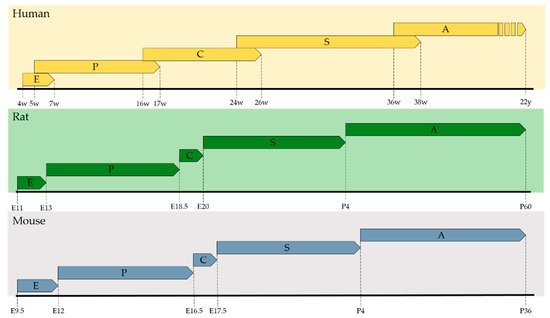
In humans, lung organogenesis initiates with the appearance of an endodermal bud on the ventral side of the anterior foregut around the fourth week of gestation. The endodermal evagination leads to the formation of the two lung buds and trachea, surrounded by mesoderm and a vascular network [
25]. Lung epithelium is endoderm-derived and lines the airways and the alveoli. The conducting airways are generated by a highly regulated dichotomous branching morphogenesis commencing on the 5th week of gestation, giving rise to a complex network with numerous terminal branches. The continuous bifurcation of the epithelial bud tips relies on the close interaction between epithelium and mesenchyme. The mesenchyme at the tips is particularly important since it contains precursor cells that will differentiate into smooth muscle that stabilize the cleft between the newly formed buds. At the same time, diffusible signals act in both compartments, orchestrating lung organogenesis processes [
26,
27,
28]. The alveolar cellular differentiation begins between the 16th and the 24th week of gestation. During this phase, bronchial epithelial cells differentiate into alveolar epithelial cells type 1 (AEC1) and type 2 (AEC2), also known as type 1 and type 2 pneumocytes, respectively. AEC2 act as AEC1 progenitor cells and are responsible for surfactant production, whereas AEC1 are responsible for gas exchange. From the 24th week onwards, tissue projection into the distal airspaces gives rise to structures resembling sacs, the primitive alveoli, lined with AEC1 and AEC2. Although the alveoli are formed at birth, their maturation begins approximately five weeks after birth, with the formation of a fine air-blood barrier composed by a thin epithelial sheet, an endothelial layer, and a basement membrane. Even though in the first years of life, the alveolar size remains constant, in adolescence, with the enlargement of the thoracic cage, it increases [
29,
30,
31].
2.1. Embryonic Phase
The respiratory system is specified from the anterior foregut endoderm approximately at embryonic day 9.5 (E9.5) in mouse and around the 4th week of gestation in humans [
30]. Initially, the anterior foregut begins as a sole epithelial tube surrounded by mesoderm. Lung and trachea specification begins with the establishment of a localized expression domain of the transcription factor NKX2.1 (also known as TTF1) in the ventral wall of the anterior foregut [
37]. The expression of
nkx2.1 on the ventral side, distally to the rudimentary trachea, leads to the evagination of the two primary lung buds [
25]. The epithelial outgrowth of the primary buds is supported by diffusible signals from the mesoderm tightly regulated both in time, dosage, and space. Briefly, WNT2 and WNT2b expression specify NKX2.1
+ respiratory endoderm progenitors in the ventral anterior mesoderm that surrounds the anterior foregut endoderm [
38]. The expression of NKX2.1 also depends on BMP signaling activation. Endodermal SHH regulates BMP4 expression in the ventral mesenchyme surrounding the ventral foregut, mainly through the transcription factors FOXF1, GLI1, and GLI3. BMP signaling represses the expression of the transcription factor SOX2 (that promotes esophageal fate), thus enabling NKX2.1 endodermal expression [
39]. After respiratory lineage specification, FGF10 mesodermal expression requires TGFβ inhibition, mediated by RA signaling, to conduct outgrowth and extension of the primary lung buds [
40].
RA signaling machinery is present in the foregut at the beginning of lung organogenesis. At E9.5,
raldh2 is highly and ubiquitously expressed in the anterior foregut, specifically in the mesenchyme neighboring the prospective trachea and lung primordia, suggesting that RA is being synthesized. Moreover, at this gestational age, a high local RAR activation is also detected in all layers of the foregut where trachea and primordial lung are emerging. This expression pattern is consistent with the hypothesis that RA acts on its receptors present in the epithelium in early lung development. At E10,
raldh2 levels are preserved in the tracheal mesenchyme and proximal lung but decrease towards the distal lung. Conversely,
cyp26 is not detected between E9.5–10; consequently, at these stages, RA synthesis is not compensated by its degradation, pointing to a crucial role for RA in the formation of the lung bud primordium. It is worth noting that, as lung morphogenesis proceeds,
cyp26 is progressively expressed, therefore controlling RA levels [
41].
Disruption of RA signaling in
in vitro mouse foregut cultures impairs lung bud initiation [
42]. Likewise,
raldh2−/− knockout mice and dams exposed to severe vitamin A deficiency during gestation display lung agenesis [
43,
44].
In vitro studies revealed that RA induces
fgf10 expression in the foregut mesoderm, where lung initiates, which then activates FGFR2 signaling in the endoderm and induces primary bud morphogenesis [
42]. By further dissecting
raldh2−/− knockout mice, it was uncovered that RARβ mediates
fgf10 induction by RA. Differential activation of RARα and RARβ has opposite effects in
fgf10 mesodermal expression; nonetheless, both receptors are needed for proper lung development [
44]. Furthermore, it has been shown that endogenous RA acts via WNT and TGFβ signaling to control
fgf10 expression. RA downregulates TGFβ activity in the foregut mesoderm, thus allowing local expression of
fgf10, which is crucial for primary lung bud induction [
40]. Conversely, RA facilitates the activation of WNT signaling, crucial for the appearance/maintenance of the respiratory field, by inhibiting the expression of a WNT/β-catenin antagonist (Dickkopf1) [
45]. Hence, an RA-dependent fine-tuned equilibrium of the WNT/TGFβ/FGF10 axis is mandatory to permit both respiratory progenitors’ expansion and lung primordium formation.
RA acts in both endoderm and mesoderm to provide a niche for lung induction by regulating the expression of signals that will induce the lung and the competence to respond. In early somite stages, RA pre-patterns the lateral plate mesoderm and establishes the anterior foregut region that will form the respiratory niche. Subsequently, RA signaling promotes endodermal Hedgehog (HH) expression, which, mediated by mesenchymal GLI transcription factors, is indispensable for
wnt2/2b and
bmp4 expression; subsequently,
wnt2/2b and
bmp4 act on the endoderm to promote
nkx2.1 expression. The RA-HH-WNT signaling cascade that coordinates respiratory lineage specification is conserved between frog, mouse, and human [
46]. Moreover, RA/RAR activity regulates the competence of the endoderm to activate the NKX2.1
+ respiratory program in response to mesodermal WNT and BMP, independently of HH, during early somite stages of development.
Recently, it has been shown that RA signaling has different roles during endoderm organogenesis, acting in a distinct temporal and spatial pattern. In early gastrula stages (mouse E6–7.5), during endoderm formation, RA induces hindgut and pancreatic stages but inhibits foregut fate. Conversely, in early somitogenesis (mouse E7.5–8.5), during endoderm patterning, RA suppresses pharyngeal and promotes respiratory fate in the anterior endoderm. Finally, lung induction (mouse E9.5) relies on the RA/WNT/BMP axis previously described [
46]. However, RA actions are only possible because, during the gastrula stage, WNT/BMP signaling specifies endodermal competence domains and, consequently, how cells respond to signals during the subsequent phases [
47].
2.2. Pseudoglandular Phase
Lung branching morphogenesis occurs during the pseudoglandular phase (E12–16.5 mouse; E13–E18.5 rat; 5–17 weeks, human), and it is characterized by reiterative splitting of the airway epithelium into the surrounding mesenchyme [
48]. The development of new generations of terminal buds contributes to defining the airway conducting system. This process is tightly regulated by a network of signaling cascades that operate via epithelial-mesenchymal interactions [
30]. The RA pathway has been recognized as a critical regulator of pulmonary branching [
4,
41,
49,
50]. In fact, in
rdh10−/− mutants, primary lung bud growth is arrested and branching morphogenesis impaired, thus preventing the formation of the lung [
51]. Likewise,
raldh2−/− mouse embryos display defective growth and branching, resulting in hypoplastic lungs [
43].
RA signaling machinery is dynamically expressed during branching morphogenesis. For instance,
stra6 mouse transcript is present in the mesenchyme surrounding the bronchi [
52]. Conversely, as lung branching initiates,
crbp transcripts are present in both epithelial and mesenchymal compartments, and later its expression is restricted to the mesenchyme [
53]. In the embryonic mouse lung,
raldh2 is expressed along the mesothelium surface at sites of low branching activity. By comparing
fgf10 and
raldh2 expression patterns, it is possible to observe that regions, where
fgf10 is expressed, are low in
raldh2 [
41,
54]. Conversely,
raldh1 mRNA is present in the proximal region of the bronchi [
41,
49], while
raldh3 is weakly expressed in the epithelium of the main bronchus [
16]. Importantly, RA bioavailability must be balanced to avoid detrimental concentrations. As secondary buds start to emerge,
cyp26 expression displays a proximal-distal epithelial gradient with high expression at distal sites. In the mesenchymal compartment,
cyp26 is present between the secondary buds contributing to the regulation of RA levels in this region [
41].
Retinoic acid signaling response is, ultimately, transduced through RAR and RXR nuclear receptors that recognize RARE sequences in the promoter region of RA-target genes. The importance of RAR is particularly evident in
rarαβ2 mouse mutants, which exhibit lung agenesis and hypoplasia due to the absence of left lung budding and altered branching morphogenesis [
55]. In the developing lung,
rarα1 and
rarα2 are ubiquitously expressed [
49,
56], whereas
rarβ expression is restricted to the proximal bronchi epithelium and the proximal subepithelial and subpleural mesenchyme [
41,
49,
53]. In opposition,
rarγ transcripts are faintly and ubiquitously expressed in the embryonic lung; indeed, RARγ knockouts do not affect lung branching [
41,
49,
53,
56,
57,
58]. Throughout branching, RARE-lacZ reporter activity is detected in the proximal bronchial region with a pattern that strongly overlaps
rarβ expression. Moreover, RARE-lacZ lacks from both the distal bud epithelium and the mesenchymal compartment [
41]. Furthermore, RXR can be sequestered by Chicken Ovalbumin upstream promoter-transcription factors (COUP-TFs), resulting in RA signaling inhibition.
coup-tfII expression is found in the lung mesenchyme, particularly higher in the mesenchyme between the secondary buds, but absent from the pulmonary epithelium [
41]. Recently, RA signaling was characterized in the embryonic chicken lung [
50]. For instance,
stra6 is expressed in the periepithelial mesenchyme surrounding the epithelium as it occurs in the mouse lung [
50,
52].
raldh2,
raldh3,
cyp26a1, and
rarα expression patterns are comparable to their mammalian counterparts. Curiously,
rarβ has a stage-dependent expression that is present in the proximal region of the mesenchymal compartment [
50]. It is worth mentioning that while in the mammalian lung RA signaling members are distributed between the mesenchymal and epithelial compartments, in the chick lung, all members seem to be restricted to the mesenchyme [
50]. Nonetheless, transcripts like
stra6 and
raldh2 display highly conserved expression patterns. Moreover, the complementary expression pattern between
raldh2 and
fgf10 is conserved, with
raldh2 being expressed in the ventral region, and
fgf10 in the dorsal pulmonary region [
50,
59].
RA signaling must be finely tuned so that mammalian lung branching morphogenesis may occur. In the mesenchymal compartment, RA is produced in the mesothelial region, at low branching sites, by RALDH2. Conversely, RA synthesis is regulated by CYP26 and COUP-TFs in the mesenchyme between the secondary buds [
41]. A gradient of RA is produced from the pleura to the periepithelial mesenchyme that surrounds the distal region of the growing bud. RA availability regulates
fgf10 that is typically expressed in the mesenchyme surrounding the distal bud tips [
41,
54]; for this reason,
raldh2−/− mouse embryos phenotype is rescued by RA and FGF10 supplementation [
43]. Concurrently, in the epithelial compartment, RA is produced in the proximal bronchi by RALDH1 [
41,
49] and may act through RARβ, which is detected in the same region [
41,
49,
53]. RA epithelial levels are regulated by CYP26, which displays a gradient from the distal to the proximal region of the epithelial bronchi [
41]. Intriguingly,
stra6 expression in the periepithelial mesenchyme, surrounding the epithelial bronchi, may play a role in retinol trafficking between epithelium and mesenchyme [
52].
The role of RA signaling during pulmonary branching was uncovered by performing RA stimulation/inhibition studies. Mouse lung explants exposed to RA display an increase in lung branching in a dose-dependent manner [
60]. Furthermore, RA supplementation can increase pulmonary branching in nitrofen-induced hypoplastic lungs, which display decreased RALDH2 activity [
61]. Similarly, rat lung explants treated with exogenous RA exhibit an increase in the number of peripheral airway buds, epithelial perimeter, and the total area of the lung [
62]. Likewise, RA supplementation, in the chicken model, revealed a dose-dependent increase in lung branching [
50]. Furthermore, RA-exposed lung explants can display morphological alterations that resemble a more immature branching configuration; specifically, the formation of typical distal bud-like structures is impaired, promoting a more proximal-like phenotype [
41,
63,
64]. Nevertheless, in some studies, a reduced number of terminal buds is observed in RA-treated lungs [
41,
56,
63,
64].
RA pathway modulation studies revealed a series of feedback control mechanisms underlying pulmonary branching morphogenesis. For instance,
crbpI and
raldh1 expression are susceptible to be modulated by activation/inhibition of the RA cascade [
49,
56]. This feedback loop mechanism may regulate RA synthesis in the proximal epithelial buds [
49]. On the other hand, RA supplementation increases both
rarβ and RARβ but decreases RARα and RARγ [
56,
62].
RA downstream targets are not only signaling machinery components, but also members of other pathways. For instance, RA can directly downregulate
fgf10 expression or indirectly by stimulating the SHH pathway (through increasing
shh expression) and, consequently, decrease
fgf10 transcript levels in the distal region of the lung [
41,
49,
54,
64,
65]. Moreover,
bmp4 is also negatively modulated by RA signaling stimulation [
41]. The interaction between RA, FGF, SHH, and BMP4 is crucial for branching and proximal-distal patterning [
41,
49,
54,
64,
65,
66,
67]. In the proximal epithelium, RA modulates the expression of
foxa2, a known regulator of epithelial differentiation and pulmonary branching [
49,
68]. RA pathway stimulation promotes
tgfβ3 expression in the lobar bronchial mesenchyme, pleura region, and bronchial epithelium [
49], and downregulates
cftr epithelial expression in the lobar bronchial and bronchial epithelium [
49]. In fact, mammalian lung branching morphogenesis can be divided into two RA responsive centers: the distal epithelial region where
shh, and
bmp4 are expressed and interact with
fgf10 mesenchymal expression; and the proximal epithelial region where RA regulates
tgfβ3,
foxa2 and
cftr [
41,
49,
54,
65].
There are other RA downstream targets described in the embryonic mammalian lung, namely
hoxa2,
hoxa5,
hoxb5, and
hoxb6, which are related to patterning. Moreover, RA regulates HOXB5 protein levels, and
hoxa2 and
hoxb6 proximal-distal patterns [
64,
69,
70]. In addition, disruption of the RA pathway results in altered murine smooth muscle phenotype and a consequent increase in the expression of
acta2 and
myh11 [
71]. During chick lung branching, RA supplementation does not affect
sox2 but decreases
sox9 expression (patterning-related genes); however, it affects
sox9 spatial distribution, which is progressively excluded from the distal regions of the lung. Still, the new distal branches do not exhibit proximal appearance [
50,
72,
73]. Furthermore, RA signaling stimulation, of the embryonic chick lung, increases the expression of
rarβ,
hoxb5, and
meis2; alters the spatial distribution of
cyp26a1,
id2,
tgfβ2, and
sox9; and has a very modest effect on
fgf10,
fgfr2, and
sox2. Even though RA machinery is confined to the mesenchymal compartment, it can influence the expression of epithelial genes such as
shh,
sox9, and
fgfr2 [
50]. In the chicken model, RA signaling stimulates early pulmonary branching and contributes to pulmonary branching proximal-distal patterning [
50].
2.5. Alveolar Phase
Alveologenesis or alveolarization is the process by which the gas exchange functional units, the alveoli, are generated. Alveoli formation is mainly a postnatal event, and it is time and species-dependent. For instance, mammals like deer, guinea pigs, or sheep are born with functional alveoli; mother-dependent mammals like mice, rats, and humans are born with primitive alveoli and, so, alveologenesis continues postnatally [
89]. In mouse and rat, alveologenesis occurs entirely in the postnatal period, approximately from P4 to P36 and P4 to P60, respectively [
23,
25,
30]. In humans, part of the alveoli is formed before birth, but their genesis continues postnatally. Alveologenesis is divided into three phases: classical alveolarization (week 36 until ∼3 years), microvascular maturation (week 36 until young adulthood), and continued alveolarization (∼2 years until young adulthood) [
30].
Throughout the canalicular and saccular phases, the terminal tubes are transformed into small saccules separated by the primary septum. During classical alveologenesis, the sacs are subdivided by the ingrowth of secondary septum, the outline of the future alveoli. Myofibroblast progenitors, endothelial cells, fibroblasts, and lipofibroblasts (LIFs) cover the secondary septa, and matrix proteins such elastin are deposited at the tip [
23,
25,
90,
91]. At first, alveolarization is quite fast (known as “bulk alveolarization”), but then, this process is slowed down, giving rise to the continued alveolarization. As the alveoli mature, the surrounding capillaries are remodeled, forming the capillary unit, and the endothelial cells are located in the proximity of the AEC1 cells permitting an efficient gas exchange. This process is known as microvascular maturation and occurs simultaneously with alveolarization [
23,
25,
30,
90,
91,
92,
93].
Secondary septation is intimately associated with several signaling events. For example, platelet-derived growth factor α (PDGFα) regulates myofibroblast differentiation and elastin production; TGFβ regulates elastin expression [
90,
91,
94], whereas ephrin B2 plays an essential role in endothelial cells. Furthermore,
fgfr3/fgfr4 double null mice fail to generate the secondary septa pointing to a role for FGF signaling in controlling this event [
95]. Finally, RA is crucial for proper alveolar formation [
23,
25].
Alveologenesis in the developing lung is partially regulated by vitamin A [
96], and endogenous RA is present in the postnatal lung [
97,
98]. Retinoids have been recognized over the years as alveolar morphogens and possible therapeutic mediators [
99]. Different studies have demonstrated that vitamin A deficiency induces major histological changes in the lung, namely: airspace enlargement, thinner alveolar walls, more alveolar breaks, and an increase in the mean free distance in the air spaces [
100]. Furthermore, vitamin A deficiency impairs lung epithelial function in rodents and promotes bronchopulmonary dysplasia (BPD) in humans [
101,
102]. The precise mechanism by which RA regulates alveolar formation remains poorly understood, although RA regulation of myofibroblast proliferation was shown to rely on intact FGF signaling [
25]. Conversely, RA supplementation in explant culture induces septation, and retinol treatment of premature lambs promotes alveologenesis [
103].
RA signaling machinery is differentially expressed during alveologenesis. For instance, in mice, CRBPI is present in the alveolar walls and exhibits higher expression levels around P9, whereas CRBPII is detected during alveolar formation at P4 [
97]. Furthermore, in the rat model, CRABP levels rise shortly after birth, reach its maximum values at P10, and at P21 it is barely detected. These genes were upregulated during alveologenesis in whole rat lung, and isolated LIFs [
104], and the alterations in the expression levels coincide with the morphological transformation of primitive saccules into differentiated alveoli [
105,
106]. Likewise, RALDH1 and RALDH2 are expressed in a temporal and spatial regulated manner in the lung and are associated with different patterns of alveolar cell wall proliferation. For example, in mice, RALDH1 levels are higher at P4, and it is found in LIFs populating alveolar walls, like CRBPI, and in the bronchial epithelium. Conversely, RALDH2 peaks just before birth, it slowly declines during alveologenesis, and it is expressed in the bronchial epithelium and pleural mesothelial cells but not in the alveolar walls [
107]. Secondary septation is RALDH/RA-dependent. Epithelium-derived vascular endothelial growth factor A (VEGFA) regulates RALDH levels and, consequently, RA production by endothelial cells. RA acts as a paracrine factor to induce the expression of FGF18 by lung fibroblasts that, on its turn, regulates elastin deposition [
108].
RA and RAR receptors are crucial for septation and secondary crest formation [
94]. RARα, RARβ, and RARγ were identified in rat lung isolated LIFs and in postnatal mice lung, namely RARα1, RARβ2, RARβ4, and RARγ2 [
107]. RARs are present in the alveolar walls, bronchial epithelium, pleura, and bronchial vascular smooth muscle. Their expression changes with time and, in mouse, increases significantly at P4 [
97]. Lungs from
rarα−/− mice are similar to wild type at P14 (end of septation), but, at P50, the alveoli number and surface area are decreased. These results hint that RARα is not vital for alveolar septation, but it may have a role in later phases of alveologenesis [
109]. Conversely, increased RA signaling of a dominant active RARα receptor in the epithelium leads to lung immaturity [
88]. In
rarβ−/− mice (exon 10 deletion), septation occurs earlier and faster; also, the administration of RARβ specific agonists in the rat model impairs septation. Overall, it seems that RARβ negatively controls the septation process [
110]. However, RARβ seems to be important for neonatal alveolar growth, as disclosed by studying a different
rarβ−/− mutant (exon 6 deletion) that displayed a decreased surface area of gas exchange [
111]. RARγ is required for alveoli formation during the first 28 postnatal days.
rarγ−/− display a decrease in the elastic tissue of the whole lung, and the alveoli number. In contrast, the distance between the alveolar walls and the mean chord length increased. Additionally, in lipofibroblasts, the trophoelastin mRNA decreased at P12 [
94]. Moreover, RARγ agonist’s administration promotes alveolar repair in an animal model of emphysema [
112]. Altogether, it seems that RARγ positively regulates pulmonary septation. Furthermore, in cultured LIFs, it was demonstrated that RARβ and RARγ increase at birth, which corresponds to the peak of RA storage. The increase in RARγ is temporary since it decreases after P2 (RA in the LIFs also decreases after postnatal day 2). In summary, RA may act at RARγ level in the early postnatal period [
107]. RAR heterodimerizes with RXR before binding to DNA. Homozygous null RXR-α mice die
in utero. Additionally, null for RARγ and heterozygote for RXR-α present decreased elastin expression in the LIFs at P10; and a decrease in pulmonary elastic tissue in the alveolar septa and not at the airway or vascular walls at P28 [
94].
After the administration of retinyl palmitate to pregnant rats, the levels of retinyl esters increase in the fetal and postnatal lung [
113], which implies that fetal lungs store retinol or retinyl esters from the progenitor. The lung is the second biggest storing place of retinoids following the liver [
114]. LIFs are the main retinoid reservoir of the lung and contain all the components of the pathway [
104,
114,
115]; consequently, they can uptake circulating retinol or hydrolyze stored retinyl esters and convert them into retinol or RA [
116,
117]. LIFs are localized in the septating tissue adjacent to AEC2 [
118]. LIFs generate all-trans retinoic acid (ATRA) that acts autocrinally to upregulate elastin gene expression and synthesis, thus playing a crucial role in the induction of septal eruption [
116,
119,
120]. Moreover, ATRA acts paracrinally to induce proliferation of the adjacent AEC2 [
121,
122], gene expression [
115], and angiogenesis in microvascular endothelial cells [
123]. After birth, esters start to disappear from the lung and are converted into active forms, like retinol and RA [
98,
104,
124]. Retinyl esters are abundant in the last three prenatal days (similar amount comparing to the liver) [
117], and its depletion correlates with lung maturation [
98]. Retinoid clearance is associated with changes in the epithelium of the conducting airways. Specifically, cell phenotype alters from stratified columnar epithelium with goblet cells to keratinizing squamous epithelium [
125].
RA regulates positively or negatively the expression of many genes. Among them, RA is important for the synthesis of the surfactant proteins SPA, SPB, and SPC. Administration of retinyl palmitate at high doses to pregnant rats elevates both total phospholipid and the desaturated portion of phosphatidylcholine of the pulmonary surfactant. However, SPA concentration remains unchanged. Additionally, repetitive RA administration increases surfactant phospholipid content [
126]. On the other hand, RA also has inhibitory actions. In some studies, it was shown that RA decreases the expression of both mRNA and protein levels of SPA [
127].
Regenerative processes are intimately connected with the reawakening of developmental programs [
128], and RA has been described as important in alveolar regeneration. Exogenous ATRA, RARα and RARγ agonists and 4-oxo RA can induce alveolar regeneration in adult rats displaying emphysema and partially rescue their phenotype [
110,
112,
129]. On the contrary, pan RXR agonist, 13-cis RA, and retinol were not regeneration inducers, and RARβ was not required for regeneration [
130]. In some studies, ATRA was shown to induce apoptosis, a normal process in wound healing, in rats previously treated with elastase, rescuing the alveolar surface area whereas, in others, RA did not affect lung function [
131,
132]. Recently, using lung organoid models, it was shown that RA pathway stimulation led to a decrease in the organoid size and inhibited epithelial proliferation. In contrast, RA pathway inhibition promoted epithelial proliferation in mice lung organoids and human organoids from chronic obstructive pulmonary disease (COPD) patients. In the mouse model, increased proliferation happened with concomitant suppression of epithelial differentiation from the airway and alveolar epithelium. Furthermore, cell proliferation was intermediated by YAP (yes-associated protein) activation and FGF signaling. Lastly, the inhibition of Histone deacetylase in combination with ATRA was proposed as a potential method to restore adult lung epithelial cell differentiation [
133]. An
in silico study provided the first clues regarding the possible role of ATRA in minimizing inflammation in elastase-induced emphysema in rat lungs and, therefore, in alveolar epithelium regeneration. It was proposed that ATRA can bind to receptors and ligands of both ERK and JAK-STAT signaling pathways, namely, TNF-α, IL6ST, TNFR1, and IL6. Furthermore, ATRA showed more binding efficiency for TNF-α and IL6ST and can potentially regulate both ERK and JAK-STAT pathways by acting at its first steps. ATRA administration restored lung histology, the proteases/antiproteases balance (imbalance is characteristic of emphysema condition), the levels of inflammatory markers and antioxidants, and the expression of candidate genes of ERK and JAK-STAT. In conclusion, ATRA reduces inflammation and improves alveolar epithelium regeneration in rat lung with emphysema [
134].