The skin is the common coat of the body and is the largest organ of the human organism. Its role is to provide an optimal environment for deeper tissues, by separating them from the external environment, and at the same time ensuring contact with it by exchanging substances and receiving stimuli.
- skin
- microbiome
- internal factors
- external factors
- disinfection
1. Introduction
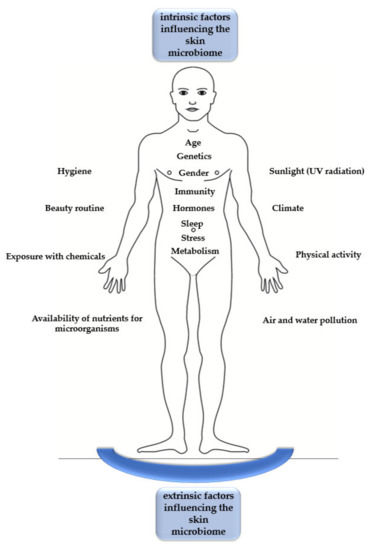
Figure 1. The intrinsic and extrinsic factors that influence the skin microbiome.
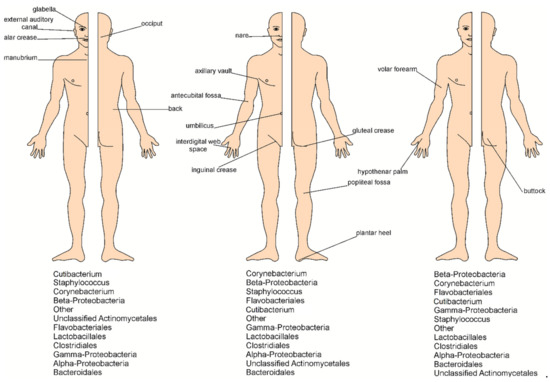
2. Microorganisms Inhabiting the Skin
| Skin Sites | |||||
|---|---|---|---|---|---|
| Moist | Sebaceous | Dry | Foot | ||
| Body sites location |
groin, axilla, antecubital fossa, toe web | face, chest, back, | arm, leg, volar forearm | Moist—toe interdigital web space dry—plantar heel |
|
| Fungi | Malassezia spp. | 36% CH–80%AD | 65% CH–99%AD | 35% CH–83%AD | 53–80% |
| Other fungi | Ascomycota: Aspergillus, Epicoccum, Phoma (levels >5%): 9.5%AD–40.2%CH Cladosporium, Cryptococcus | Cryptococcus, Aspergillus, Rhodotorula, Epicoccum, Saccharomyces, Candida, Epidermophyton Microsporum, Trichophyton | |||
3. Interactions between Skin Microorganisms
The dominant resident species of skin bacteria are commensals. Together with immune cells and keratinized skin cells (replaced every four weeks), these are responsible for the appropriate skin immune barrier functioning [3][10]. There are diverse mechanisms of skin immune system support that are associated with the activity of the microorganisms. While a properly functioning microbiome of healthy skin supports the body’s immune barrier, its transition into a dysbiosis state may lead to numerous systemic disorders. Dysbiosis, which is a disturbance of the structural and functional balance of the normal microbiome, is caused by internal and external stressors. Factors used in the fight against dysbiosis and helping to restore the balance of the skin microbiota include the use of probiotics and prebiotics. Dysbiosis alters the proportions of organisms in the healthy skin microbiome and may trigger the pathogenic potential of the commensals. Examples of diseases associated with the skin microbiome composition disturbance include acne, atopic dermatitis (AD), and dandruff [11].
4. Skin Disinfection and Its Influence on the Microbiome Condition
5. Summary
This entry is adapted from the peer-reviewed paper 10.3390/microorganisms9030543
References
- Richard L. Gallo; Human Skin Is the Largest Epithelial Surface for Interaction with Microbes. Journal of Investigative Dermatology 2017, 137, 1213-1214, 10.1016/j.jid.2016.11.045.
- Elizabeth Grice; Julia A. Segre; The skin microbiome. Nature Reviews Genetics 2011, 9, 244-253, 10.1038/nrmicro2537.
- Anthony M. Cundell; Microbial Ecology of the Human Skin. Microbial Ecology 2016, 76, 113-120, 10.1007/s00248-016-0789-6.
- Allyson L. Byrd; Yasmine Belkaid; Julia A. Segre; The human skin microbiome. Nature Reviews Genetics 2018, 16, 143-155, 10.1038/nrmicro.2017.157.
- Cheng, J.; Hata, T. . Dysbiosis of the Skin Microbiome in Atopic Dermatitis. ; Dayan, N., Eds.; Scrivener Publishing LLC: Beverly, MA, USA, 2020; pp. 185-201.
- Andersen, B.M.. Prevention and Control of Infections in Hospitals: Practice and Theory; Springer Nature: Switzerland, 2018; pp. 337–437.
- Elizabeth Grice; Heidi Kong; Sean Conlan; Clayton B. Deming; Joie Davis; Alice C. Young; Gerard G. Bouffard; Robert W. Blakesley; Patrick R. Murray; Eric D. Green; et al. Topographical and Temporal Diversity of the Human Skin Microbiome. Science 2009, 324, 1190-1192, 10.1126/science.1171700.
- Nathalia Murillo; Didier Raoult; Skin microbiota: overview and role in the skin diseases acne vulgaris and rosacea. Future Microbiology 2013, 8, 209-222, 10.2217/fmb.12.141.
- Buerger, S. . The Skin and Oral Microbiome: An Examination of Overlap and Potential Interactions between Microbiome Communities.; Scrivener Publishing LLC: Beverly, MA, USA, 2020; pp. 45-58.
- Mohammad Asif Sherwani; Saba Tufail; Anum Fatima Muzaffar; Nabiha Yusuf; The skin microbiome and immune system: Potential target for chemoprevention?. Photodermatology, Photoimmunology & Photomedicine 2017, 34, 25-34, 10.1111/phpp.12334.
- Farahmand, S.. Microbiome of Compromised Skin.; Scrivener Publishing LLC: Beverly, MA, USA, 2020; pp. 145–170.
- Qianyu Lin; Jason Y. C. Lim; Kun Xue; Pek Yin Michelle Yew; Cally Owh; Pei Lin Chee; Xian Jun Loh; Sanitizing agents for virus inactivation and disinfection. View 2020, 1, e16, 10.1002/viw2.16.
