myogenin, whereas they rarely show positive and focal stain for cytokeratins [
7,
30].
2.5. Synovial Sarcoma
The incidence of cardiac synovial sarcomas is truly rare (
Table 1). Most of them occur in individuals younger than 20–40 years old [
31]. Cardiac synovial sarcoma usually develops in the atria and pericardium [
7,
28,
32]. The right atrium is the most common site, while the pericardial localization requires differentiation from primary mesothelioma [
7]. The invasiveness of the growing mass leads to the fast invasion of other cardiac chambers and great dimensions of the malignant neoplasm that can be 10–15 cm in diameter [
32]. Microscopic evaluation often revealed both epithelial and spindle cells differently mixed within the malignant tissue [
7,
28,
32]. The presence of these cells or the identification of spindle cells accounts for the biphasic or monophasic variant, respectively [
28,
32]. The cytology outlines the presence of cells with modest cytoplasm and nuclei bearing fine chromatin [
32]. Mitoses can also be detected, while necrotic areas can predominate in more undifferentiated forms [
32]. The identification of hemangiopericytoma-like vascular structures is a distinctive feature for cardiac synovial sarcomas compared to those arising from other sites [
33,
34]. The genetic background of cardiac synovial sarcomas pointed out the possibility of translocation of chromosome X to chromosome 18 (p21.2; q11.2), which promotes the fusion between
SYT on chromosome 18 and
SSX1 or
SSX2 on chromosome X [
7]. Indeed, cytokeratins and vimentin can be detected, while rarely malignant cells express epithelial membrane antigen (EMA) and/or α-smooth muscle actin [
7].
3. The Therapeutic Options
The rarity of the pSTS-h makes challenging the development of a standardized protocols for a definite treatment. Surgery, chemotherapy, and radiotherapy should be integrated to improve the prognosis.
3.1. Surgical Treatment
In the early stage, pSTS-h surgical removal is suitable. After biopsy confirmation for histological characterization, cytoreductive chemotherapy with or without radiotherapy can be optioned. It has been estimated that radical surgery can promote a 51% effective reduction in the overall risk for mortality [
59], while cumulative survival rate equal to 72% at 5 years and 59% at 15 years follow-up were in patients treated for cardiac neoplasms, irrespective of the histotypes [
60]. No standard techniques can be described due to the rarity of the different histotypes and sites of origin. Orthotopic heart autotransplantation (OHA) has been considered as a possible surgical option [
61]—it consists of cardiac explantation, ex vivo tumor resection, reconstruction, and reimplantation [
62]. Reardon et al. firstly performed OHA in a large sarcoma of the left atrium and collected a case series on 11 patients [
61,
63]. Indeed, the literature offers little further data about the application and the outcomes related to this surgical technique [
64,
65]. Kim et al. [
58] evaluated the influence of the site of origin on surgery outcome. They observed an overall 5-year survival rate equal to 17% in patients with pSTS-h involving right cardiac chambers, which was extremely lower as compared to the survival rate from those of the left cardiac chambers [
66]. Ramlawi et al. [
67] reported a higher prevalence in death between 1 and 6 months after surgery for right cardiac chamber pSTS-h while demonstrating increased prevalence in deaths within 1 month or between 6 and 12 months after surgical removal of left cardiac chamber pSTS-h.
Nevertheless, surgical margins remain the mainstay in understanding the outcome related to surgery—free-cancer cell margins increased the 5-year survival rate of patients with right sarcoma as compared to R1 and/or R2 borders [
66]. R1 and/or R2 resections deserve more aggressive interventions and multimodality approaches with chemo- and radiotherapy [
68], and heart transplantation is to be considered in selected cases [
69]. Moreover, the histotype and the differentiation degree influence the survival—less differentiated neoplasia entails a higher mortality rate and/or recurrence of the disease [
70]. Therefore, non-metastatic and localized pSTS-h should undergo complete surgical removal to prolong life expectancy.
3.2. Radiotherapy
The radiotherapy (RT) in patients with pSTS-h is questionable due to the risks related to its application. Damages to cardiac muscular cells might be extremely deleterious, thus forcing physicians to adopt reduced or fractioned doses [
11], but this may limit the efficacy of the treatment [
71]. In the literature, a few case reports are described. Fatima et al. [
72] observed a better survival rate in patients who underwent postoperative radiotherapy at 40 to 50 Gy than surgery alone. A retrospective analysis on 168 primary cardiac angiosarcomas selected from the National Cancer Institute’s SEER database confirmed data about outcomes associated with RT. The mean survival rate was higher in patients who underwent radiotherapy (63% higher than controls at univariate analysis) [
73].
In the preoperative setting, Thariat et al. considered 124 patients from the French Sarcoma Group, who received 45 Gy in 1.8 Gy per fraction and further implemented with 14 Gy in seven fractions within the residual margins of the lesion, with a result of 15-month mean survival, although six patients developed metastases and/or loco-regional recurrence [
71]. Similar results derived from the retrospective analysis by Isambert et al. who observed a 67% improvement in overall survival rate when radiotherapy was considered as a therapeutic option in pSTS-h [
8]. Nevertheless, other studies and Aboud et al. did not find an effective role of radiotherapy in ameliorating the outcomes of their patients [
29,
74].
3.3. Chemotherapy
The highly malignant nature of pSTS-h requires evaluation of adjuvant chemotherapy with or without radiotherapy to reduce the cancer mass to plan a definite surgical approach, and, secondly, to prevent the occurrence of metastases [
78,
79]. Dedicated protocols for chemotherapy in pSTS-h are still a matter of debate due to the paucity of data in the literature and the rarity of these types of cancers. The first-line therapy for pSTS-h is based on Adriamycin at a dose of 75 mg/m
2 administered as a continuous intravenous infusion over 3 days, and ifosfamide at a dose of 10 g/m
2 divided over 4 to 5 days [
80,
81,
82]. Adequate hydration therapy should be managed to prevent kidney toxicity, while neurotoxicity related to ifosfamide might be prevented by promoting alkalinization and albumin infusion [
82].
The second-line regimen considers a combination of gemcitabine plus docetaxel [
81,
82]. Generally, gemcitabine might be given on days 1 and 8 at 900 mg/mq, and docetaxel at 100 mg/mq, although a reduced dose may be considered to reduce side effects [
82]. Fluid retention due to docetaxel might effectively influence cardiovascular hemodynamics, while gemcitabine should be slowly administrated to allow its phosphorylation for DNA inclusion [
82]. Although further chemotherapeutic agents might theoretically be applied in pSTS-h, no randomized controlled trial/studies have been performed, and thus no definite indications may be provided. Frezza et al. [
83] retrospectively evaluated the efficacy and safety of chemotherapies (i.e., anthracycline, gemcitabine, pazopanib) in 72 patients with intimal sarcoma. The anthracycline group did not present any cardiac toxicity event, with a real-world overall response rate (rwORR) equal to 38% [
83]. Gemcitabine was mostly adopted as a second-line treatment (77% of cases), demonstrating rwORR equal to 8% [
83]. The same results (rwORR = 8%) occurred for pazopanib—a tyrosine kinase inhibitor (TKI) with anti-angiogenetic properties—which was considered as a further line therapy in advanced diseases [
83].
Temozolomide, dacarbazine, vinorelbine, and liposomal doxorubicin are no longer the first choice in the treatment of advanced or metastatic disease because of their high toxicity profile [
84]. Indeed, trabectedin might be adopted as second-line therapy in liposarcoma (LPS) and leiomyosarcoma (LMS) after weighting the risk for sever bone marrow depression and gastrointestinal symptoms.
A phase-III, multicenter, clinical trial compared trabectedin (1.5 mg/mq 24-h i.v.) to dacarbazine (1 g/mq 20–120-min i.v.) in metastatic patients with LMS o LPS after progression to anthracyclines. Patients on trabectedin demonstrated amelioration in PFS (4.2 versus 1.5 months) and 13% reduction in median OS [
85]. Similar results were observed from Schöffski et al. [
86] who considered eribulin (1.4 mg/mq i.v. on days 1 and 8) on top of anthracycline therapy in patients with LPS or LMS.
Comprehensive management of patients with pSTS-h might consider adequate chemotherapy before surgical excision—in the ESPERO trial (Safety and Efficacy of a Novel Radical Tumor Resection Procedure used in Conjunction with Neoadjuvant Chemotherapy to treat Malignant Primary Right Heart Cardiac Tumors), 33% (8 out of 24) of patients treated with doxorubicin–ifosfamide for 4–6 cycles achieved negative margins with 80% survival at 40 months. Abu Saleh et al. described an improved overall survival and high degree in R0 resections in patients who underwent neoadjuvant chemotherapy before surgery (32 of 44 patients in the study), with an estimated median survival of 20 months compared to 9 months in those without pre-operative systemic therapy [
80]. Moreover, upfront surgery followed by adjuvant therapy may provide favorable outcomes in patients with pSTS-h [
80,
87]. Llombart-Cussac et al. [
88] pointed out an overall two-year survival rate equal to 26% in pSTS-h treated with both surgery and post-operative doxorubicin, especially in cardiac angiosarcoma. Hendriksen et al. [
89] observed a positive effect of chemotherapy on postoperative 2-year survival after surgical intervention.
This entry is adapted from the peer-reviewed paper 10.3390/biomedicines9070774