Many people live under stressful conditions which has an adverse effect on their health. Human stress, especially long-term one, can lead to a serious illness. Therefore, monitoring of human stress influence can be very useful. We can monitor stress in strictly controlled laboratory conditions, but it is time-consuming and does not capture reactions, on everyday stressors or in natural environment using wearable sensors, but with limited accuracy. Therefore, we began to analyze the current state of promising wearable stress-meters and the latest advances in the record of related physiological variables. Based on these results, we present the concept of an accurate, reliable and easier to use telemedicine device for long-term monitoring of people in a real life. In our concept, we ratify with two synchronized devices, one on the finger and the second on the chest. The results will be obtained from several physiological variables including electrodermal activity, heart rate and respiration, body temperature, blood pressure and others. All these variables will be measured using a coherent multi-sensors device. Our goal is to show possibilities and trends towards the production of new telemedicine equipment and thus, opening the door to a widespread application of human stress-meters.
- human stress
- multi-sensor
- telemedicine
- electrodermal activity
- monitoring
- interdigital array of electrodes
1. Human Stress Phenomena
Stress in some forms affect people every day and the World Health Organization calls stress a “21st Century Health Epidemic” [1]. However, what does the word stress really mean? We can look at it from several angles. In the past, stress was viewed differently and this word is still used inconsistently between disciplines. Until the 16th century, this term was used directly for physical injuries. In the 17th century, stress was associated with sadness, misery, and suffering, while in the 18th and 19th centuries, the word stress was understood as tension, pressure, and effort due to the development of physics. In the 20th century, the view of stress was significantly influenced by wars, fatigue from fighting and nervous shocks suffered by soldiers. At the end of the 19th century, on the basis of significant experiments, the view began to focus on emotions, the homeostasis of the organism and stress started to be thought of as a burden that causes changes in mental health and affects a person’s physiology. At the beginning of the 20th century, the response to short-term stress after the secretion of adrenaline was concretized by Walter Cannon, who described prepares the organism for a rapid “fight or flight” response, and who made significant discoveries with respect to internal balance—homeostasis. On the other hand, Hans Selye known as the “father of stress”, focused on the chronic, long-term stress. He pointed to the role of the brain and the adrenal cortex in response to stress and identified several hormones that regulate the stress response. Unlike previous years, he emphasized the importance of psychological and social factors in inducing a stress response. He gave the first definition of stress, where it is referred to the mutual action of forces that take place in any part of the body, physical or mental and which represent a psychophysiological response of an individual mediated primarily by the autonomic nervous system (ANS) and the endocrine system [1][2][3][4]. Selye also described the “General Adaptation Syndrome” [2][4], which deals with changes in the body after exposure to stress, arguing that each stressor factor stimulates the same response in the body. Today, stress can be described as “any effect of a change in the environment on a living being that results in disruption of the homeostasis of that living being” [4].
Nowadays, stress is categorized mainly as acute (short-term) and chronic (long-term) [5][6][7]. The human body responds differently to various durations of stress stimuli Acute stress can be for example a job interview, a fine for speed and more. Certainly, acute stress is unpleasant, but the reaction can be positively influenced by soothing breathing or rapid physical activity [8][9][10][11][12][13]. The problem arises when the stress is too intensive, the stressors accumulate and one cannot get rid of them. Persistent chronic stress may have a milder course, but the body is prepared for a stress response long time. Stress hormones are released and the body does not recover as fast as when it is at rest. This can lead to more severe physiological manifestations than those of acute stress. People might feel headaches, insomnia, fatigue, inattention, digestive problems, and memory impairment can occur [14][15][16][17][18][19][20][21]. Each individual respond to stress differently. Effective stress management involves the identification and management of both acute and chronic stress. And it is precisely to be aware of the stress response and subsequent compensation that it is possible to monitor a person’s physiological condition and change life for the better and predict disease [22]. While acute stress can stimulate a person to perform better, in chronic stress performance decreases rapidly. This also applies to stress in the workplace. Not only a person has physiological manifestations of stress, but also stress is reflected in the results of work done, loss of productivity, burnout, dissatisfaction with work and others [23][24][25][26][27]. Solving the issue of stress is very important from a human and economic point of view. According to The American Institute of Stress, work stress is a major source of stress for adult Americans and is on the rise. They reported that approximately 33% of people experience extreme stress. Stress is responsible for 80% of accidents and 120,000 deaths per year in the workplace. The Global Organization for Stress reported 75% of Americans and 91% of Australians exposed to stress. At work, 80% of American and 86% of Chinese workers experience stress. They are also reported 450,000 workers in Britain with stress-related illnesses. About half of people exposed to stress are affected by post-traumatic stress disorder (PTSD) and acute stress disorder. The downside is that it tends to get worse and no one is completely resistant to stress. An increasing number of people exposed to stress and the contraindications associated with stress show us that there is a need for equipment and methodology that would help detect stress and fluctuations in mental health and help reduce them [14][28][29][30][31][32][33][34][35][36]. The stress is affecting also the economy, and U.S. employers are spending health care and working days at $300 billion a year. In Britain, people miss out on 13.7 million working days a year because of the stress, and it costs them about $37 billion, and in Australia, stress is responsible for the loss of $14.2 billion. Stress in everyday life and in the workplace is related to anxiety and depression. Statistically, more than 300 million people suffer from depression and, along with anxiety, are the most common mental disorders. The annual global cost is estimated at $2.5 trillion and is very likely to increase in the coming years [30][31][32][34][35][36][37].
Stress from the perspective of medicine shows how stressors stimulate the human body to defend itself. The response to stress affects the whole biological system of the organism and physiological processes. This is manifested by various symptoms, often deleterious individual problems such as headaches, gastrointestinal disorders, anxiety, hypertension, coronary heart disease and depression [38]. It should be mentioned that the response on stress begins in the same way. During the stress response, the stress hormones adrenaline and noradrenaline, which are released by the sympathetic nervous system, and cortisol that is produced after activation of the hypothalamic-pituitary-adrenal axis, are released [39]. Cells in the body express receptors for stress hormones, so they are easily provided with information about the stress stimulus. Other factors such as adrenocorticotropin (ACTH), oxytocin and vasopressin, cytokines (interleukin-6 and interleukin-1β) also play a role in stress. The length and magnitude of action of these factors depend on the stressor type. Overall, the response to stress is still biologically consistent and these physiological symptoms are suitable for measurement [11][18][19][40][41][42][43]. Autonomic nervous system (ANS) plays main role in the response to stress, which cannot be controlled by our own will. It consists of sympathetic and parasympathetic systems; whose balance regulates the physiological degrees of “arousal” in the response to signals from the environment. The parasympathetic regimen regulates the maintenance of energy and the renewal of the organism; sympathetic one stimulates increased heart rhythm, blood pressure, dilated pupils, sweating and other physiological manifestations caused by the secretion of adrenaline and norepinephrine. These manifestations are visible even under stress [44], so we focused on the possibility of recording them as well as on the subsequent interpretation of a person’s condition [22][45][46][47][48][49]. The primary response to stress triggers a sympathetic nervous response that regulates the adaptation to the external environment. The hypothalamus secretes hormones that stimulate the pituitary gland and thus begin to regulate the stress response. The pituitary gland secretes adrenocorticotropic hormone (ACTH) into the blood. This hormone helps to balance the intensely regulated stress response. The amygdala, in turn, regulates emotional processes. Activities in the prefrontal cortex are temporarily suppressed (planning, attention, problem solving). Adrenaline and norepinephrine and cortisol are excreted. Serotonin, which regulates mood, especially depression and anxiety, is also secreted. The hypothalamic-pituitary-adrenal (HPA) axis enables the communication of three endocrine glands (hypothalamus, pituitary, adrenal gland), which ensure the stress response, but also digestion, mood, autoimmune system, energy, sexual cycles [28]. Inflammatory markers eluted approximately 90–120 min after the onset of acute stress, specifically IL-6, IL-1β and TNF-α. Acute stress induced an increase in the pro-inflammatory transcription factor NF-κB with the highest amount after 10 min. Chronic stress shows less inflammation, and available studies show elevated levels of TNF-α and CRP over an observation period of 3 years. Inflammatory cytokines and CRPs may play a role in increased amounts of secreted cortisol [50].
Also interesting is the connection between stress, CNS, ANS and voice output, which consists of three stages—breathing, phonation and resonance. Thus, ANS is responsible not only for the stress response but also for the creation of voice and speech. Even a shaking voice is our body’s response to stress. The voice can be a very sensitive indicator of a person’s emotions, attitudes, mental experience, depression, anxiety, tremor or physical fatigue. Voice quality can be the result of tension throughout the body, which also manifests itself locally as a specific tension in the external and internal laryngeal muscles [51]. It’s all about the vocal cords, which in this case affects the ANS. There are currently several studies that attempt to identify stress patterns of voice using neural networks and machine learning [52][53][54]. Some even combine speech signals with electrodermal activity [55] or use wearable devices with multi-sensors combining audio and physiological sensors together with deep neural learning networks to monitoring an individual’s well-being in a naturalistic environment [37][56][57].
In order for stress to begin, an individual has to be first be exposed to a certain stressor, which initiates a stress response. Anything that forces the body to release stress hormones can be a stressor and cause stress. Stressors can be divided into psychological and physiological. Physiological effects on the body include, for example, very high/low temperatures, injuries, chronic diseases, infection or pain. Psychological (mental) stressors can be attributed to life situations, negative social communications, conflicts, failure to satisfy internal drives and others [12][14][58][59]. The division into physical and psychological stressors is also based on the scientific function of the organism, because these various stressors activate every other part of the brain, and the trace they leave can be used back to concretize the stressor [12]. On the other hand, stressors can also be divided into absolute stressors, which would be evaluated by everyone who is exposed to them as stress (objective stress factors such as natural disasters) and relative stressors, where we can include effects that only part of the population would declare as the stress initiators (subjective stress factors such as time pressure, tax payment, school exam) [6][11][60][61][62][63]. However, all stressors activate the same biological response of the body [39]. To determine the stress to which a person is exposed, the “Social Readjustment Rating Scale” (SRRS) was released in 1967 [64], but it was not ideal because it offered a very subjective view.
The stress monitoring techniques used today are based on several variables as self-assessment, measurement of behavior and cognitive functions, and finally on physiological manifestations. In our study, we focus mainly on physiological manifestations, because they are an objective manifestation of the organism [23][27][44][65][66].
2. Advanced Wearable Stress-Meters
Current human stress monitoring devices are usually very inaccurate or rely on a strictly controlled laboratory environment. The concept proposed in this paper is based on our long-term experience in this scientific field in which we have been operating for the last 10 years [67]. In this work, we focused on a multi-sensor device, because one separate sensor is not able to determine whether a person is really exposed to stress. Simply put, the electrical conductivity of EDA actually only responds to brain activity. Using memory is less energy-intensive than inventing new things. As an example, a lie detector can be used. It works on the principle that when person telling the truth, the brain is not so burdened (EDA drops) as when a person lies, invents and the brain is more congested (EDA increases). The EDA does not distinguish whether the increase in conductivity actually occurs due to real stress or only increased physical or mental activity. A single sensor does not know if the change in finger temperature is caused by stress or the outside temperature. It does not know if posture affects respiration or HRV. Therefore, a reliable and accurate stress monitor that includes not only long-term stress but also acute short-term stress must be multi-sensor. The result must be supplemented by other physiological variables in order to obtain the most comprehensive view of the overall situation of a subject under test. Our aim is to create a multi-sensor device for sensing several physiological variables. An advanced stress meter must be something like a portable lie detector, which also captures blood pressure, pulse, respiration in addition to skin conductivity.
2.1. Multi-Sensor Monitors Overview
A large number of scientists have been interested in the idea of using the coherence of several sensors to determine stress in their laboratories [68][69][70][71]. For example it is worth to mention the classifier of negative emotion induced by a visual stimulation evaluated from EDA, ECG and skin temperature [72], multimodal emotion evaluation from combination of EDA, ECG and EMG [73], driver anxiety detection using EDA, PPG, EEG and pupil information [74], identification of cognitive tasks by machine learning from EDA and HRV [75], evaluating of mental workload during web browsing from EDA, PPG and EEG [76][77]. Nowadays, the trend is the use of virtual reality [78][79].
In the current scene of wearable devices usable in the diagnosis of human stress, we have discovered several promising commercially available multi-sensor systems. Smart health watches are very widespread in the today’s population. Since early 2010s, the CPU computational power and the overall performance have been high enough to run sophisticated machine learning algorithms, and such devices are able to derive stress from HR. Actually, the most popular way to detect stress today is using wrist wearables. WHOOP’s Recovery metric uses HRV, resting HR, sleep and respiratory rate to determine the state of recovery after body underwent stressful endurance physical training [80]. Nowadays, smartwatches and trackers from Garmin [81] such as Vivoactive 4, Vivosmart 4, Fenix 6, from Samsung [82] Galaxy Watch and Galaxy Watch Active 2, from Apple Watch Series 6 [83], Google Wear smartwatches [84] such as Fossil Gen 5, Fossil Sport, TicWatch E2 and Skagen Falster 3 and Fitbit products [85][86] such as Charge 4, Versa 3 and Ionic are worth mentioning devices on the market. An interesting solution from the Fitbit Company in the Sense product is the possibility to measure also the SCL of EDA after placing your second hand over the watch thanks multi-path electrical sensor [85]. Using Fitbit Sense, you can make a mental well-being practice. Clinical studies have shown that such meditation is very effective in reducing stress [28]. Last but not least, Withings Scanwatch [87] with medical grade ECG and oximeter and two devices from company Empatica: Embrace 2 and E4 should be mentioned [88][89][90]. Both are in the form of wristband and can stream the following variables in real time: EDA, wrist temperature and accelerometric signal. E4 is enhanced further by employing a PPG sensor. Embrace 2 was especially designed for epilepsy monitoring, sleep/rest management and physical activity tracking. E4 is more suitable for lab or home recording, real-time clinical observation and raw data analysis. Very interesting is also Samsung health device concept Simband with Simsense [91], which includes PPG, EDA, skin temperature, 3D accelerometer and ECG lead. Today’s advances in miniaturization allow us to monitor physiology with a ring. Perfect example is the Oura health ring, which includes PPG and temperature sensors together with an accelerometer and a gyroscope encapsulated in an attractive package [92]. Another very common form of recording human physiology are chest-belts. A typical representative is, for example, Zephyr Bioharness 3 that includes HR, RR and accelerometric monitoring [93]. One can also appreciate the design of the non-traditional Qardiocore chest holter [94] that captures ECG, RR, temperature and activity recognition, as well as Wearable biosensor from Philips [95], which contains an ECG sensor together with an accelerometer and a skin temperature sensor. A chapter in themselves are headband neurotrackers like Neurosky Mindwave [96], Muse 2 EEG [97], and Flowtime [98] that monitors EEG and helps to reduce stress through meditation. Muse 2 and Flowtime have also an integrated PPG sensor. Spire Health Tag [99] is also worth mentioning. This device can be adhered inside clothes and detect heart rate, breathing patterns, and body movements to assess the emotional and mental well-being of a person. Detailed parameters of the selected wearable devices suitable for stress-detection can be found in Table 1. Within some experiments, scientists have developed their own designs. One of these offers stress detection from portable ECG and EDA, where authors use two channels EDA and ECG to suppress undesired artifacts [100]. Another example is the activity recognition system (mental, physical and emotions) based on combination of ECG and respiration sensor, and EDA gloves [101]. Systems using speech analysis also appear to be very promising for stress analysis purposes. These systems can be easily incorporated into modern mobile phones [102]. In the research of Jin et al. [37], in addition to the speech analysis itself, they included behavioral signals (3D accelerometer and 3D angle sensor) and propose an attention-based deep-learning architecture for a more accurate classification of mental state. Nowadays, there are even systems that perform the analysis of biomarkers from sweat and saliva directly during sports activities [103]. The current literature summary of stress assessment using wearable multi-sensors in the natural environment includes: emotion recognition by neural networks from portable eyetracker and Empatica E4 [104], ANS research using again E4 but now with ECG and respiration sensors [105], development of cognitive load tracker using machine learning [106], smart stress reduction system using E4 combined with accelerometers [107], validation of wireless sensors for psychophysiological studies and stress detection [108][109], prediction of relative physical activity [110], real-time monitoring of passenger psychological stress [111], classification of calm/distress condition [112], assessment of mental stress of fighters [113], and others. A comprehensive overview about pain and stress detection using available wearable sensors was actually made very recently by Jerry Chen et al. [114]. They mention, stress monitoring using mobile EEG head set MindWave [115], ECG and EMG DataLOG [116], using a combination of MindWave EEG (NeuroSky, San Jose, CA, USA), Zephyr BioHarness 3 chest belt (Medtronic, Boulder, CO, USA), Shimmer Sensor (Shimmer Sensing, Dublin, Ireland) [117] and mobile sensors suite AutoSense (National Institutes of Health, Bethesda, MD, USA) [118]. Mental health monitoring using ubiquitous wearable sensors [119] and machine learning [120][121] has been also described.
Table 1. Technical parameters of selected wearable devices suitable for stress-detection.
| Garmin Vivoactive 4 [81] |
| Sensors: PPG 1, accelerometer, gyroscope, compass, barometer, thermometer, microphone, ambient light, GPS, GLONASS, Galileo |
| Physiology variables: HR, spO2, stress 2, respiration 2 (meditation), sleep and activity tracking, body battery energy |
| Connectivity: Bluetooth, Wi-Fi, NFC, ANT+, Waterproof: 5 ATM; Form: Watch |
| Samsung Galaxy Watch Active 2 [82] |
| Sensors: PPG 1, ECG 3, accelerometer, gyroscope, compass, barometer, microphone, ambient light, GPS, GLONASS, Galileo, Beidou |
| Physiology variables: ECG 3, HR, BP 3, stress 2 (meditation), sleep and activity monitoring |
| Connectivity: Bluetooth, Wi-Fi, NFC; Waterproof: 5 ATM; Form: watch |
| Google Fossil Gen 5 [84] |
| Sensors: PPG 1, accelerometer, gyroscope, compass, barometer, microphone, ambient light, GPS |
| Physiology variables: HR, stress 2 (meditation), sleep and activity monitoring |
| Connectivity: Bluetooth, Wi-Fi, NFC; Waterproof: 3 ATM; Form: watch |
| Apple Watch 6 [83] |
| Sensors: PPG 1, ECG 3, accelerometer, gyroscope, compass, barometer, microphone, ambient light, GPS, GLONASS, Galileo |
| Physiology variables: ECG 3, HR, spO2, sleep and activity monitoring |
| Connectivity: Bluetooth, Wi-Fi, NFC; Waterproof: 5 ATM; Form: watch |
| Withings Scanwatch [87] |
| Sensors: PPG 1, ECG 3, accelerometer, gyroscope, compass, barometer, ambient light |
| Physiology variables: ECG 3, HR, spO2 (medical grade), sleep and activity tracking |
| Connectivity: Bluetooth Low Energy, USB; Waterproof: 5 ATM; Form: watch |
| Fitbit Sense [86] |
| Sensors: PPG 1, ECG 3, EDA 3, thermometer, accelerometer, gyroscope, barometer, microphone, ambient light, GPS, GLONASS |
| Physiology variables: ECG 3, HR, spO2, peripheral temperature, stress (meditation), sleep and activity monitoring |
| Connectivity: Bluetooth Low Energy, Wi-Fi, NFC; Waterproof: 5 ATM; Form: watch |
| Samsung Simband [91] |
| Sensors: PPG 1, ECG 3, EDA, bioimpedance, thermometer, accelerometer |
| Physiology variables: ECG 3, HR, EDA, bioimpedance (blood flow), peripheral temperature, activity tracking |
| Connectivity: Bluetooth, USB; Form: watch |
| Empatica Embrace 2 [90] |
| Sensors: EDA, temperature, accelerometer, gyroscope |
| Physiology variables: EDA (clinical grade), peripheral temperature, stress, sleep and activity tracking |
| Connectivity: Bluetooth Low Energy; Waterproof: 0.1 ATM; Form: wristband |
| Empatica E4 [90] |
| Sensors: PPG 1, EDA, infrared temperature, accelerometer, event maker |
| Physiology variables: HR, spO2, EDA, peripheral temperature, activity tracking |
| Connectivity: Bluetooth Low Energy, USB 2.0, Raw data analysis; Waterproof: 0.1 ATM; Form: wristband |
| Zephyr Bioharness 3 [93] |
| Sensors: HR, RR, accelerometer |
| Physiology variables: HR, RR, activity monitoring |
| Connectivity: Bluetooth Low Energy; Form: chest-belt |
| Quardiocore [94] |
| Sensors: ECG, skin temperature, accelerometer, gyroscope, compass |
| Physiology variables: ECG, HR, RR, body core temperature, activity tracking |
| Connectivity: Bluetooth 4.0; Form: chest-belt |
| Philips Wearable biosensor [95] |
| Sensors: ECG, skin temperature, accelerometer |
| Physiology variables: ECG, HR, RR, body core temperature, activity tracking |
| Connectivity: Bluetooth; Form: chest-belt |
| Oura health ring [122] |
| Sensors: PPG 4, accelerometer, gyroscope, NTC thermometer |
| Physiology variables: HR, RR 2, peripheral temperature, stress (meditation), sleep and activity tracking |
| Connectivity: Bluetooth Low Energy; Waterproof: 10 ATM; Form: ring |
| Neurosky MindWave [96] |
| Sensors: EEG |
| Physiology variables: EEG |
| Connectivity: Bluetooth/Bluetooth Low Energy dual mode; Form: headband |
| Muse 2 EEG [97] |
| Sensors: EEG, PPG 1, accelerometer, gyroscope |
| Physiology variables: EEG (emotions), HR, stress (meditation) and activity tracking |
| Connectivity: Bluetooth 4.2, USB; Form: headband |
| Flowtime EEG [98] |
| Sensors: EEG, PPG 1 |
| Physiology variables: EEG, HR, stress tracking (active/neutral/calm) |
| Connectivity: Bluetooth; Form: headband |
| Spire Health Tag [99] |
| Sensors: PPG 1, accelerometer |
| Physiology variables: HR, RR 2, stress (calm/focus/tension), sleep and activity tracking |
| Connectivity: Bluetooth; Form: adhered to clothes; Washer and dryer proof |
| Multi-sensor concept |
| Sensors: ECG, PPG 4, respiration, EDA (IDA microelectrodes), 2× infrared temperature, 2× accelerometer, gyroscope, compass |
| Physiology variables: ECG, HR, spO2, EDA, respiration, peripheral and body core temperature (heat gradient), BP (derived from ECG and PPG), stress, sleep and activity monitoring |
| Connectivity: Bluetooth Low Energy, USB; Form: ring and chest-belt |
2.2. The Proposed Multi-Sensor Concept
Based on the analysis described in the previous sections, we still see points where current multi-sensor monitoring systems can be improved, and therefore we come up with our own concept. From practical reasons, the main idea behind the concept is to divide the stress-meter system into two separate sub-systems (Figure 1). We consider appropriate to place one sub-system on bottom parts of non-dominant hand, ideally on fingers (smart-ring) as depicted in Figure 1a. The second part of sensors should be placed on the chest in the heart area, most probably in the form of a smart sticker or a tiny chest belt, as depicted in Figure 1b. The keystone lays in the precise time synchronization of those two sub-systems.
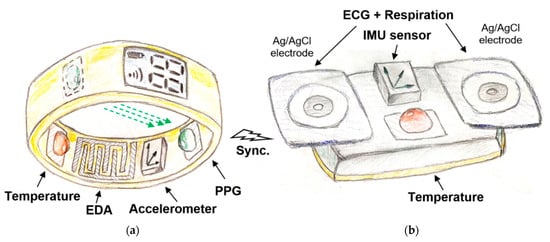
Figure 1. Concept of new stress-meter: (a) smart ring, (b) chest holter.
Let us start with a smart ring illustrated in Figure 7a. The basis component, as in most other stress detection devices, should be an exosomatic EDA sensor stored in a smart-ring (Figure 7a). For practical reasons of long-term monitoring, we choose dry electrodes and harmonic signal. However, instead of conventional macroelectrodes, we recommend using optimized microelectrodes in the form of symmetrical IDA microelectrodes of dimensions between 100/100 and 200/200 μm (finger/gap). In this way, we will be able to obtain the EDA signal from a smaller area and the measure signal will be more tied to nerve activity and stress. In the first research phases, we would not even ignore the possibility of measuring the complex impedance at different frequencies. From our experience a harmonic input signal with the frequency value about 1 kHz and the amplitude between 1.5 and 3 V is recommended. Since dry microelectrodes are intended to be used, there will be a need to minimize the motion artifacts. Despite the fact that we have high hopes for software filters, built in circuity as a part of a standard physical sensor is assumed. A simple accelerometer seems to be the most suitable choice, but using the piezoelectric pressure sensor we can obtain direct information about the contact force between the electrodes and the skin. Another essential part of this sensor sub-system must be the optical HR sensor, where conventional PPG sensor can be used. As confirmed in the previous analysis, monitoring of blood oxygenation is not necessary, but at the present COVID-19 time, will certainly not be redundant. The transmittance principle of PPG used on fingers has been suggested in [123], which is more reliable compared to the reflective principle. The last sensor in the ring/watch sub-system should be a reliable thermometer, whether it is a contact thermocouple or an optical one. It should not be a problem to place all these sensors in a still compact ring of about 1.5 cm thickness. An area of about 2 cm2 is sufficient for EDA electrodes, LED and photodiode placed opposite each other and the thermal sensor occupy only a few tens of mm2. The battery and the transmitter are the largest parts. If there is a requirement for further integration, we have experience with the use of transparent metals for EDA electrodes [124]. Such a design would allow the placement of optical sensors directly behind EDA electrodes.
The second multi-sensor sub-system (Figure 7b) should definitely contain an ECG sensor. The quality of the ECG itself is not important, we are dominantly interested only in the exact estimate of the R peak in the QRS complex. From this information we obtain HR and, thanks to the precise synchronization with the first sensor sub-system and the PPG, also pulse transition time (PTT) which is relative to BP. If the quality of ECG is high enough, it will definitely not hurt. ECG holters are the most commonly used telemedicine devices and they can also monitor other cardiovascular parameters that can more accurately determine the physiological condition. We have good experience with chips from Texas Instruments (TI 1292R) [125], which also integrate a reliable respiration impedance sensor, so in this way, the second important physiological parameter—the respiration could be obtained. Biosignals can be measured using Ag/AgCl adhesive electrodes with the sufficient mutual distance of 5 cm. Another important sensor is an IMU sensor (3-axis accelerometer, gyroscope and compass). There are an infinite series of IMU sensors. Since the IMU sensor will be placed on the chest, the best overview of posture and physical activity of the body can be extracted. An IMU sensor on your hands or feet would not be reliable enough. Information on overall human activity will help us better understand the very important phasic response of the EDA signal. We know that in some situations, especially with higher physical activity, the signal from the accelerometer so-called seismocardiographic signal, can replace the ECG signal in determining HR [126]. The last used sensor here is again a body core thermal sensor.
From the all sensors used, the following physiological variables will be obtained: ECG and chest temperature, HR and finger temperature, EDA, EDA motion artefacts, respiration, posture and physical activity. Synchronization is now entering the scene. For sub-systems synchronization and external communication we plan to use Bluetooth Low Energy. By comparing the temperature of the finger and chest, one can get information about the heat gradient and so-called “circulating shock” level. From the determination of the time shift between the ECG and PPG signals, continuous information about the blood flow rate will be available, which in our case can be considered as BP. Here is the key to accurate synchronization. We estimate that an inaccuracy of 5 ms corresponds to a blood pressure error of 1 mmHg corresponding to the average person when using a ring. We should try to achieve a sync error of about 1 ms [127]. Additional information on systolic and diastolic pressure can also be obtained by analyzing the shape of the PPG curve [128][126][129]. In addition to bluetooth connectivity, the concept can be also connected via USB. The device will have integrated an internal memory (micro SD card), real-time clock and battery management circuitry. The battery management is one of issues to be investigated further. Here, energy harvesting systems generating electrical energy from ambient environment represent a promising solution towards enhancing the battery lifetime or avoiding the necessity of battery change that might be very impractical and inconvenient in some applications [130][131] could be effectively employed to provide a self-powered (at least partially) electronic system. Detailed parameters of proposed multi-sensor concept are summarized at the end of Table 1.
After designing a device, which is the main development goal in the near future, the experimental part will follow. The biggest challenge will be to examine the coherence of all the measured physiological variables during different situations in human life. Some mutual relations have been already analyzed within the previous analysis, however, skillful programmers and the use of neural networks and machine learning will be in high demand. Of course, one cannot avoid laboratory and simulated situations supplemented by standard psychological tests and stress assessments, whether by standardized questionnaires or by measuring hormone levels to fine-tune the device.
This entry is adapted from the peer-reviewed paper 10.3390/s21103499
References
- Fink, G. Stress: Definition and history. Encycl. Neurosci. 2009, 549–555.
- Cooper, C.L.; Dewe, P. Stress: A Brief History; Blackwell Publishing Ltd.: Oxford, UK, 2008; ISBN 9780470774755.
- Robinson, A.M. Let’s talk about stress: History of stress research. Rev. Gen. Psychol. 2018, 22, 334–342.
- Selye, H. The Stress of My Life; McGraw-Hill: New York, NY, USA, 1976; ISBN 9780070562080.
- Lupien, S.J.; Juster, R.P.; Raymond, C.; Marin, M.F. The effects of chronic stress on the human brain: From neurotoxicity, to vulnerability, to opportunity. Front. Neuroendocr. 2018, 49, 91–105.
- Lupien, S.J.; Ouellet-Morin, I.; Hupbach, A.; Tu, M.T.; Buss, C.; Walker, D.; Pruessner, J.; McEwen, B.S. Beyond the Stress Concept: Allostatic Load-A Developmental Biological and Cognitive Perspective. Dev. Psychopathol. Second Ed. 2015, 2, 578–628.
- Soreq, H.; Friedman, A.; Kaufer, D. (Eds.) Stress—From Molecules to Behavior; Wiley: Hoboken, NJ, USA, 2009; ISBN 9783527323746.
- Rohleder, N. Stress and inflammation—The need to address the gap in the transition between acute and chronic stress effects. Psychoneuroendocrinology 2019, 105, 164–171.
- Gabrys, R.L.; Howell, J.W.; Cebulski, S.F.; Anismana, H.; Matheson, K. Acute stressor effects on cognitive flexibility: Mediating role of stressor appraisals and cortisol. Stress 2019, 22, 182–189.
- Nicolaides, N.C.; Kyratzi, E.; Lamprokostopoulou, A.; Chrousos, G.P.; Charmandari, E. Stress, the stress system and the role of glucocorticoids. Neuroimmunomodulation 2014, 22, 6–19.
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391.
- Dayas, C.V.; Buller, K.M.; Crane, J.W.; Xu, Y.; Day, T.A. Stressor categorization: Acute physical and psychological stressors elicit distinctive recruitment patterns in the amygdala and in medullary noradrenergic cell groups. Eur. J. Neurosci. 2001, 14, 1143–1152.
- Walker, F.; Nilsson, M.; Jones, K. Acute and Chronic Stress-Induced Disturbances of Microglial Plasticity, Phenotype and Function. Curr. Drug Targets 2013, 14, 1262–1276.
- Sawyers, C.; Sheerin, C.; Eastman, M.; Burchett, J.; Howell, P.; Neigh, G.; Amstadter, A.B.; Hettema, J.; Roberson-Nay, R. Genetic and environmental influences on cortisol reactivity to a psychosocial stressor in adolescents and young adults. Psychoneuroendocrinology 2021, 127, 105195.
- Hofmann, S.G.; Asnaani, A.; Vonk, I.J.J.; Sawyer, A.T.; Fang, A. The efficacy of CBT: A review of meta-analyses. Cogn. Ther. Res. 2012, 36, 427–440.
- Qin, H.Y.; Cheng, C.W.; Tang, X.D.; Bian, Z.X. Impact of psychological stress on irritable bowel syndrome. World J. Gastroenterol. 2014, 20, 14126–14131.
- Ray, A.; Gulati, K.; Rai, N. Stress, Anxiety, and Immunomodulation: A Pharmacological Analysis, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; Volume 103.
- Zong, Y.; Zhu, S.; Zhang, S.; Zheng, G.; Wiley, J.W.; Hong, S. Chronic stress and intestinal permeability: Lubiprostone regulates glucocorticoid receptor-mediated changes in colon epithelial tight junction proteins, barrier function, and visceral pain in the rodent and human. Neurogastroenterol. Motil. 2019, 31, e13477.
- Zefferino, R.; Di Gioia, S.; Conese, M. Molecular links between endocrine, nervous and immune system during chronic stress. Brain Behav. 2020, 1, e01960.
- Strike, P.C.; Steptoe, A. Psychosocial factors in the development of coronary artery disease. Prog. Cardiovasc. Dis. 2004, 46, 337–347.
- Yao, B.C.; Meng, L.B.; Hao, M.L.; Zhang, Y.M.; Gong, T.; Guo, Z.G. Chronic stress: A critical risk factor for atherosclerosis. J. Int. Med. Res. 2019, 47, 1429–1440.
- Fleshner, M. Physical activity and stress resistance: Sympathetic nervous system adaptations prevent stress-induced immunosuppression. Exerc. Sport Sci. Rev. 2005, 33, 120–126.
- Cooper, C.L.; Williams, S.; Sloan, S.J. Occupational Stress Indicator Management Guide; Windsor NFER-Nelson: Berkshire, UK, 1988.
- Ironson, G. Work, job stress, and health. Front. Ind. Organ. Psychol. 1992, 5, 33–69.
- Sauter, S.L.; Murphy, L.R. Organizational Risk Factors for Job Stress; American Psychological Association: Washington, DC, USA, 1995; ISBN 1-557-98297.
- Landy, F.; Quick, J.C.; Kasl, S. Work, stress, and well-being. Int. J. Stress Manag. 1994, 1, 33–73.
- Stanton, J.M.; Balzer, W.K.; Smith, P.C.; Parra, L.F.; Ironson, G. A general measure of work stress: The stress in general scale. Educ. Psychol. Meas. 2001, 61, 866–888.
- Spijkerman, M.P.J.; Pots, W.T.M.; Bohlmeijer, E.T. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clin. Psychol. Rev. 2016, 45, 102–114.
- Tran, L.; Xiao, J.F.; Agarwal, N.; Duex, J.E.; Theodorescu, D. Advances in bladder cancer biology and therapy. Nat. Rev. Cancer 2020, 21, 104–121.
- Adamson, M.M.; Phillips, A.; Seenivasan, S.; Martinez, J.; Grewal, H.; Kang, X.; Coetzee, J.; Luttenbacher, I.; Jester, A.; Harris, O.A.; et al. International prevalence and correlates of psychological stress during the global COVID-19 pandemic. Int. J. Environ. Res. Public Health 2020, 17, 9248.
- The American Institute of Stress. Available online: (accessed on 4 May 2021).
- Stress Statistics. Available online: (accessed on 4 May 2021).
- Here’s Why Workplace Stress Is Costing Employers $300 Billion a Year. Available online: (accessed on 4 May 2021).
- Stress in America. Available online: (accessed on 4 May 2021).
- Great Britain and Stress. Available online: (accessed on 4 May 2021).
- American Psychological Association. Available online: (accessed on 4 May 2021).
- Jin, J.; Gao, B.; Yang, S.; Zhao, B.; Luo, L.; Woo, W.L. Attention-Block Deep Learning Based Features Fusion in Wearable Social Sensor for Mental Wellbeing Evaluations. IEEE Access 2020, 8, 89258–89268.
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628.
- Dhabhar, F.S. The short-term stress response—Mother nature’s mechanism for enhancing protection and performance under conditions of threat, challenge, and opportunity. Front. Neuroendocr. 2018, 49, 175–192.
- Larrosa, P.N.F.; Ojea, A.; Ojea, I.; Molina, V.A.; Zorrilla-Zubilete, M.A.; Delorenzi, A. Retrieval under stress decreases the long-term expression of a human declarative memory via reconsolidation. Neurobiol. Learn. Mem. 2017, 142, 135–145.
- Joëls, M. Corticosteroids and the brain. J. Endocrinol. 2018, 238, R121–R130.
- Savage, B.M.; Lujan, H.L.; Thipparthi, R.R.; DiCarlo, S.E. Humor, laughter, learning, and health! A brief review. Adv. Physiol. Educ. 2017, 41, 341–347.
- Jung, Y.H.; Jang, J.H.; Lee, D.; Choi, Y.; Choi, S.H.; Kang, D.H. Relationships Between Catecholamine Levels and Stress or Intelligence. Neurochem. Res. 2019, 44, 1192–1200.
- Wickramasuriya, D.S.; Qi, C.; Faghih, R.T. A State-Space Approach for Detecting Stress from Electrodermal Activity. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; IEEE: Piscataway, NJ, USA, 2018; Volume 2018, pp. 3562–3567.
- Weissman, D.G.; Mendes, W.B. Correlation of sympathetic and parasympathetic nervous system activity during rest and acute stress tasks. Int. J. Psychophysiol. 2021, 162, 60–68.
- Miyazaki, Y.; Ikei, H.; Song, C. Forest medicine research in Japan. Nihon Eiseigaku Zasshi 2014, 69, 122–135.
- Kudielka, B.M.; Wüst, S. Human models in acute and chronic stress: Assessing determinants of individual hypothalamuspituitaryadrenal axis activity and reactivity. Stress 2010, 13, 1–14.
- De Looff, P.C.; Cornet, L.J.M.; Embregts, P.J.C.M.; Nijman, H.L.I.; Didden, H.C.M. Associations of sympathetic and parasympathetic activity in job stress and burnout: A systematic review. PLoS ONE 2018, 13, e0205741.
- Nagai, Y.; Critchley, H.D.; Featherstone, E.; Trimble, M.R.; Dolan, R.J. Activity in ventromedial prefrontal cortex covaries with sympathetic skin conductance level: A physiological account of a “default mode” of brain function. Neuroimage 2004, 22, 243–251.
- Cohen, S.; Gianaros, P.J.; Manuck, S.B. A Stage Model of Stress and Disease. Perspect. Psychol. Sci. 2016, 11, 456–463.
- Van Puyvelde, M.; Neyt, X.; McGlone, F.; Pattyn, N. Voice stress analysis: A new framework for voice and effort in human performance. Front. Psychol. 2018, 9, 1–25.
- Partila, P.; Tovarek, J.; Rozhon, J.; Jalowiczor, J. Human stress detection from the speech in danger situation. In Mobile Multimedia/Image Processing, Security, and Applications 2019; Agaian, S.S., DelMarco, S.P., Asari, V.K., Eds.; SPIE: Bellingham, WA, USA, 2019; p. 31.
- Tomba, K.; Dumoulin, J.; Mugellini, E.; Khaled, O.A.; Hawila, S. Stress detection through speech analysis. In Proceedings of the ICETE 2018—15th International Joint Conference on e-Business and Telecommunications, Porto, Portugal, 26–28 July 2018; Volume 1, pp. 394–398.
- Dhole, N.P.; Kale, S.N. Stress Detection in Speech Signal Using Machine Learning and AI. In Machine Learning and Information Processing; Springer: Singapore, 2020; pp. 11–26.
- Kurniawan, H.; Maslov, A.V.; Pechenizkiy, M. Stress detection from speech and Galvanic Skin Response signals. In Proceedings of the 26th IEEE International Symposium on Computer-Based Medical Systems, Porto, Portugal, 20–22 June 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 209–214.
- Jiang, L.; Gao, B.; Gu, J.; Chen, Y.; Gao, Z.; Ma, X.; Kendrick, K.M.; Woo, W.L. Wearable Long-Term Social Sensing for Mental Wellbeing. IEEE Sens. J. 2019, 19, 8532–8542.
- Yang, S.; Gao, B.; Jiang, L.; Jin, J.; Gao, Z.; Ma, X.; Woo, W.L. IoT Structured Long-Term Wearable Social Sensing for Mental Wellbeing. IEEE Internet Things J. 2019, 6, 3652–3662.
- Sevil, M.; Rashid, M.; Hajizadeh, I.; Askari, M.R.; Hobbs, N.; Brandt, R.; Park, M.; Quinn, L.; Cinar, A. Discrimination of simultaneous psychological and physical stressors using wristband biosignals. Comput. Methods Programs Biomed. 2021, 199, 105898.
- Lamb, D.H. On the distinction between physical and psychological stressors. Motiv. Emot. 1979, 3, 51–61.
- Matos, T.M.; De Souza-Talarico, J.N. How stress mediators can cumulatively contribute to Alzheimer’s disease An allostatic load approach. Dement. Neuropsychol. 2019, 13, 11–21.
- Juster, R.-P.; Vencill, J.A.; Johnson, P.J. Impact of Stress and Strain on Current LGBT Health Disparities. In Trauma, Resilience, and Health Promotion in LGBT Patients; Springer International Publishing: Cham, Switzerland, 2017; pp. 35–48. ISBN 9783319545097.
- Giakoumis, D.; Tzovaras, D.; Hassapis, G. Subject-dependent biosignal features for increased accuracy in psychological stress detection. Int. J. Hum. Comput. Stud. 2013, 71, 425–439.
- Nasiri Khoozani, E.; Hadzic, M. Designing the human stress ontology: A formal framework to capture and represent knowledge about human stress. Aust. Psychol. 2010, 45, 258–273.
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. J. Psychosom. Res. 1967, 11, 213–218.
- Vavrinský, E.; Stopjaková, V.; Březina, I.; Tvarožek, V.; Majer, L.; Soláriková, P. Electro-optical monitoring of human cognitive processes. In Proceedings of the 2008 International Conference on Advanced Semiconductor Devices and Microsystems, Smolenice, Slovakia, 12–16 October 2008; pp. 279–282.
- Anusha, A.S.; Sukumaran, P.; Sarveswaran, V.; Surees Kumar, S.; Shyam, A.; Akl, T.J.; Preejith, S.P.; Sivaprakasam, M. Electrodermal Activity Based Pre-surgery Stress Detection Using a Wrist Wearable. IEEE J. Biomed. Health Inform. 2020, 24, 92–100.
- Vavrinsky, E.; Solarikova, P.; Stopjakova, V.; Tvarozek, V.; Brezi, I. Implementation of Microsensor Interface for Biomonitoring of Human Cognitive Processes. In Biomedical Engineering, Trends in Electronics, Communications and Software; IntechOpen: London, UK, 2011.
- Zhai, J.; Barreto, A. Stress detection in computer users through non-invasive monitoring of physiological signals. Biomed. Sci. Instrum. 2006, 42, 495–500.
- Ren, P.; Barreto, A.; Huang, J.; Gao, Y.; Ortega, F.R.; Adjouadi, M. Off-line and on-line stress detection through processing of the pupil diameter signal. Ann. Biomed. Eng. 2014, 42, 162–176.
- De Santos Sierra, A.; Sánchez Ávila, C.; Guerra Casanova, J.; Bailador Del Pozo, G. A stress-detection system based on physiological signals and fuzzy logic. IEEE Trans. Ind. Electron. 2011, 58, 4857–4865.
- van den Broek, E.L. Affective Signal Processing (ASP): Unraveling the mystery of emotions, by Egon, L. van den Broek. J. Ambient Intell. Smart Environ. 2012, 4, 67–69.
- Lee, J.; Yoo, S.K. Design of user-customized negative emotion classifier based on feature selection using physiological signal sensors. Sensors 2018, 18, 4253.
- Pinto, G.; Carvalho, J.M.; Barros, F.; Soares, S.C.; Pinho, A.J.; Brás, S. Multimodal emotion evaluation: A physiological model for cost-effective emotion classification. Sensors 2020, 20, 3515.
- Lee, S.; Lee, T.; Yang, T.; Yoon, C.; Kim, S.P. Detection of drivers’ anxiety invoked by driving situations using multimodal biosignals. Processes 2020, 8, 155.
- Posada-Quintero, H.F.; Bolkhovsky, J.B. Machine learning models for the identification of cognitive tasks using autonomic reactions from heart rate variability and electrodermal activity. Behav. Sci. 2019, 9, 45.
- Valdés, A.A. Measurement of Acute Psychological Stress; Universitat Autònoma de Barcelona: Barcelona, Spain, 2017.
- Jimenez-Molina, A.; Retamal, C.; Lira, H. Using psychophysiological sensors to assess mental workload during web browsing. Sensors 2018, 18, 458.
- Cho, D.; Ham, J.; Oh, J.; Park, J.; Kim, S.; Lee, N.K.; Lee, B. Detection of stress levels from biosignals measured in virtual reality environments using a kernel-based extreme learning machine. Sensors 2017, 17, 2435.
- Hui, T.K.L.; Sherratt, R.S. Coverage of emotion recognition for common wearable biosensors. Biosensors 2018, 8, 30.
- Whoop. Available online: (accessed on 4 May 2021).
- Garmin. Available online: (accessed on 4 May 2021).
- Galaxy Watch Active2. Available online: (accessed on 4 May 2021).
- Apple Watch. Available online: (accessed on 4 May 2021).
- Fossil. Available online: (accessed on 4 May 2021).
- Fitbit. Available online: (accessed on 4 May 2021).
- Fitbit Smartwatches. Available online: (accessed on 4 May 2021).
- Scanwatch. Available online: (accessed on 4 May 2021).
- Martin, N.; Mathieu, N.; Pallamin, N.; Ragot, M.; Diverrez, J.-M. Virtual reality sickness detection: An approach based on physiological signals and machine learning. In Proceedings of the 2020 IEEE International Symposium on Mixed and Augmented Reality (ISMAR), Porto de Galinhas, Brazil, 9–13 November 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 387–399.
- Romaniszyn-Kania, P.; Pollak, A.; Danch-Wierzchowska, M.; Kania, D.; Myśliwiec, A.P.; Piętka, E.; Mitas, A.W. Hybrid system of emotion evaluation in physiotherapeutic procedures. Sensors 2020, 20, 6343.
- Empatica. Available online: (accessed on 2 May 2021).
- SIMBAND. Available online: (accessed on 4 May 2021).
- Ouraring HERITAGE—SILVER. Available online: (accessed on 4 May 2021).
- Zephyranywhere. Available online: (accessed on 4 May 2021).
- QARDIO. Available online: (accessed on 4 May 2021).
- Philips: Wearable Biosensor. Available online: (accessed on 5 May 2021).
- Mindtecstore NeuroSky-Brainwave. Available online: (accessed on 4 May 2021).
- Muse-2. Available online: (accessed on 4 May 2021).
- Flowtime. Available online: (accessed on 4 May 2021).
- Spirehealth. Available online: (accessed on 4 May 2021).
- Affanni, A. Wireless Sensors System for Stress Detection by Means of ECG and EDA Acquisition. Sensors 2020, 20, 2026.
- Mohino-Herranz, I.; Gil-Pita, R.; Rosa-Zurera, M.; Seoane, F. Activity recognition using wearable physiological measurements: Selection of features from a comprehensive literature study. Sensors 2019, 19, 5524.
- Slavich, G.M.; Taylor, S.; Picard, R.W. Stress measurement using speech: Recent advancements, validation issues, and ethical and privacy considerations. Stress 2019, 22, 408–413.
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the physiological and biochemical profile of the athlete. NPJ Digit. Med. 2019, 2, 72.
- Zhang, T.; El Ali, A.; Wang, C.; Hanjalic, A.; Cesar, P. Corrnet: Fine-grained emotion recognition for video watching using wearable physiological sensors. Sensors 2021, 21, 52.
- Bizzego, A.; Gabrieli, G.; Furlanello, C.; Esposito, G. Comparison of wearable and clinical devices for acquisition of peripheral nervous system signals. Sensors 2020, 20, 6778.
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart rate variability and cardiac vagal tone in psychophysiological research—Recommendations for experiment planning, data analysis, and data reporting. Front. Psychol. 2017, 8, 1–18.
- Can, Y.S.; Iles-Smith, H.; Chalabianloo, N.; Ekiz, D.; Fernández-Álvarez, J.; Repetto, C.; Riva, G.; Ersoy, C. How to Relax in Stressful Situations: A Smart Stress Reduction System. Healthcare 2020, 8, 100.
- Silva Moreira, P.; Chaves, P.; Dias, R.; Dias, N.; Almeida, P.R. Validation of Wireless Sensors for Psychophysiological Studies. Sensors 2019, 19, 4824.
- Can, Y.S.; Chalabianloo, N.; Ekiz, D.; Ersoy, C. Continuous stress detection using wearable sensors in real life: Algorithmic programming contest case study. Sensors 2019, 19, 1849.
- Chowdhury, A.K.; Tjondronegoro, D.; Chandran, V.; Zhang, J.; Trost, S.G. Prediction of relative physical activity intensity using multimodal sensing of physiological data. Sensors 2019, 19, 4509.
- Vila, G.; Godin, C.; Sakri, O.; Labyt, E.; Vidal, A.; Charbonnier, S.; Ollander, S.; Campagne, A. Real-time monitoring of passenger’s psychological stress. Future Internet 2019, 11, 102.
- Zangróniz, R.; Martínez-Rodrigo, A.; Pastor, J.M.; López, M.T.; Fernández-Caballero, A. Electrodermal activity sensor for classification of calm/distress condition. Sensors 2017, 17, 2324.
- Seoane, F.; Mohino-Herranz, I.; Ferreira, J.; Alvarez, L.; Buendia, R.; Ayllón, D.; Llerena, C.; Gil-Pita, R. Wearable biomedical measurement systems for assessment of mental stress of combatants in real time. Sensors 2014, 14, 7120–7141.
- Chen, J.; Abbod, M.; Shieh, J.S. Pain and stress detection using wearable sensors and devices—A review. Sensors 2021, 21, 1030.
- Betti, S.; Lova, R.M.; Rovini, E.; Acerbi, G.; Santarelli, L.; Cabiati, M.; Del Ry, S.; Cavallo, F. Evaluation of an integrated system of wearable physiological sensors for stress monitoring in working environments by using biological markers. IEEE Trans. Biomed. Eng. 2018, 65, 1748–1758.
- Pourmohammadi, S.; Maleki, A. Stress detection using ECG and EMG signals: A comprehensive study. Comput. Methods Programs Biomed. 2020, 193, 105482.
- Muaremi, A.; Arnrich, B.; Tröster, G. Towards Measuring Stress with Smartphones and Wearable Devices During Workday and Sleep. Bionanoscience 2013, 3, 172–183.
- Nakajima, M.; Lemieux, A.M.; Fiecas, M.; Chatterjee, S.; Sarker, H.; Saleheen, N.; Ertin, E.; Kumar, S.; al’Absi, M. Using novel mobile sensors to assess stress and smoking lapse. Int. J. Psychophysiol. 2020, 158, 411–418.
- Peake, J.M.; Kerr, G.; Sullivan, J.P. A critical review of consumer wearables, mobile applications, and equipment for providing biofeedback, monitoring stress, and sleep in physically active populations. Front. Physiol. 2018, 9, 743.
- Mohr, D.C.; Zhang, M.; Schueller, S.M. Personal Sensing: Understanding Mental Health Using Ubiquitous Sensors and Machine Learning. Annu. Rev. Clin. Psychol. 2017, 13, 23–47.
- Garcia-Ceja, E.; Riegler, M.; Nordgreen, T.; Jakobsen, P.; Oedegaard, K.J.; Tørresen, J. Mental health monitoring with multimodal sensing and machine learning: A survey. Pervasive Mob. Comput. 2018, 51, 1–26.
- Ouraring. Available online: (accessed on 4 May 2021).
- TrendMedic. Available online: (accessed on 4 May 2021).
- Vavrinsky, E.; Stopjakova, V.; Brezina, I.; Majer, L.; Solarikova, P.; Tvarozek, V. Electro-Optical Monitoring and Analysis of Human Cognitive Processes. In Semiconductor Technologies; InTech: London, UK, 2010; pp. 465–490. ISBN 978-953-307-080-3.
- Texas Instruments. Available online: (accessed on 4 May 2021).
- Vavrinsky, E.; Subjak, J.; Donoval, M.; Wagner, A.; Zavodnik, T.; Svobodova, H. Application of Modern Multi-Sensor Holter in Diagnosis and Treatment. Sensors 2020, 20, 2663.
- Asgarian, F.; Najafi, K. Time synchronization in a network of bluetooth low energy beacons. In Proceedings of the SIGCOMM Posters and Demos, Los Angeles, CA, USA, 22–24 August 2017; pp. 119–120.
- Passler, S.; Müller, N.; Senner, V. In-Ear Pulse Rate Measurement: A Valid Alternative to Heart Rate Derived from Electrocardiography? Sensors 2019, 19, 3641.
- Di Rienzo, M.; Rizzo, G.; Işilay, Z.M.; Lombardi, P. SeisMote: A Multi-Sensor Wireless Platform for Cardiovascular Monitoring in Laboratory, Daily Life, and Telemedicine. Sensors 2020, 20, 680.
- Stopjakova, V.; Kovac, M.; Potocny, M. On-chip energy harvesting for implantable medical devices. Radioengineering 2020, 29, 269–284.
- Nagy, G.; Arbet, D.; Stopjakova, V.; Kovac, M. Novel CMOS bulk-driven charge pump for ultra low input voltage. Radioengineering 2016, 25, 321–331.
