Obesity is a prevalent disease worldwide, usually associated with infertility. Studies in obese infertile females show the occurrence of systemic hyperestrogenemia, hyperinsulinemia, and associated ovarian dysfunction through premature follicular atresia and anovulation [1]. Indeed, the ovaries of obese mothers have been shown to accumulate lipids, high levels of reactive oxygen species [2], and inflammatory mediators [3]. Furthermore, obesity has been shown to hamper not only oocyte maturation and quality [4] but also embryo development [5], with reported long term effects and direct causality between obesity in the mother and prevalence of cardiovascular disease or cancer in the offspring.
- leptin
- obesity
- ovary
- folliculogenesis
- oocyte
1. Introduction
The worldwide epidemic of obesity has reached unprecedented levels and infertility is described as an associated comorbidity [1]. Indeed, obese women were linked to poor reproductive outcomes, such as anovulation or decreased conception rate [7]. Literature has evidenced the link between peripheral insulin resistance and functional hyperandrogenism and hyperestrogenism [8], the main causes of anovulation and reduced endometrial receptivity [1]. Studies in mice have shown how obesity-associated hyperinsulinemia and diabetes can lead to delayed oocyte maturation in preovulatory follicles and apoptosis in granulosa cells (GC) [9]. Furthermore, ovaries of obese women were shown to present high levels of androstenedione and testosterone [8], responsible for premature follicular atresia. Therefore, the endocrine imbalance observed in obese mothers affects directly the follicular pool, reducing the number of primordial follicles and compromising fertility [10].
2. Leptin—A Common Denominator between Ovarian Function and Obesity
During obesity progression, the ever-growing adipose tissue secretes large amounts of leptin, which causes systemic hormonal imbalance. Leptin is mainly known to regulate appetite at the central level [15] besides modulating the release of gonadotropin releasing hormone (GnRH) neuron activity and gonadotropins [16]. Nonetheless, leptin is also an important modulator of ovarian function [17]. Leptin long and short receptor isoforms were detected in most cell types in murine ovary, particularly in the oocyte [17]. Likewise, both isoforms of the leptin receptor (ObR) were previously detected in human GC and theca cells (TC) [18]; as well, leptin and leptin soluble receptor were detected in human follicular fluid [18,19]. Thus, leptin signaling components’ heavy representation in the ovary makes the organ particularly vulnerable to the systemic hyperleptinemia observed in obese mothers [20].
Concerning the role of leptin in the ovary, evidence gathered from studies with leptin or ObR deficient mice, as well as women, confirmed their infertility and altered pubertal development [24,25]. Functionally, leptin actions in the ovary were shown to have a bimodal nature. In vivo and in vitro studies in mouse ovarian explants [26] evidenced the dose-dependent effect of leptin on progesterone (P4) synthesis, with low doses stimulating and high doses inhibiting expression of enzymes involved in P4 synthesis [26]. Also, studies in other species corroborated the aforementioned observations as the in vitro treatment of equine luteal cells with lower doses of leptin supported P4 secretion, whereas higher doses presented no effect [27]. Particularly regarding follicular dynamics, studies in mice showed that high levels of circulating leptin blocked folliculogenesis, but lower circulating levels of leptin supported the transition from primary to secondary follicle [28]. Conversely, the in vitro treatment of mouse follicles with mouse recombinant leptin once more revealed a dose-dependent response with higher treatment doses inhibiting follicular growth [29]. Presently, we used the data from Zhang and co-workers’ recent report profiling the transcriptome of GC and oocytes isolated from different stages of folliculogenesis in women [30] and plotted the main components of the leptin signaling pathway in order to understand if their expression profile could be linked to a leptin concerted role during particular developmental stages. Indeed, we confirmed some leptin signaling components, such as ptyrosine phosphatase non-receptor type 2 (PTPN2), protein tyrosine phosphatase (PTP) 1B, or STAT3, were abundantly transcribed in both oocytes and GCs throughout folliculogenesis, whereas others, such as SOCS3, presented very low expression in both cell types under physiological conditions, particularly in later stages of folliculogenesis (Figure 1). Finally, we have recently shown that obesity progression in DIO mice alters leptin signaling in the ovary with increased leptin signaling in the ovary of 4 wk DIO mice, being followed by the establishment of leptin resistance in the ovaries of 16 wk DIO mice [6]. Indeed, expression levels of SOCS3 in ovarian extracts were dramatically increased already at 4 wk DIO [6]. Therefore, our findings, as well as the observations on leptin signaling component expression in oocytes and GCs from women’s follicles, clearly suggest that the impairment of leptin signaling in the ovaries of obese mothers may contribute to pathogenesis of ovarian failure, particularly given leptin’s established role in ovarian function.
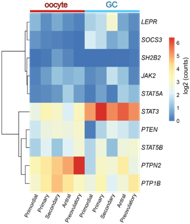
Figure 1. Heatmap representing the expression level of transcripts from the leptin signaling pathway components in human oocyte and granulosa cells (GC) throughout folliculogenesis. Primordial = primordial follicle; Primary = primary follicle; Secondary = secondary follicle; Antral = antral follicle; Preovulatory = preovulatory follicle. Color code from blue to red indicates the relative gene expression level from low to high, respectively. Data from Zhang et al. 2018 [30]. Leptin receptor (LEPR), suppressor of cytokine signaling 3 (SOCS3), SH2B Adaptor Protein 1 (SH2B1), Janus kinase 2 (JAK2), signal transducer and activator of transcription (STAT), protein tyrosine phosphatase non-receptor type 2 (PTPN2), protein tyrosine phosphatase (PTP) 1B.
3. Ovarian Function in Obese Mothers
The complex nature of folliculogenesis regulation certainly accounts for the vulnerability the ovaries present to the hormonal imbalance seen in obese mothers [7]. Generally, obesity may affect the oocyte and somatic cells at each single developmental stage of folliculogenesis (Figure 3) with the incidence of obesity earlier in life posing a greater threat for the quality of the gamete later in adulthood [41]. Hence, in this section, we revisit folliculogenesis, analyzing major cellular events taking place throughout the long journey the female gamete makes from primordial follicle until fertilization, based on lessons learnt from studies in mice and in humans.
3.1 Obesity and Primordial Follicle Activation
Studies in rodents have highlighted the effects of maternal obesity on ovarian failure and, particularly, on PI3K dysregulation. A report in rats showed that DIO treatment led to POF through activation of mTOR and suppression of sirtuin (SIRT) 1 signaling [67], whereas the ovaries of mice fed a high-fat diet (HFD) presented aberrant expression levels of PI3K pathway components [68]. Indeed, the putative crosstalk between leptin and the PI3K pathway can be anticipated, mainly, through components of the insulin signaling cascade (Figure 2). After ObRb activation, JAK2 can phosphorylate IRs, with subsequent activation of PI3K pathway [21]. This generates PIP3, which further activates PIP3-dependent serine/threonine kinases, such as PDK1,2, responsible for activation of Akt, as previously discussed (Figure 1) [21]. Indeed, a study in mice with a triple mutation in ObR tyrosines linked follicle loss to the activation of PTEN/PI3K/Akt/mTOR signaling [69]. Furthermore, Panwar and colleagues showed the direct effects of leptin on the follicular pool once passive immunization of prepubertal mice against leptin prompted the transition of primordial to primary follicles [28]. Therefore, adequate levels of leptin signaling in the ovary seem to prevent primordial follicle hyperactivation and help to maintain the follicular pool. Concordantly, these observations suggest the decrease in leptin signaling we have reported in the ovaries of 16 wk DIO mice [6] might accelerate the activation and depletion of the primordial follicle pool.
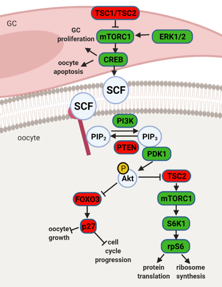
Figure 2. Schematic representation of mammalian target of rapamycin (mTOR) and phosphatidylinositol 3 kinase (PI3K) signaling pathway and its downstream regulators in the granulosa cells (GC) and oocyte. Extracellular signal-regulated protein kinase ½ (ERK1/2) activates mTOR complex 1 (mTORC1) in pre-GC to initiate the activation of primordial follicles. mTORC1 activates cyclic AMP-response element binding protein (CREB), which promotes stem cell factor (SCF) transcription and stimulates PI3K signaling but also affects pre-GC proliferation and oocyte apoptosis. mTOR signaling negative regulators TSC1 and TSC2 suppress mTORC1 activity. PI3K signaling pathway is activated by SCF in the oocyte. PI3K phosphorylates phosphatidylinositol-4,5-biphosphate (PIP2) to phosphatidylinositol-3,4,5-triphosphate (PIP3), which interacts with 3-phosphoinositide dependent protein kinase 1 (PDK1) for subsequent phosphorylation of protein kinase B (Akt) and forkhead box O3 (FOXO3) with its downstream mediator, cyclin-dependent kinase inhibitor 1B (p27). Upon phosphorylation, the inhibitory effect of FOXO3 and p27 on cell cycle progression and oocyte growth is inhibited, and the primordial follicle is recruited. Akt also activates ribosomal protein S6 kinase beta-1 (S6K1) through inhibition of TSC2 with subsequent mTORC1 activation and further ribosomal protein S6 (rpS6) phosphorylation, which leads to protein translation and ribosome synthesis. Factors indicated in red are associated with follicle dormancy; molecules indicated in green are associated with follicle activation. Created with BioRender.com.
3.2 Obesity and Preovulatory Follicle Formation
Obesity has been strongly associated with increased circulating levels of both E2 and androgens, not only due to the ability of the adipose tissue to synthesize steroids [105] but also to low circulating sex hormone binding globulin levels and suppression of gonadotropin release. Moreover, ovarian TC are known to respond to insulin during androgen synthesis [1]. Seminal work by Wu and co-workers clearly showed the link between hyperinsulinemia in DIO mice and increased ovarian androgen production through hyperactivation of CYP17 at TC level [106]. On the other hand, Souter et al. also correlated gain in body mass index (BMI) with E2 secretion by preovulatory follicles in obese women [107]. Finally, studies in rats evidenced the link between obesity and the lack of preovulatory surge of P4 and LH [108]. Hence, obesity clearly disrupts steroidogenesis, causing a predisposition to premature follicular atresia and anovulation.
3.3 Oocyte Maturation and Early Embryo Development in Obese Mothers
Obesity leads to severe systemic hormonal imbalance with drastic consequences for oocyte maturation and embryo development. Firstly, maternal obesity was shown to alter insulin, glucose, and free fatty acid concentration in follicular fluid, directly affecting oocyte metabolism and reducing oocyte maturation [142]. Secondly, insulin-stimulated glucose uptake was shown to be impaired in CC isolated from mice treated with HFD, suggesting the establishment of insulin-resistance [143]. Indeed, activation of the polyol pathway during hyperglycemia was shown to negatively affect metabolism and CC–oocyte communication [144]. As a result, in obese mothers, oocyte maturation, fertilization rate, and embryo quality were significantly decreased [145]. Moreover, oocytes derived from obese mice after in vitro fertilization and culture presented reduced development [145]. Furthermore, studies in mice clearly linked maternal obesity with oocyte and zygote increased mitochondrial potential, mitochondrial DNA content and biogenesis, and generation of reactive oxygen species (ROS) [2]. Importantly, the absence of mitophagy was presented as the main cause of mitochondrial dysfunction in oocytes and early embryos from obese mothers [12]. Another recent report also linked lack of expression of Stella in oocytes from obese mice with increased hydromethylation in the zygote and DNA instability [5]. Thus, obesity can drastically affect both oocyte and embryo quality.
4 . Conclusions
Folliculogenesis regulation is a complex process that depends on the crosstalk between local and systemic factors, accounting, therefore, for its vulnerability to maternal physiological fitness. Indeed, leptin, an established local regulator of folliculogenesis, presents increased circulating levels in obese mothers with major consequences for follicular activation, recruitment, and growth. In addition to increased ovarian ObRb activation and altered leptin signaling, deleterious effects of systemic hyperleptinemia during obesity can also result from local overexpression of mediators of leptin resistance, such as SOCS3. As a result, leptin’s prominent role as suppressor of follicular pool activation can be affected in obese mothers, with consequent POF. During preovulatory follicle formation, altered leptin signaling affects not only steroidogenesis but the communication between GC and oocyte, which is known to be key for antrum formation and oocyte growth. Finally, changes in leptin signaling and impaired metabolism may also incur drastic consequences for oocyte maturation, hampering meiosis resumption and cytoplasmic maturation (Figure 6). Hence, advances in our understanding of the role of leptin on ovarian pathophysiology during obesity should unravel innovative tools to monitor the quality of the oocyte during disease progression, potentially preventing pregnancy failure and ensuring the birth of a healthy offspring.
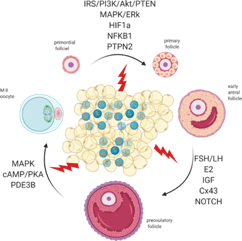
Figure 3. Adipose tissue secretes excessive amounts of leptin (L) during obesity. Leptin signaling in the ovaries of obese mothers is altered, culminating with the establishment of leptin resistance. As a result, signaling pathways governing primordial follicle activation, preovulatory follicle formation, and oocyte maturation can be affected. Created with BioRender.com.
References
- Gambineri, ; Laudisio, D.; Marocco, C.; Radellini, S.; Colao, A.; Savastano, S. Female infertility: Which role for obesity? Int. J. Obes. Suppl. 2019, 9, 65–72, doi:10.1038/s41367-019-0009-1.
- Igosheva, ; Abramov, A.Y.; Poston, L.; Eckert, J.J.; Fleming, T.P.; Duchen, M.R.; McConnell, J. Maternal Diet-Induced Obesity Alters Mitochondrial Activity and Redox Status in Mouse Oocytes and Zygotes. PLoS ONE 2010, 5, e10074.
- Robker, L.; Wu, L.L.-Y.; Yang, X. Inflammatory pathways linking obesity and ovarian dysfunction. J. Reprod. Immunol. 2011, 88, 142–148, doi:10.1016/j.jri.2011.01.008.
- Yang, ; Wu, L.L.; Chura, L.R.; Liang, X.; Lane, M.; Norman, R.J.; Robker, R.L. Exposure to lipid-rich follicular fluid is associated with endoplasmic reticulum stress and impaired oocyte maturation in cumulus-oocyte complexes. Fertil. Steril. 2012, 97, 1438–1443, doi:10.1016/j.fertnstert.2012.02.034.
- Han, ; Ren, C.; Li, L.; Li, X.; Ge, J.; Wang, H.; Miao, Y.-L.; Guo, X.; Moley, K.H.; Shu, W.; et al. Embryonic defects induced by maternal obesity in mice derive from Stella insufficiency in oocytes. Nat. Genet. 2018, 50, 432–442, doi:10.1038/s41588-018-0055-6.
- Wołodko, ; Walewska, E.; Adamowski, M.; Castillo-Fernandez, J.; Kelsey, G.; Galvão, A. Leptin Resistance in the Ovary of Obese Mice is Associated with Profound Changes in the Transcriptome of Cumulus Cells. Cell. Physiol. Biochem. 2020, 54, 417–437, doi:10.33594/000000228.
- Dag, O.; Dilbaz, B. Impact of obesity on infertility in women. J. Turk. Gynecol. Assoc. 2015, 16, 111–117, doi:10.5152/jtgga.2015.15232.
- Cree-Green, ; Newcomer, B.R.; Coe, G.; Newnes, L.; Baumgartner, A.; Brown, M.S.; Pyle, L.; Reusch, J.E.; Nadeau, K.J. Peripheral insulin resistance in obese girls with hyperandrogenism is related to oxidative phosphor-ylation and elevated serum free fatty acids. Am. J. Physiol. Metab. 2015, 308, E726–E733.
- Chang, S.; Dale, A.N.; Moley, K.H. Maternal Diabetes Adversely Affects Preovulatory Oocyte Maturation, Development, and Granulosa Cell Apoptosis. Endocrinology 2005, 146, 2445–2453, doi:10.1210/en.2004-1472.
- Skaznik-Wikiel, E.; Swindle, D.C.; Allshouse, A.A.; Polotsky, A.J.; McManaman, J.L. High-Fat Diet Causes Subfertility and Compromised Ovarian Function Independent of Obesity in Mice1. Biol. Reprod. 2016, 94, 108, doi:10.1095/biolreprod.115.137414.
- Wu, L.-Y.; Dunning, K.R.; Yang, X.; Russell, D.L.; Lane, M.; Norman, R.J.; Robker, R.L. High-Fat Diet Causes Lipotoxicity Responses in Cumulus–Oocyte Complexes and Decreased Fertilization Rates. Endocrinology 2010, 151, 5438–5445, doi:10.1210/en.2010-0551.
- Boudoures, L.; Saben, J.; Drury, A.; Scheaffer, S.; Modi, Z.; Zhang, W.; Moley, K.H. Obesity-exposed oocytes accumulate and transmit damaged mitochondria due to an inability to activate mitophagy. Dev. Biol. 2017, 426, 126–138, doi:10.1016/j.ydbio.2017.04.005.
- Hou, -J.; Zhu, C.-C.; Duan, X.; Liu, H.-L.; Wang, Q.; Sun, S.-C. Both diet and gene mutation induced obesity affect oocyte quality in mice. Sci. Rep. 2016, 6, srep18858, doi:10.1038/srep18858.
- Robker, L.; Akison, L.K.; Bennett, B.D.; Thrupp, P.N.; Chura, L.R.; Russell, D.L.; Lane, M.; Norman, R.J. Obese Women Exhibit Differences in Ovarian Metabolites, Hormones, and Gene Expression Compared with Moderate-Weight Women. J. Clin. Endocrinol. Metab. 2009, 94, 1533–1540, doi:10.1210/jc.2008-2648.
- Vaisse, ; Halaas, J.L.; Horvath, C.M.; Darnell, J.E.; Stoffel, M.; Friedman, J.M. Leptin activation of Stat3 in the hypothalamus of wild–type and ob/ob mice but not db/db mice. Nat. Genet. 1996, 14, 95–97, doi:10.1038/ng0996-95.
- Odle, K.; Akhter, N.; Syed, M.M.; Allensworth-James, M.L.; Beneš, H.; Castillo, A.I.M.; MacNicol, M.C.; MacNicol, A.M.; Childs, G.V. Leptin Regulation of Gonadotrope Gonadotropin-Releasing Hormone Receptors As a Metabolic Checkpoint and Gateway to Reproductive Competence. Front. Endocrinol. 2018, 8, 367, doi:10.3389/fendo.2017.00367.
- Ryan, K.; Woodhouse, C.M.; Van Der Hoek, K.H.; Gilchrist, R.B.; Armstrong, D.T.; Norman, R.J. Expression of leptin and its receptor in the murine ovary: Possible role in the regulation of oocyte maturation. Biol. Reprod. 2002, 66, 1548–1554, doi:10.1095/biolreprod66.5.1548.
- Karlsson, ; Lindell, K.; Svensson, E.; Bergh, C.; Lind, P.; Billig, H.; Carlsson, L.M.; Carlsson, B. Expression of Functional Leptin Receptors in the Human Ovary 1. J. Clin. Endocrinol. Metab. 1997, 82, 4144–4148.
- Welt, K.; Schneyer, A.L.; Heist, K.; Mantzoros, C.S. Leptin and Soluble Leptin Receptor in Follicular Fluid. J. Assist. Reprod. Genet. 2003, 20, 495–501, doi:10.1023/b:jarg.0000013649.38415.2a.
- Maffei, ; Halaas, J.L.; Ravussin, E.; Pratley, R.E.; Lee, G.; Zhang, Y.; Fei, H.; Kim, S.; Lallone, R.; Ranganathan, S.; et al. Leptin levels in human and rodent: Measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat. Med. 1995, 1, 1155–1161, doi:10.1038/nm1195-1155.
- Hegyi, ; Fülöp, K.; Kovacs, K.; Tóth, S.; Falus, A. Leptin-induced signal transduction pathways. Cell Biol. Int. 2004, 28, 159–169, doi:10.1016/j.cellbi.2003.12.003.
- Bjørbæk, ; Uotani, S.; da Silva, B.; Flier, J.S. Divergent Signaling Capacities of the Long and Short Isoforms of the Leptin Receptor. J. Biol. Chem. 1997, 272, 32686–32695, doi:10.1074/jbc.272.51.32686.
- Bjørbæk, ; Buchholz, R.M.; Davis, S.M.; Bates, S.H.; Pierroz, D.D.; Gu, H.; Neel, B.G.; Jr., M.G.M.; Flier, J.S. Divergent Roles of SHP-2 in ERK Activation by Leptin Receptors. J. Biol. Chem. 2001, 276, 4747–4755, doi:10.1074/jbc.m007439200.
- Clément, ; Vaisse, C.; Lahlou, N.; Cabrol, S.; Pelloux, V.; Cassuto, D.; Gourmelen, M.; Dina, C.; Chambaz, J.; Lacorte, J.-M.; et al. A mutation in the human leptin receptor gene causes obesity and pituitary dysfunction. Nat. Cell Biol. 1998, 392, 398–401, doi:10.1038/32911.
- Tu, ; Kuang, Z.; Gong, X.; Shi, Y.; Yu, L.; Shi, H.; Wang, J.; Sun, Z. The Influence of LepR Tyrosine Site Mutations on Mouse Ovary Development and Related Gene Expression Changes. PLoS ONE 2015, 10, e0141800, doi:10.1371/journal.pone.0141800.
- Bilbao, G.; Di Yorio, M.P.; Faletti, A.G. Different levels of leptin regulate different target enzymes involved in proges-terone synthesis. Fertil. Steril. 2013, 99, 1460–1466.
- Galvão, ; Tramontano, A.; Rebordão, M.R.; Amaral, A.; Bravo, P.P.; Szóstek, A.; Skarzynski, D.; Mollo, A.; Ferreira-Dias, G. Opposing Roles of Leptin and Ghrelin in the Equine Corpus Luteum Regulation: An In Vitro Study. Mediat. Inflamm. 2014, 2014, 1–13, doi:10.1155/2014/682193.
- Panwar, ; Herrid, M.; Kauter, K.G.; McFarlane, J.R. Effect of passive immunization against leptin on ovarian follicular development in prepubertal mice. J. Reprod. Immunol. 2012, 96, 19–24, doi:10.1016/j.jri.2012.07.004.
- Swain, E.; Dunn, R.L.; McConnell, D.; Gonzalez-Martinez, J.; Smith, G.D. Direct Effects of Leptin on Mouse Reproductive Function: Regulation of Follicular, Oocyte, and Embryo Development. Biol. Reprod. 2004, 71, 1446–1452, doi:10.1095/biolreprod.104.033035.
- Zhang, ; Yan, Z.; Qin, Q.; Nisenblat, V.; Chang, H.-M.; Yu, Y.; Wang, T.; Lu, C.; Yang, M.; Yang, S.; et al. Transcriptome Landscape of Human Folliculogenesis Reveals Oocyte and Granulosa Cell Interactions. Mol. Cell 2018, 72, 1021–1034.e4, doi:10.1016/j.molcel.2018.10.029.
- Campos, B.; Palin, M.F.; Bordignon, V.; Murphy, B.D. The ‘beneficial’ adipokines in reproduction and fertility. Ternational J. Obes. 2008, 32, 223–231.
- Chen, ; Jia, X.; Qiao, J.; Guan, Y.; Kang, J. Adipokines in reproductive function: A link between obesity and polycystic ovary syndrome. J. Mol. Endocrinol. 2013, 50, R21–R37, doi:10.1530/jme-12-0247.
- Stern, H.; Rutkowski, J.M.; Scherer, P.E. Adiponectin, Leptin, and Fatty Acids in the Maintenance of Metabolic Ho-meostasis through Adipose Tissue Crosstalk. Cell Metab. 2016, 23, 770–784.
- Di Carlo, ; Tommaselli, G.A.; De Filippo, E.; Pisano, G.; Nasti, A.; Bifulco, G.; Contaldo, F.; Nappi, C. Menstrual status and serum leptin levels in anorectic and in menstruating women with low body mass indexes. Fertil. Steril. 2002, 78, 376–382, doi:10.1016/s0015-0282(02)03221-1.
- Richards, S.; Liu, Z.; Kawai, T.; Tabata, K.; Watanabe, H.; Suresh, D.; Kuo, F.-T.; Pisarska, M.D.; Shimada, M. Adiponectin and its receptors modulate granulosa cell and cumulus cell functions, fertility, and early embryo development in the mouse and human. Fertil. Steril. 2012, 98, 471–479.e1, doi:10.1016/j.fertnstert.2012.04.050.
- Maillard, ; Uzbekova, S.; Guignot, F.; Perreau, C.; Ramé; C.; Coyral-Castel, S.; Dupont, J. Effect of adiponectin on bovine granulosa cell steroidogenesis, oocyte maturation and embryo devel-opment. Reprod. Biol. Endocrinol. 2010, 8, 1–15.
- Zhuo, ; Hua, L.; Feng, B.; Jiang, X.; Li, J.; Jiang, D.; Huang, X.; Zhu, Y.; Li, Z.; Yan, L.; et al. Fibroblast growth factor 21 coordinates adiponectin to mediate the beneficial effects of low-protein diet on primordial follicle reserve. EBioMedicine 2019, 41, 623–635, doi:10.1016/j.ebiom.2019.02.020.
- Zieba, ; Biernat, W.; Barć, J. Roles of leptin and resistin in metabolism, reproduction, and leptin resistance. Domest. Anim. Endocrinol. 2020, 73, 106472, doi:10.1016/j.domaniend.2020.106472.
- Biernat, ; Kirsz, K.; Szczesna, M.; Zieba, D.A. Resistin regulates reproductive hormone secretion from the ovine ade-nohypophysis depending on season. Domest. Anim. Endocrinol. 2018, 65, 95–100.
- Estienne, ; Bongrani, A.; Reverchon, M.; Ramé, C.; Ducluzeau, P.-H.; Froment, P.; Dupont, J. Involvement of Novel Adipokines, Chemerin, Visfatin, Resistin and Apelin in Reproductive Functions in Normal and Pathological Conditions in Humans and Animal Models. Int. J. Mol. Sci. 2019, 20, 4431, doi:10.3390/ijms20184431.
- He, ; Tian, J.; Blizzard, L.; Oddy, W.H.; Dwyer, T.; Bazzano, L.A.; Hickey, M.; Harville, E.W.; Venn, A.J. Associations of childhood adiposity with menstrual irregularity and polycystic ovary syndrome in adulthood: The Childhood Determinants of Adult Health Study and the Bogalusa Heart Study. Hum. Reprod. 2020, 35, 1185–1198, doi:10.1093/humrep/deaa069.
- Monk, ; McLaren, A. X-chromosome activity in foetal germ cells of the mouse. J. Embryol. Exp. Morphol. 1981, 63, 75–84.
- Borum, Oogenesis in the mouse. A study of the origin of the mature ova. Exp. Cell Res.1967, 45, 39–47.
- Pepling, E.; Spradling, A.C. Mouse Ovarian Germ Cell Cysts Undergo Programmed Breakdown to Form Primordial Follicles. Dev. Biol. 2001, 234, 339–351, doi:10.1006/dbio.2001.0269.
- Pepling, E.; A. Sundman, E.; Patterson, N.L.; Gephardt, G.W.; Medico, L.; Wilson, K.I. Differences in oocyte development and estradiol sensitivity among mouse strains. Reproduction 2010, 139, 349–357, doi:10.1530/rep-09-0392.
- Baerwald, R.; Adams, G.P.; Pierson, R.A. Ovarian antral folliculogenesis during the human menstrual cycle: A review. Hum. Reprod. Updat. 2011, 18, 73–91, doi:10.1093/humupd/dmr039.
- Peters, ; Byskov, A.; Grinsted, J. Follicular growth in fetal and prepubertal ovaries of humans and other primates. Clin. Endocrinol. Metab. 1978, 7, 469–485, doi:10.1016/s0300-595x(78)80005-x.
- Skinner, K. Regulation of primordial follicle assembly and development. Hum. Reprod. Updat. 2005, 11, 461–471, doi:10.1093/humupd/dmi020.
- Jamnongjit, ; Hammes, S.R. Oocyte Maturation: The Coming of Age of a Germ Cell. Semin. Reprod. Med. 2005, 23, 234–241, doi:10.1055/s-2005-872451.
- McGee, A.; Hsueh, A.J.W. Initial and Cyclic Recruitment of Ovarian Follicles. Endocr. Rev. 2000, 21, 200–214, doi:10.1210/edrv.21.2.0394.
- Kaipia, ; Hsueh, A.J.W. Regulation of ovarian follicle atresia. Annu. Rev. Physiol. 1997, 59, 349–363, doi:10.1146/annurev.physiol.59.1.349.
- Faddy, J.; Gosden, R.G.; Edwards, R.G. Ovarian follicle dynamics in mice: A comparative study of three inbred strains and an F1 hybrid. J. Endocrinol. 1983, 96, 23–33, doi:10.1677/joe.0.0960023.
- Findlay, K.; Hutt, K.J.; Hickey, M.; Anderson, R.A. How Is the Number of Primordial Follicles in the Ovarian Reserve Established? Biol. Reprod. 2015, 93, 111, doi:10.1095/biolreprod.115.133652.
- Tsafriri, ; Reich, R.; Abisogun, A.O. The Ovarian Egg and Ovulation. Marshall’s Physiol. Reprod. .
- Guzeloglu-Kayisli, ; Basar, M.; Arici, A. Basic aspects of implantation. Reprod. Biomed. Online 2007, 15, 728–739, doi:10.1016/s1472-6483(10)60541-x.
- Fortune, ; Cushman, R.; Wahl, C.; Kito, S. The primordial to primary follicle transition. Mol. Cell. Endocrinol. 2000, 163, 53–60, doi:10.1016/s0303-7207(99)00240-3.
- Li, ; Zhang, Y.; Zheng, N.; Li, B.; Yang, J.; Zhang, C.; Xia, G.; Zhang, M. CREB activity is required for mTORC1 signaling-induced primordial follicle activation in mice. Histochem. Cell Biol. 2020, 154, 287–299, doi:10.1007/s00418-020-01888-4.
- Castrillon, H.; Miao, L.; Kollipara, R.; Horner, J.W.; Depinho, R.A. Suppression of Ovarian Follicle Activation in Mice by the Transcription Factor Foxo3a. Science 2003, 301, 215–218, doi:10.1126/science.1086336.
- Reddy, ; Adhikari, D.; Zheng, W.; Liang, S.; Hämäläinen, T.; Tohonen, V.; Ogawa, W.; Noda, T.; Volarevic, S.; Huhtaniemi, I.; et al. PDK1 signaling in oocytes controls reproductive aging and lifespan by manipulating the survival of pri-mordial follicles. Hum. Mol. Genet. 2009, 18, 2813–2824.
- Reddy, ; Liu, L.; Adhikari, D.; Jagarlamudi, K.; Rajareddy, S.; Shen, Y.; Du, C.; Tang, W.; La Inen, T.H.M.; Peng, S.L.; et al. Oocyte-Specific Deletion of Pten Causes Premature Activation of the Primordial Follicle Pool. Science 2008, 319, 611–613, doi:10.1126/science.1152257.
- Adhikari, ; Zheng, W.; Shen, Y.; Gorre, N.; Hämäläinen, T.; Cooney, A.J.; Huhtaniemi, I.; Lan, Z.-J.; Liu, K. Tsc/mTORC1 signaling in oocytes governs the quiescence and activation of primordial follicles. Hum. Mol. Genet. 2009, 19, 397–410, doi:10.1093/hmg/ddp483.
- Li, ; Kawamura, K.; Cheng, Y.; Liu, S.; Klein, C.; Duan, E.-K.; Hsueh, A.J.W. Activation of dormant ovarian follicles to generate mature eggs. Proc. Natl. Acad. Sci. USA 2010, 107, 10280–10284, doi:10.1073/pnas.1001198107.
- Ding, ; Wang, W.; Zhou, B.; Zhang, W.; Huang, P.; Shi, F.; Taya, K. Formation of Primordial Follicles and Immunolocalization of PTEN, PKB and FOXO3A Proteins in the Ovaries of Fetal and Neonatal Pigs. J. Reprod. Dev. 2010, 56, 162–168, doi:10.1262/jrd.09-094h.
- Dong, ; Albertini, D.F.; Nishimori, K.; Kumar, T.R.; Lu, N.; Matzuk, M.M. Growth differentiation factor-9 is required during early ovarian folliculogenesis. Nat. Cell Biol. 1996, 383, 531–535, doi:10.1038/383531a0.
- Yoshida, ; Takakura, N.; Kataoka, H.; Kunisada, T.; Okamura, H.; Nishikawa, S.I. Stepwise requirement of c-kit tyrosine kinase in mouse ovarian follicle development. Dev. Biol. 1997, 184, 122–137.
- Kezele, R.; Nilsson, E.E.; Skinner, M.K. Insulin but not insulin-like growth factor-1 promotes the primordial to primary follicle transition. Mol. Cell. Endocrinol. 2002, 192, 37–43, doi:10.1016/s0303-7207(02)00114-4.
- Wang, ; Luo, L.-L.; Xu, J.-J.; Xu, M.-Y.; Zhang, X.-M.; Zhou, X.-L.; Liu, W.-J.; Fu, Y.-C. Obesity accelerates ovarian follicle development and follicle loss in rats. Metabolism 2014, 63, 94–103, doi:10.1016/j.metabol.2013.09.001.
- Nteeba, ; Ross, J.; Ii, J.P.; Keating, A. High fat diet induced obesity alters ovarian phosphatidylinositol-3 kinase signaling gene expression. Reprod. Toxicol. 2013, 42, 68–77, doi:10.1016/j.reprotox.2013.07.026.
- Xia, ; Zhang, R.; Guan, H.; Zhang, W. Follicle loss and PTEN/PI3K/mTOR signaling pathway activated in LepR-mutated mice. Gynecol. Endocrinol. 2019, 35, 44–48.
- Loh, ; Fukushima, A.; Zhang, X.; Galic, S.; Briggs, D.; Enriori, P.J.; Simonds, S.; Wiede, F.; Reichenbach, A.; Hauser, C.; et al. Elevated Hypothalamic TCPTP in Obesity Contributes to Cellular Leptin Resistance. Cell Metab. 2011, 14, 684–699, doi:10.1016/j.cmet.2011.09.011.
- Durlinger, L.L.; Kramer, P.; Karels, B.; De Jong, F.H.; Uilenbroek, J.T.J.; Grootegoed, J.A.; Themmen, A.P.N. Control of Primordial Follicle Recruitment by Anti-Müllerian Hormone in the Mouse Ovary1. Endocrinology 1999, 140, 5789–5796, doi:10.1210/endo.140.12.7204.
- Ren, ; Suzuki, H.; Jagarlamudi, K.; Golnoski, K.; McGuire, M.; Lopes, R.; Pachnis, V.; Rajkovic, A. Lhx8 regulates primordial follicle activation and postnatal folliculogenesis. BMC Biol. 2015, 13, 39, doi:10.1186/s12915-015-0151-3.
- Zhang, -P.; Yang, J.-L.; Zhang, J.; Li, L.; Huang, L.; Ji, S.-Y.; Hu, Z.-Y.; Gao, F.; Liu, Y.-X. Notch Signaling Is Involved in Ovarian Follicle Development by Regulating Granulosa Cell Proliferation. Endocrinology 2011, 152, 2437–2447, doi:10.1210/en.2010-1182.
- Yu, ; Yaba, A.; Kasiman, C.; Thomson, T.; Johnson, J. mTOR Controls Ovarian Follicle Growth by Regulating Granulosa Cell Proliferation. PLoS ONE 2011, 6, e21415, doi:10.1371/journal.pone.0021415.
- Hsueh, J.W.; Billig, H.; Tsafriri, A. Ovarian Follicle Atresia: A Hormonally Controlled Apoptotic Process. Endocr. Rev. 1994, 15, 707–724, doi:10.1210/edrv-15-6-707.
- Lin, ; Li, R.; Pan, Z.X.; Zhou, B.; Yu, D.B.; Wang, X.G.; Ma, X.S.; Han, J.; Shen, M.; Liu, H.L. miR-26b Promotes Granulosa Cell Apoptosis by Targeting ATM during Follicular Atresia in Porcine Ovary. PLoS ONE 2012, 7, e38640, doi:10.1371/journal.pone.0038640.
- Li, ; Du, X.; Liu, L.; Liu, H.; Pan, Z. Upregulation of miR-146b promotes porcine ovarian granulosa cell apoptosis by attenuating CYP19A1. Domest. Anim. Endocrinol. 2021, 74, 106509, doi:10.1016/j.domaniend.2020.106509.
- Yuan, ; Wen, J.; Cheng, J.; Shen, W.; Zhou, S.; Yan, W.; Shen, L.; Luo, A.; Wang, S. Age-associated up-regulation of EGR1 promotes granulosa cell apoptosis during follicle atresia in mice through the NF-κB pathway. Cell Cycle 2016, 15, 2895–2905.
- Braw, H.; Tsafriri, A. Effect of PMSG on follicular atresia in the immature rat ovary. Reproduction 1980, 59, 267–272, doi:10.1530/jrf.0.0590267.
- Franks, ; Hardy, K. Androgen Action in the Ovary. Front. Endocrinol. 2018, 9, 452, 10-, doi:10.3389/fendo.2018.00452.
- Fuentes, ; Silveyra, P. Estrogen receptor signaling mechanisms. Adv. Protein Chem. Struct. Biol. 2019, 116, 135–170, doi:10.1016/bs.apcsb.2019.01.001.
- Armstrong, T.; Dorrington, J.H. Estrogen biosynthesis in the ovaries and testes. Adv. Sex Horm. Res. 1977, 3, 217–258.
- Kristensen, G.; Mamsen, L.S.; Jeppesen, J.V.; Bøtkjær, J.A.; Pors, S.E.; Borgbo, T.; Ernst, E.; Macklon, K.T.; Andersen, C.Y. Hallmarks of Human Small Antral Follicle Development: Implications for Regulation of Ovarian Steroidogenesis and Selection of the Dominant Follicle. Front. Endocrinol. 2018, 8, 376, doi:10.3389/fendo.2017.00376.
- Liu, ; Xin, Q.; Wang, X.; Wang, S.; Wang, H.; Zhang, W.; Yang, Y.; Zhang, Y.; Zhang, Z.; Wang, C.; et al. Estrogen receptors in granulosa cells govern meiotic resumption of pre-ovulatory oocytes in mammals. Cell Death Dis. 2017, 8, e2662, doi:10.1038/cddis.2017.82.
- Sar, ; Welsch, F. Differential Expression of Estrogen Receptor-β and Estrogen Receptor-α in the Rat Ovary. Endocrinology 1999, 140, 963–971, doi:10.1210/endo.140.2.6533.
- Dupont, ; Krust, A.; Gansmuller, A.; Dierich, A.; Chambon, P.; Mark, M. Effect of single and compound knockouts of estrogen receptors alpha (ERalpha) and beta (ERbeta) on mouse reproductive phenotypes. Development 2000, 127, 4277–4291.
- Chakravarthi, P.; Ratri, A.; Masumi, S.; Borosha, S.; Ghosh, S.; Christenson, L.K.; Roby, K.F.; Wolfe, M.W.; Rumi, M.K. Granulosa cell genes that regulate ovarian follicle development beyond the antral stage: The role of estrogen receptor β. Mol. Cell. Endocrinology 2021, 528, 111212, doi:10.1016/j.mce.2021.111212.
- Kovács, ; Szabó-Meleg, E.; Ábrahám, I.M. Estradiol-Induced Epigenetically Mediated Mechanisms and Regulation of Gene Expression. Int. J. Mol. Sci. 2020, 21, 3177.
- Simon, M.; Goodenough, D.A.; Li, E.; Paul, D.L. Female infertility in mice lacking connexin 37. Nat. Cell Biol. 1997, 385, 525–529, doi:10.1038/385525a0.
- Granot, ; Dekel, N. The ovarian gap junction protein connexin43: Regulation by gonadotropins. Trends Endocrinol. Metab. 2002, 13, 310–313, doi:10.1016/s1043-2760(02)00623-9.
- Wiesen, F.; Midgley, A.R. Changes in expression of connexin 43 gap junction messenger ribonucleic acid and protein during ovarian follicular growth. Endocrinology 1993, 133, 741–746, doi:10.1210/endo.133.2.8393773.
- Albertini, F.; Combelles, C.M.; Benecchi, E.; Carabatsos, M.J. Cellular basis for paracrine regulation of ovarian follicle development. Reproduction 2001, 121, 647–653.
- Combelles, M.; Carabatsos, M.J.; Kumar, T.R.; Matzuk, M.M.; Albertini, D.F. Hormonal control of somatic cell oocyte interactions during ovarian follicle development. Mol. Reprod. Dev. 2004, 69, 347–355, doi:10.1002/mrd.20128.
- Makita, ; Miyano, T. Steroid hormones promote bovine oocyte growth and connection with granulosa cells. Theriogenology 2014, 82, 605–612, doi:10.1016/j.theriogenology.2014.05.020.
- Zachow, J.; Magoffin, D.A. Direct Intraovarian Effects of Leptin: Impairment of the Synergistic Action of Insulin-Like Growth Factor-I on Follicle-Stimulating Hormone-Dependent Estradiol-17β Production by Rat Ovarian Granulosa Cells. Endocrinology 1997, 138, 847–850, doi:10.1210/endo.138.2.5035.
- Guo, ; Chen, S.; Xing, F. Effects of leptin on estradiol and progesterone production by human luteinized granulosa cells in vitro. Zhonghua fu chan ke za zhi 2001, 36, 95–97.
- Gregoraszczuk, Łucja; Wójtowicz, A.K.; Ptak, A.; Nowak, K. In vitro effect of leptin on steroids’ secretion by FSH- and LH-treated porcine small, medium and large preovulatory follicles. Reprod. Biol. 2003, 3, 227–239.
- Agarwal, K.; Vogel, K.; Weitsman, S.R.; Magoffin, D.A. Leptin Antagonizes the Insulin-Like Growth Factor-I Aug-mentation of Steroidogenesis in Granulosa and Theca Cells of the Human Ovary 1. J. Clin. Endocrinol. Metab. 1999, 84, 1072–1076.
- Ma, ; Hayes, E.; Prizant, H.; Srivastava, R.K.; Hammes, S.R.; Sen, A. Leptin-induced CART (cocaine- and ampheta-mine-regulated transcript) is a novel intraovarian mediator of obesity-related infertility in females. Endocrinology 2016, 157, 1248–1257, Mar. 2016.
- Mirshamsi, ; Laidlaw, H.A.; Ning, K.; Anderson, E.; Burgess, L.A.; Gray, A.; Sutherland, C.; Ashford, M.L.J. Leptin and insulin stimulation of signalling pathways in arcuate nucleus neurones: PI3K dependent actin reorganization and KATP channel activation. Bmc Neurosci. 2004, 5, 54, doi:10.1186/1471-2202-5-54.
- Li, ; Liang, J.; Wu, W.K.K.; Yu, X.; Yu, J.; Weng, X.; Shen, J. Leptin Activates RhoA/ROCK Pathway to Induce Cytoskeleton Remodeling in Nucleus Pulposus Cells. Int. J. Mol. Sci. 2014, 15, 1176–1188, doi:10.3390/ijms15011176.
- Antczak; ; Blerkom, V.J. Oocyte influences on early development: The regulatory proteins leptin and STAT3 are polarized in mouse and human oocytes and differentially distributed within the cells of the preimplantation stage embryo. Mol. Hum. Reprod. 1997, 3, 12.
- Deng, -H.; Liao, J.; Zhang, J.-Y.; Liang, C.; Song, C.-H.; Han, M.; Wang, L.-H.; Xue, H.; Zhang, K.; Zabeau, L.; et al. Inhibition of the Connexin 43 Elevation May be Involved in the Neuroprotective Activity of Leptin Against Brain Ischemic Injury. Cell. Mol. Neurobiol. 2014, 34, 871–879, doi:10.1007/s10571-014-0066-5.
- Panza, ; Russo, U.; Giordano, F.; Leggio, A.; Barone, I.; Bonofiglio, D.; Gelsomino, L.; Malivindi, R.; Conforti, F.L.; Naimo, G.D.; et al. Leptin and Notch Signaling Cooperate in Sustaining Glioblastoma Multiforme Progression. Biomolecules 2020, 10, 886, doi:10.3390/biom10060886.
- Quinkler, ; Sinha, B.; Tomlinson, J.W.; Bujalska, I.J.; Stewart, P.M.; Arlt, W. Androgen generation in adipose tissue in women with simple obesity–a site-specific role for 17β-hydroxysteroid dehydrogenase type 5. J. Endocrinol. 2004, 183, 331–342, doi:10.1677/joe.1.05762.
- Wu, ; Divall, S.; Nwaopara, A.; Radovick, S.; Wondisford, F.; Ko, C.; Wolfe, A. Obesity-Induced Infertility and Hyperandrogenism Are Corrected by Deletion of the Insulin Receptor in the Ovarian Theca Cell. Diabetes 2013, 63, 1270–1282, doi:10.2337/db13-1514.
- Souter, ; Baltagi, L.M.; Kuleta, D.; Meeker, J.D.; Petrozza, J.C. Women, weight, and fertility: The effect of body mass index on the outcome of superovulation/intrauterine insemination cycles. Fertil. Steril. 2011, 95, 1042–1047, doi:10.1016/j.fertnstert.2010.11.062.
- Sagae, C.; Menezes, E.F.; Bonfleur, M.L.; Vanzela, E.C.; Zacharias, P.; Lubaczeuski, C.; Franci, C.R.; Sanvitto, G.L. Early onset of obesity induces reproductive deficits in female rats. Physiol. Behav. 2012, 105, 1104–1111, doi:10.1016/j.physbeh.2011.12.002.
- Arnold, F.; Melamed, M.; Vorojeikina, D.P.; Notides, A.C.; Sasson, S. Estradiol-Binding Mechanism and Binding Capacity of the Human Estrogen Receptor Is Regulated by Tyrosine Phosphorylation. Mol. Endocrinol. 1997, 11, 48–53.
- Barone, ; Giordano, C.; Malivindi, R.; Lanzino, M.; Rizza, P.; Casaburi, I.; Bonofiglio, D.; Catalano, S.; Andò, S. Estrogens and PTP1B Function in a Novel Pathway to Regulate Aromatase Enzymatic Activity in Breast Cancer Cells. Endocrinol. 2012, 153, 5157–5166, doi:10.1210/en.2012-1561.
- White, L.; Whittington, A.; Barnes, M.J.; Wang, Z.; Bray, G.A.; Morrison, C.D. HF diets increase hypothalamic PTP1B and induce leptin resistance through both leptin-dependent and -independent mechanisms. Am. J. Physiol. Metab. 2009, 296, E291–E299, doi:10.1152/ajpendo.90513.2008.
- Fan, Y.; Liu, Z.; Shimada, M.; Sterneck, E.; Johnson, P.F.; Hedrick, S.M.; Richards, J.S. MAPK3/1 (ERK1/2) in ovarian granulosa cells are essential for female fertility. Science 2009, 324, 938–941.
- Ma, -Y.; Li, M.; Luo, Y.-B.; Song, S.; Tian, D.; Yang, J.; Zhang, B.; Hou, Y.; Schatten, H.; Liu, Z.; et al. Maternal factors required for oocyte developmental competence in mice: Transcriptome analysis of non-surrounded nucleolus (NSN) and surrounded nucleolus (SN) oocytes. Cell Cycle 2013, 12, 1928–1938, doi:10.4161/cc.24991.
- Hinckley, ; Vaccari, S.; Horner, K.; Chen, R.; Conti, M. The G-protein-coupled receptors GPR3 and GPR12 are involved in cAMP signaling and maintenance of meiotic arrest in rodent oocytes. Dev. Biol. 2005, 287, 249–261, doi:10.1016/j.ydbio.2005.08.019.
- Oh, S.; Han, S.J.; Conti, M. Wee1B, Myt1, and Cdc25 function in distinct compartments of the mouse oocyte to control meiotic resumption. J. Cell Biol. 2010, 188, 199–207, doi:10.1083/jcb.200907161.
- Pan, ; Li, J. The art of oocyte meiotic arrest regulation 11 Medical and Health Sciences 1114 Paediatrics and Reproductive Medicine. Reprod. Biol. Endocrinol. 2019, 17, 1–12.
- Vaccari, ; Weeks, J.L.; Hsieh, M.; Menniti, F.S.; Conti, M. Cyclic GMP signaling is involved in the luteinizing hor-mone-dependent meiotic maturation of mouse oocytes. Biol. Reprod. 2009, 81, 595–604.
- Nogueira, ; Ron-El, R.; Friedler, S.; Schachter, M.; Raziel, A.; Cortvrindt, R.; Smitz, J. Meiotic Arrest In Vitro by Phosphodiesterase 3-Inhibitor Enhances Maturation Capacity of Human Oo-cytes and Allows Subsequent Embryonic Development1. Biol. Reprod. 2006, 74, 177–184.
- Yang, ; Zhang, Y.; Xu, X.; Li, J.; Yuan, F.; Bo, S.; Qiao, J.; Xia, G.; Su, Y.; Zhang, M. Transforming growth factor-β is involved in maintaining oocyte meiotic arrest by promoting natriuretic peptide type C expression in mouse granulosa cells. Cell Death Dis. 2019, 10, 1–13, doi:10.1038/s41419-019-1797-5.
- Gill, ; Jamnongjit, M.; Hammes, S.R. Androgens Promote Maturation and Signaling in Mouse Oocytes Independent of Transcription: A Release of Inhibition Model for Mammalian Oocyte Meiosis. Mol. Endocrinol. 2004, 18, 97–104, doi:10.1210/me.2003-0326.
- Holubcová, ; Blayney, M.; Elder, K.; Schuh, M. Error-prone chromosome-mediated spindle assembly favors chromosome segregation defects in human oocytes. Science 2015, 348, 1143–1147, doi:10.1126/science.aaa9529.
- Watson, J. Oocyte cytoplasmic maturation: A key mediator of oocyte and embryo developmental competence1. J. Anim. Sci. 2007, 85, E1–E3, doi:10.2527/jas.2006-432.
- Schisa, A. New Insights into the Regulation of RNP Granule Assembly in Oocytes. Int. Rev. Cell Mol. Biol. 2012, 295, 233–289, doi:10.1016/b978-0-12-394306-4.00013-7.
- Esposito, ; Vitale, A.M.; Leijten, F.P.J.; Strik, A.M.; Koonen-Reemst, A.M.C.B.; Yurttas, P.; Robben, T.J.A.A.; Coonrod, S.; Gossen, J.A. Peptidylarginine deiminase (PAD) 6 is essential for oocyte cytoskeletal sheet formation and female fer-tility. Mol. Cell. Endocrinol. 2007, 273, 25–31.
- Kim, ; Kan, R.; Anguish, L.; Nelson, L.M.; Coonrod, S.A. Potential Role for MATER in Cytoplasmic Lattice Formation in Murine Oocytes. PLoS ONE 2010, 5, e12587, doi:10.1371/journal.pone.0012587.
- Steeves, E.; Gardner, D.K.; Zuelke, K.A.; Squires, T.S.; Fry, R.C. In vitro development and nutrient uptake by embryos derived from oocytes of pre-pubertal and adult cows. Mol. Reprod. Dev. 1999, 54, 49–56.
- Cui, -S.; Li, X.-Y.; Yin, X.-J.; Kong, I.K.; Kang, J.-J.; Kim, N.-H. Maternal Gene Transcription in Mouse Oocytes: Genes Implicated in Oocyte Maturation and Fertilization. J. Reprod. Dev. 2007, 53, 405–418, doi:10.1262/jrd.18113.
- Katz-Jaffe, ; McCallie, B.; Preis, K.; Filipovits, J.; Gardner, D. Transcriptome analysis of in vivo and in vitro matured bovine MII oocytes. Theriogenology 2009, 71, 939–946, doi:10.1016/j.theriogenology.2008.10.024.
- Downs, M.; Hudson, E.D. Energy substrates and the completion of spontaneous meiotic maturation. Zygote 2000, 8, 339–351, doi:10.1017/s0967199400001131.
- Sanfins, ; Rodrigues, P.; Albertini, D.F. GDF-9 and BMP-15 direct the follicle symphony. J. Assist. Reprod. Genet. 2018, 35, 1741–1750, doi:10.1007/s10815-018-1268-4.
- Wilding, ; Coppola, G.; Dale, B.; Di Matteo, L. Mitochondria and human preimplantation embryo development. Reproduction 2009, 137, 619–624, doi:10.1530/rep-08-0444.
- Dunning, R.; Anastasi, M.R.; Zhang, V.J.; Russell, D.L.; Robker, R.L. Regulation of Fatty Acid Oxidation in Mouse Cumulus-Oocyte Complexes during Maturation and Modulation by PPAR Agonists. PLoS ONE 2014, 9, e87327, doi:10.1371/journal.pone.0087327.
- Reidy, P.; Weber, J.-M. Leptin: An essential regulator of lipid metabolism. Comp. Biochem. Physiol. Part. A Mol. Integr. Physiol. 2000, 125, 285–298, doi:10.1016/s1095-6433(00)00159-8.
- Paula-Lopes, F.; Boelhauve, M.; Habermann, F.A.; Sinowatz, F.; Wolf, E. Leptin Promotes Meiotic Progression and Developmental Capacity of Bovine Oocytes Via Cumulus Cell-Independent and -Dependent Mechanisms1. Biol. Reprod. 2007, 76, 532–541, doi:10.1095/biolreprod.106.054551.
- Craig, ; Zhu, H.; Dyce, P.W.; Petrik, J.; Li, J. Leptin enhances oocyte nuclear and cytoplasmic maturation via the mito-gen-activated protein kinase pathway. Endocrinology 2004, 145, 5355–5363.
- Ye, ; Kawamura, K.; Sasaki, M.; Kawamura, N.; Groenen, P.; Gelpke, M.D.S.; Kumagai, J.; Fukuda, J.; Tanaka, T. Leptin and ObRa/MEK signalling in mouse oocyte maturation and preimplantation embryo development. Reprod. Biomed. Online 2009, 19, 181–190, doi:10.1016/s1472-6483(10)60070-3.
- Ahrén, ; Havel, P.J. Leptin inhibits insulin secretion induced by cellular cAMP in a pancreatic B cell line (INS-1 cells). Am. J. Physiol. Content 1999, 277, R959–R966, doi:10.1152/ajpregu.1999.277.4.r959.
- Zhao, Z.; Bornfeldt, K.E.; Beavo, J.A. Leptin inhibits insulin secretion by activation of phosphodiesterase 3B. J. Clin. Investig. 1998, 102, 869–873, doi:10.1172/jci3920.
- Zhao, ; Hou, M.; Xia, M.; Wang, Q.; Zhu, H.; Xiao, Y.; Tang, Z.; Ma, J.; Ling, W. Globular adiponectin decreases leptin-induced tumor necrosis factor-α expression by murine macrophages: Involvement of cAMP-PKA and MAPK pathways. Cell. Immunol. 2005, 238, 19–30.
- Morton, J.; Schwartz, M.W. Leptin and the Central Nervous System Control of Glucose Metabolism. Physiol. Rev. 2011, 91, 389–411, doi:10.1152/physrev.00007.2010.
- Silva, ; Paczkowski, M.; Krisher, R.L. The effect of leptin on maturing porcine oocytes is dependent on glucose con-centration. Mol. Reprod. Dev. 2012, 79, 296–307.
- Purcell, H.; Moley, K.H. The impact of obesity on egg quality. J. Assist. Reprod. Genet. 2011, 28, 517–524, doi:10.1007/s10815-011-9592-y.
- Purcell, H.; Chi, M.M.; Moley, K.H. Insulin-Stimulated Glucose Uptake Occurs in Specialized Cells within the Cumulus Oocyte Complex. Endocrinology 2012, 153, 2444–2454, doi:10.1210/en.2011-1974.
- Sutton-McDowall, L.; Gilchrist, R.B.; Thompson, J.G. The pivotal role of glucose metabolism in determining oocyte developmental competence. Reproduction 2010, 139, 685–695, doi:10.1530/rep-09-0345.
- Robker, L. Evidence that obesity alters the quality of oocytes and embryos. Pathophysiology 2008, 15, 115–121, doi:10.1016/j.pathophys.2008.04.004.
- Huang, ; Hao, C.; Shen, X.; Liu, X.; Shan, Y.; Zhang, Y.; Chen, L. Differences in the transcriptional profiles of human cumulus cells isolated from MI and MII oocytes of patients with polycystic ovary syndrome. Reproduction 2013, 145, 597–608, doi:10.1530/rep-13-0005.
This entry is adapted from the peer-reviewed paper 10.3390/ijms22084270
