Silk derived from the silkworm is known for its excellent biological and mechanical properties. It has been used in various fields as a biomaterial, especially in bone tissue engineering scaffolding. Recently, silk protein-based biomaterial has been used as a barrier membrane scaffolding for guided bone regeneration (GBR). GBR promotes bone regeneration in bone defect areas using special barrier membranes. GBR membranes should have biocompatibility, biodegradability, cell occlusion, the mechanical properties of space-making, and easy clinical handling. Silk-based biomaterial has excellent biologic and mechanical properties that make it a good candidate to be used as GBR membranes.
1. Introduction
Guided bone regeneration (GBR) promotes new bone formation in bone defects using the barrier membrane [
1]. The barrier membrane prevents the infiltration of the epithelial cells and the down growth of the connective tissue in the defect area [
2]. It secures the space for the migration of osteoblasts and osteogenic cells and for new bone to grow in [
2]. The barrier membrane must have several beneficial properties, such as biocompatibility, biodegradability without immune reaction, cell occlusion to prevent epithelial cell migration, the mechanical property for space making, tissue integration, and easy clinical handling [
3]. However, there is no ideal barrier membrane that satisfies all of these properties. Generally, two types of the membrane have been used for GBR: resorbable and non-resorbable membranes [
4].
Non-resorbable membranes, such as titanium mesh and titanium-reinforced expanded-polytetrafluoroethylene (e-PTFE), have high biocompatibility, mechanical properties, and stability [
5]. They can stably maintain the form of grafted bone material and secure the space for bone growth [
6]. The e-PTFE membrane effectively occludes the soft tissue cell invasion [
7]. Even though non-resorbable membranes have had successful clinical outcomes in GBR, they can be more easily exposed in the oral cavity and lead to wound dehiscence compared with resorbable membranes [
8], causing bacterial contamination on the membrane and potentially leading to the failure of the bone graft. Therefore, when membrane exposure occurs, it should be removed immediately [
9]. Resorbable membranes have been widely used in clinical practice due to their advantages with similar results as the non-resorbable membranes [
10]. As the main source of the resorbable membrane, collagen has good biocompatibility, low risk of membrane exposure and donor site infection, and no need of a secondary surgery for removal [
11]. However, collagen membranes have weak mechanical properties, rapid biodegradation, and lower space-making ability compared to non-resorbable membranes [
10]. To overcome this problem, cross-linking membranes have been manufactured, but the agent used in the cross-linking can be cytotoxic during degradation [
12,
13].
Silk derived from the silkworm
Bombyx mori (B. mori) is a natural biopolymer [
14]. Silk is mainly composed of fibroin and sericin [
14]. Silk fibroin (SF) has been used as a biomaterial after the removal of sericin by the degumming process [
15]. Several types of SF material have been used for bone tissue engineering scaffolding, such as sponge, film, and hydrogel forms [
16]. SF has excellent biocompatibility, biodegradation, oxygen and water permeability, and tissue integration [
16]. Recently, the application of silk protein-based biomaterial for the GBR membrane has been reported [
17,
18]. SF membranes have good osteogenic cell adhesion and induce new bone formation [
17]. Although SF has excellent biological benefits as GBR membranes, it has weak mechanical properties and is difficult to handle [
19]. The silk mat from cocoons, which is not the result of the degumming process, shows excellent mechanical properties [
20]. This silk mat can be separated in different layers by eco-friendly methods [
20,
21]. As a GBR membrane, it shows excellent tensile strength and comparable new bone regeneration in vivo [
20,
22].
The clinical indication of the GBR procedure has been increased in the maxillofacial bone region [
23]. GBR membranes are applied to the areas of bone defect after cyst and tumor excision, tooth extraction, and deficient alveolar bone for implant installation [
11,
24]. However, commercially available GBR membranes have limitations according to their material, properties, and high prices [
25]. The ideal GBR membrane has biological and mechanical properties, easy handling, and reasonable pricing [
26]. Previously, various forms of silk protein-based membrane have been introduced for use in GBR [
19]. Silk protein-based membranes have excellent osteogenic and mechanical properties and show potential as GBR membranes [
17,
21].
2. Silk Material Proteins
Silk, as a protein polymer containing repetitive amino acids, is spun into fiber from the secretory gland of Lepidoptera larvae, such as silkworms, spiders, bees, and flies [
27]. The composition and structure of silk differs depending on the species [
28]. Silk derived from silkworms has been popularly used in the textile industry for centuries and in biomedical suture material for decades due to its excellent mechanical properties and biocompatibility [
28]. Silk derived from silkworms consists of two major proteins, fibroin (72–81%) and sericin (19–38%) [
14]. Both proteins contain the same 18 amino acids, including glycine, alanine, and serine in different ratios [
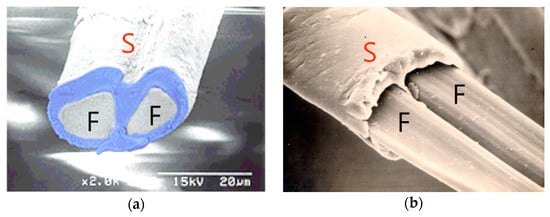
14]. Fibroin composes the core of silk filament, and sericin coats the fibroin fiber (). Sericin is a glue-like protein that makes two fibroin fibers bind together [
29]. Sericin is a water-soluble protein, and generally, it is removed by the thermochemical treatment known as the degumming process [
15]. Silk-based biomaterial has been used as a suture material for wound treatment, and recently, it has been widely used as the major component of biomaterials, including bone tissue scaffolding, wound dressing materials, drug delivery, and vascular patches [
27,
30]. Silk material has suitable properties for use as bone scaffolding material, and it can be easily obtained and processed in various forms of scaffolding [
29].
Figure 1. Scanning electron microscopic view of cocoon fiber. (a) The silk mat is composed of interconnecting strings. Each string has two main fibers (F) and surrounding bonding proteins (S). (b) After the removal of sericin (S), two fibers composed of silk fibroin (F) remain.
3. Silk Fibroin Membrane
SF as natural biomaterial has been studied for use in the scaffolding of bone tissue engineering [
35]. SF has been known as a biocompatible and biodegradable biomaterial [
29]. However, SF is a high-molecule natural polymer and can induce an inflammatory reaction when implanted in the human body. Therefore, low molecular SF power is used as a bone graft scaffold [
56]. Low molecular SF power shows favorable osteogenic cell properties in in vitro studies. It increases the expression of osteogenic genes, including alkaline phosphatase (ALP), collagen type 1, and transforming growth factor-β1, and the ALP activity in MG-63 cells [
56]. In vivo, the low molecular SF power combined with Choukroun platelet-rich fibrin showed rapid bone regeneration compared with the empty defect in a rabbit calvarial defect and a rabbit tibia peri-implant defect [
57,
58].
SF can be manufactured as a membrane-type scaffold for use as a GBR membrane [
59]. GBR membranes should have several properties, such as biocompatibility, mechanical properties for space maintenance, cell occlusion of connective tissue cells, and biodegradability without inflammatory reaction [
10]. SF membranes can be made by an electrospinning and casting technique [
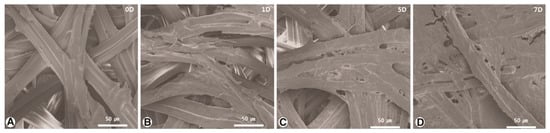
27]. SF membrane has shown cell and tissue compatibility and the increase of osteogenic cell proliferation () [
17]. The electrospinning SF nanofiber membrane increased osteoblast-like cell attachment and proliferation according to the culture period, and the expression of osteocalcin and ALP activity were increased [
38]. SF nanofiber membrane in a rabbit calvarial defect showed significantly increased new bone regeneration compared with the empty defect without inflammatory reaction [
38]. Compared with commercial collagen membranes, SF nanofiber membranes have shown satisfactory mechanical stability and new bone regeneration ability in a rat calvarial defect [
39]. In clinical application, SF nanofiber membranes have shown similar bone regeneration ability compared with polylactic acid/poly(lactic/glycolic) acid (PLA/PLGA) membranes in tooth extraction defects [
60,
61].
Figure 2. Scanning electron microscopy (SEM) images of cell attachment on the surface of silk fibroin (SF) membranes. (
A) SEM image shows the SF membrane surface for day 0; (
B) the cells gradually filled across the fiber texture, covering approximately 10–20% of the SF membrane surface; (
C) at 5 days, the gap between the SF membrane fibers was filled and covered by the cell attachment; (
D) at 7 days, the surface of the SF membrane was nearly filled and covered with cells (reproduced from previous publication by permission) [
17].
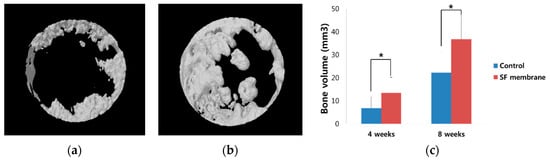
The SF membrane manufactured by the casting technique showed higher new bone regeneration ability than the uncovered defect in a rabbit calvarial defect () [
19], and compared with the collagen membrane, it shows comparable new bone regeneration without inflammatory reaction [
40]. However, the casting SF membrane has weak mechanical properties and is brittle in its dry state [
19]. Despite their low mechanical properties and difficult handling, SF membranes can be suitable barrier membranes for GBR due to their low cost and biocompatibility [
40]. In the previously reported study, the silk-based membranes showed their potential as GBR membranes. They have favorable osteogenic cell compatibility and new bone regeneration ability with low immune reaction.
Figure 3. Micro-computerized tomography (CT) image at 8 weeks after operation [
19]. SF membrane was applied on the rabbit calvarial defect. (
a) Unfilled defect in the control group; (
b) SF membrane group; (
c) bone volume analysis of the micro-CT. New bone formation was significantly higher in the SF membrane group than the control (*
p < 0.05). (“*” means significant difference)
4-hexylresorcinol (4-HR) is natural phenolic compound that has antimicrobial, antioxidant, and antimutagenic activity [
62]. It has been used as a food additive for preventing the enzymatic browning of fruit and seafood [
63]. Medically, it has been used as an antiparasitic and antiseptic agent, and now, it is used as a topical antiseptic ingredient for skin and throat lozenges [
64,
65]. 4-HR has an anticancer effect through the suppression of the transglutaminase and inhibition of the nuclear factor-κB (NF-κB) pathways [
66]. The NF-κB pathway is related to osteoclast differentiation, and the NF-κB pathway inhibitor can impair the osteoclast activation [
67,
68]. As a result, 4-HR can inhibit the osteoclast activation, and it may contribute to new bone regeneration.
Tetracycline (TC) is a broad-spectrum antibiotic that is effective against gram-positive and negative bacteria [
77]. It inhibits the protein synthesis of bacteria and has bacteriostatic activity [
77]. TC has an affinity to the mineralizing tissue of bone and tooth and causes the proliferation of osteoblastic cell [
78]. It decreases the degradation of the collagen matrix and bone resorption and has been used for the treatment of periodontal disease [
79,
80]. Using its antimicrobial and therapeutic activity, TC has been used as a component of the SF membrane for new bone regeneration [
81].
Chitosan is a natural polysaccharide derived from chitin that is known for its excellent biologic properties, including biodegradability, biocompatibility, and antimicrobial activity [
84]. Chitosan has been used in biomedical and pharmaceutical applications, such as in wound healing, drug carriers, and tissue engineering scaffolding [
85]. Chitosan is blended with SF and widely used in the tissue engineering scaffolding of bone and cartilage and skin healing [
86]. Various forms of chitosan-blended SF scaffolds can be manufactured for bone tissue engineering, such as film, nanofiber, and membranes, and it shows good osteogenic properties by increasing osteogenic cell proliferation and gene expression [
84,
87,
88].
4. Silk Mat as GBR Membrane
Silkworm cocoons have a multi-layered structure (), and the silk mat is produced from silkworm cocoons by cutting and peeling off [
20]. As it is produced manually without any chemical treatment, its production is eco-friendly [
20]. As the size of the cocoon is limited, the size of the silk mat is also limited. Because silkworm cocoons have a layered structure, their separation into thin membranes is easy. By manual separation, their thickness can be 0.01–0.2 mm. This silk mat shows good tensile strength in wetting conditions [
20,
22]. Considering the oral environment, high tensile strength in wetting conditions is an advantage.
Figure 4. Silkworm cocoon. (a) After removing the larva, the cocoon has a Rugby ball-like structure; (b) when the cocoon is cut into a rectangular shape, it is easily peeled off as many sheets.
This entry is adapted from the peer-reviewed paper 10.3390/app8081214