The emergence of the coronavirus disease 2019 (COVID-19) pandemic has rapidly transformed the pre-existing worldwide sexual and reproductive health environment. The provision and supply of contraceptives, and a wide variety of sexual health, new-born, and maternal health services have been seriously affected. Thus, this scoping review mapped the available evidence on the impacts of the COVID-19 outbreak on sexual and reproductive health.
- COVID-19
- family planning
- maternal and child health services
- sexual health
- sexual and reproductive health
1. Introduction
The emergence of the coronavirus disease 2019 (COVID-19) pandemic has transformed the pre-existing worldwide sexual and reproductive health environment rapidly [1,2]. The provision and supply of contraceptives and a wide variety of sexual health, new-born, and maternal health services have been seriously affected or disrupted [3,4,5].
More than two decades ago, the United Nations at the International Conference on Population and Development (ICPD), held in Cairo, recognized the role of an adequate response to an individual’s reproductive health needs as a panacea to universal economic and social development [6]. The gathering further endorsed the equal distribution of family planning and other related sexual and reproductive health services via the primary healthcare system to encourage comprehensive reproductive health care utilization [6]. Therefore, reproductive health implies an individual’s ability to have a satisfying and safe sex life and have the capacity and freedom to reproduce at their desire [6], hence the need to provide adequate and friendly access to safe, effective, affordable, and acceptable methods of family planning and health care services of their choice that will increase maternal and child health safety. This concept also includes sexual health, which is considered the enhancement of life and personal relations relating to reproduction and sexually transmitted infections (STIs) [6,7].
Prior to the emergence of COVID-19, adverse sexual and reproductive health outcomes have been a major issue globally, with an estimated 210 million women being exposed to pregnancy complications, and approximately half a million of these women dying between pregnancy and the post-partum period [8]. In addition, about 68 000 women die every year from complications of unsafe abortions [9]. In the same vein, 3.3 million infants were stillborn, whilst 3 million babies die in the first week of their life yearly [8]. This is also coupled with more than 340 million new sexually transmitted bacterial and protozoal infections acquired every year [10].
Interestingly, uninterrupted access to sexual and reproductive services has been identified as a remedy to curb these adverse sexual and reproductive health globally and across all socio-demographic characteristics [11,12,13,14]. However, the sudden emergence of the COVID-19 outbreak and the virus’s declaration as a global health concern in the first quarter of the year 2020 led many governments worldwide to enforce country-national lockdowns in order to limit the propagation of the virus [15]. These measures have been documented to have altered sexual and reproductive health (SRH) services around the world [16].
Specifically, SRH services such as family planning supplies [17], sexual health [18], and maternal and child health services [17,19] have been disrupted. To ensure adherence to guidelines prescribed by the World Health Organization (WHO) [20], authors at the Guttmacher Institute and others have opined that the sudden halt in supply of SRH services would lead to an unexpected rise in adverse SRH [17,21,22].
2. Screening Results
After the database search, this scoping review found two hundred and eighty-nine (289) eligible studies from a total of 1575 articles after title screening and removing duplicates. A total of 47 articles were also excluded following the abstract and 225 after full article screening. Hence, 17 articles were included for analysis. Results of the article screening are presented in Figure 1.
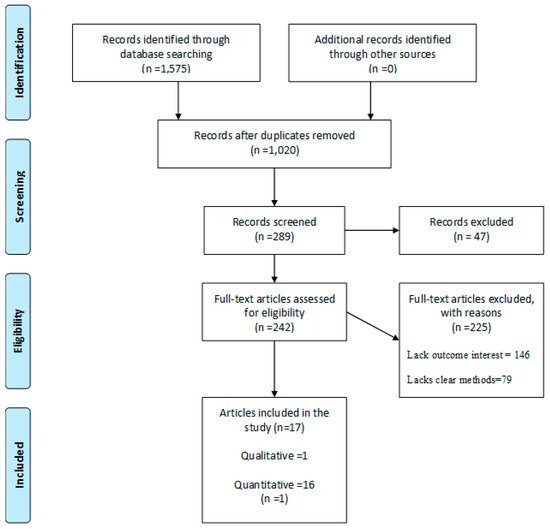
Figure 1. PRISMA flow-chart of the study selection process. (Source: Adapted from Moher et al. [30]).
The preferred report items for systematic and meta-analysis (PRISMA) flow chart for the screening and selection of studies in this review is shown in Figure 1.
3. Characteristics of the Included Studies
Table 1 shows the characteristics of the included studies. These included studies were conducted in various high income countries (HICs) and low-middle income countries (LMICs) (Figure 2): 23% of the studies were done in the United Kingdom [31,32,33,34], 6% in Brazil [35], 17% in the United States [36,37,38], 6% in Wales [39], 12% in Italy [40,41], 6% in Israel [42], 6% in the United States, Canada, United Kingdom, Australia, and other countries [43], 6% in Turkey [44], 6% in Belgium [45], 6% in Poland [46], and 6% in HICs and LMICs [47].
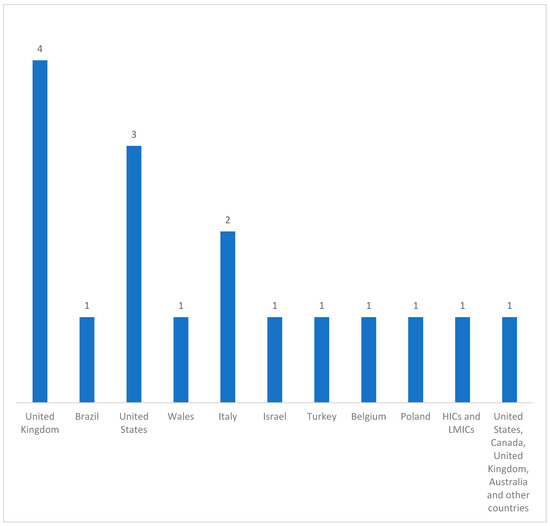
Figure 2. Distribution of the countries represented in the included studies (n = 17).
4. Quality of Evidence from the Included Studies
All the included studies received a high quality score ranging from 80% to 100% during the methodological quality assessment. Overall, the included studies were deemed to have a low chance of bias.
Table 2 below shows that the most common sexual and reproductive health service impacted by the outbreak of COVID-19 was sexual behavior because changes in pattern of sexual behavior were reported in almost all the countries included in the study except in Belgium, with 11 studies reporting unusual sexual behavior during the COVID-19 pandemic [32,35,36,37,38,39,41,42,43,44,46]. Contraceptive use or family planning service disruption was reported in the United States [36], Italy [40], and Turkey [44], with 3 studies reporting limited access to contraceptive of choice. Maternal and child health services disruption was reported in the United Kingdom thrice [31,33,34], Turkey once [44], Belgium once [45], and once in a study conducted in more than one country [47].
Table 2. Showing common findings in all countries included in the study.
| Countries Included in the Study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 and SHR Services | United Kingdom | Brazil | United States | Wales | Italy | Israel | Turkey | Belgium | Poland | Multiple Countries |
| COVID-19 and family planning services | X * | X * | X * | |||||||
| COVID-19 and maternal and child services | XX *** | XX * | XX * | XX * | ||||||
| COVID-19 and sexual behavior | XXX * | XXX * | XXX *** | XXX * | XXX * | XXX* | XXX * | XXX * | XXX * | |
Source: Authors, X represents family planning services were disrupted by COVID-19 outbreak, XX represents maternal and health care services were disrupted by COVID-19 outbreak, XXX represents COVID-19 impacted sexual behavior, * represents number of times study reported any of the SRH by countries.
5. Themes from Included Studies
5.1. COVID-19 and Family Planning Services
Four of the seventeen included studies reported on the impact of COVID-19 and family planning services [36,37,40,44]. A study conducted in Turkey showed a significant decrease in contraception use during the pandemic compared with the time prior to the pandemic [44].
A cross-sectional study carried out in Italy reported that 50.5% of single or non-cohabiting women had discontinued their short-acting reversible contraception (SARC) method while social distancing due to the COVID-19 pandemic, for non-method-related reasons [40]. However, 46.5% of the non-cohabiting or single women did not adhere to the social distancing guidelines and continued with their sexual activity resulting in 14.9% of the women having an unplanned pregnancy and requesting termination [40]. A study conducted on the impact of COVID-19 on men who have sex with men (MSM) in the United States demonstrated that 9.4% of the participants had less access to condoms, while 5.4% reported less use of a condom [36].
On the contrary, Sanchez et al. [36] reported that 89.4% and 92.9% of the participants had no change in access to or condom use, consecutively, and condom access and usage remained unchanged due to COVID-19 [36] as shown in Table 3.
Table 3. Summary characteristics of the included studies.
| Author and Year | Study Setting (Country) | Study Design | Population (n) (Sample Size and Target Pop) |
COVID-19 and Family Planning Services | COVID-19 and Maternal and Child Services | COVID-19 and Sexual Behavior |
|---|---|---|---|---|---|---|
| Babu Karavadra et al. and 2020 [31] | United Kingdom | Cross-sectional (Web survey) | Women who were pregnant or delivered during COVID-19, n = 1451 |
|
||
| Thiago S. Torres et al. and 2020 [35] | Brazil | Cross-sectional (Web-survey) |
n = 3486 among cismen |
|
||
| Travis H. Sanchez et al. and 2020 [36] | United States | Cross-sectional (Web survey) | Men who have sex with men n = 1051 |
|
|
|
| David Gillespie et al. and 2020 [39] | Wales | Longitudinal survey (Web survey) |
Participants were individuals accessing PrEP n = 56 |
|
||
| Salvatore Caruso and 2020 [40] | Italy | Cross-sectional (Web survey) | Among women known to be using hormonal contraceptives, n = 169 |
|
||
| Rob Stephenson et al. and 2020 [37] | United States | Cross-sectional (Web survey) | Among gay, bisexual, and other men who have sex with men, n = 518 |
|
||
| Guy Shilo and Zohar Mor and 2020 [42] | Israel | Cross-sectional (Web survey) | Among men who have sex with men, n = 2562 |
|
||
| Michele Carlo Schiavi and 2020 [41] | Italy | Cross-sectional | Women of reproductive age, n = 89 |
|
||
| Louis Jacob et al. and 2020 [32] | United Kingdom | Cross-sectional (Web survey) | n = 868 |
|
||
| Tyrel J. Starks et al. and 2020 [38] | United States | Cohort-control design | Among sexual minority men, n = 455 |
|
||
| Justin J. Lehmiller et al. and 2020 [43] | United States 73.4% Canada 6.0% United Kingdom 5.7% Australia 2.4% Other countries, 12.5% |
Cross-sectional (Web survey) | Among participants 18 years of age or older, n = 1559 |
|
||
| Bahar Yuksel, Faruk Ozgor and 2020 [44] | Turkey | Cross-sectional (Telephone) |
Among married patients who were older than 18 years and sexually active, n = 58 |
|
|
|
| Helen I McDonald et al. and 2020 [33] | United Kingdom | Cross-sectional | Vaccination among children n = 67,116 |
|
||
| Michael Ceulemans et al. and 2020 [45] | Belgium | Cross-sectional (Web survey) | 2647 pregnant and 3823 breastfeeding women, n = 6470 |
|
||
| Anna Fuchs et al. and 2020 [46] | Poland | Cross-sectional | 764 sexually active female patients and above 18 years |
|
||
| James John Ashton et al. 2020 [34] | United Kingdom | Cross-sectional | 20 tertiaries pediatric IBD centers |
|
||
| Anja Saso, Helen Skirrow and Beate Kampmann and 2020 [47] | LMICs and HICs | Cross-sectional (Web survey) | n = 48 |
|
This entry is adapted from the peer-reviewed paper 10.3390/healthcare9040436
