Lung ultrasound has become increasingly used in both adult and pediatric populations, allowing the rapid evaluation of many lung and pleura diseases.
- lung ultrasound
- infants
- children
1. Introduction
The management of pediatric lung diseases has always been challenging for clinicians because of the variable clinical manifestations and often overlapping symptoms and signs. Traditionally, chest X-ray (CXR) has played a crucial role in the diagnosis of respiratory diseases. However, the potentially harmful effects of radiation exposure due to CXR reduce its applications, especially in children [1].
In recent years, a new imaging application of sonography has spread in emergency departments and clinical practice: lung ultrasound (LUS) [2]. It is quick, portable, repeatable, lacks ionizing radiation and, therefore, finds application in many different settings, both inpatient and outpatient, in both acute and chronic conditions [3]. In particular, growing evidence highlights the effectiveness of this method as a diagnostic tool in different pediatric diseases [4,5]. Infants and children are considered ideal candidates for this type of exam due to their thinner chest and smaller lung volumes. These features help to make any lesions better visible because, in smaller lungs, it is more likely that such lesions reach the pleura and make the linear probe able to complete the exam [6].
2. Lung Ultrasound Findings in Healthy Subjects
3. Lung and Chest Wall Ultrasound Applications in Children
The main indications for lung and chest wall ultrasound in the pediatric population include:
-
Diagnosis and follow-up of neonatal lung diseases;
-
Confirm antenatal diagnosis of lung malformations;
-
Diagnosis and follow-up of pediatric lung infectious diseases (namely bronchiolitis and pneumonia) and lung complications (such as pneumothorax, pleural effusion and lung abscess);
-
Diagnosis and follow-up of pulmonary edema;
-
Diagnosis of thoracic trauma and early detection of signs of child abuse;
-
Follow-up in children undergoing cardiac surgery;
-
Diaphragm ultrasound.
4. Neonatal Lung Diseases
Many lung diseases, such as respiratory distress syndrome, transient tachypnea, pneumonia, atelectasis and pneumothorax, can cause respiratory distress in newborns, especially among premature infants. The differential diagnosis of these diseases is often difficult, but LUS can help to discriminate these diseases [19,20].
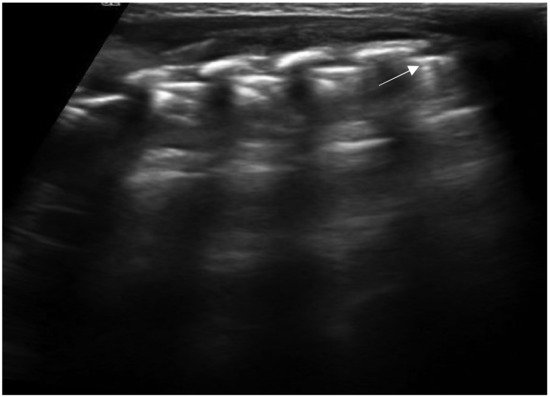
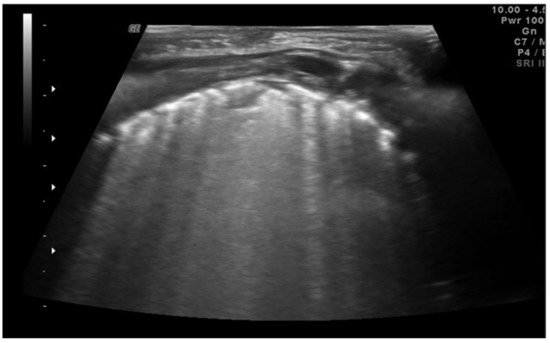
Neonatal respiratory distress syndrome (NRDS) is characterized by a functional and structural immaturity of the lung resulting in respiratory distress that appears at birth. The ultrasound findings of NRDS are represented by coalescent B-lines, diffuse and symmetrically distributed in both lungs. These lines are due to the presence of fluid in the interstitial or alveolar compartment, and generally, their number correlates with the severity of the disease, up to “white lung” in the most severe cases. The pleural line appears irregular, poorly defined and thickened. In addition, small areas of hypoechogenic subpleural consolidation can often be observed, especially in the posterior lung fields (Figure 4) [21].
The 2019 European consensus guidelines on the management of respiratory distress syndrome assert that lung ultrasound could be a useful tool for clinical decision making, and it seems able to differentiate NRDS from other common respiratory disorders of the newborn, reducing exposure to ionizing radiation [22]. In addition, some recent evidence has underlined how ultrasound performed in the first 12 h of life can be useful in identifying patients most likely to require surfactant therapy or mechanical ventilation, even before the oxygenation criteria [23].
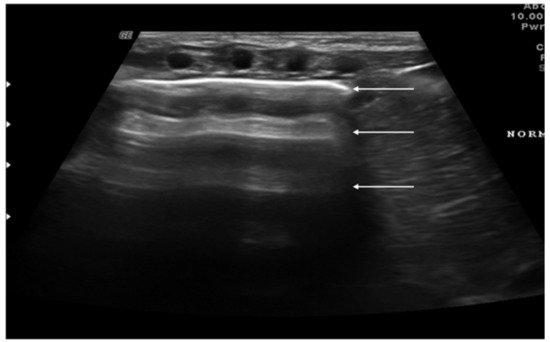
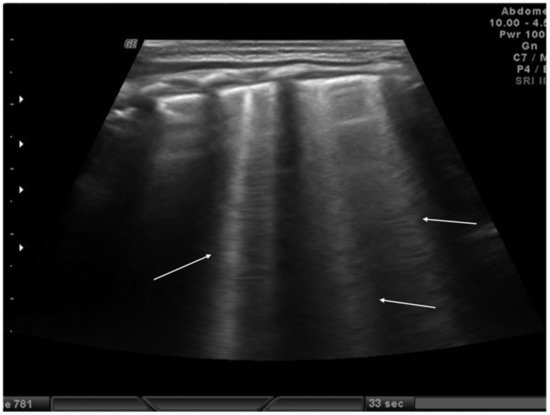
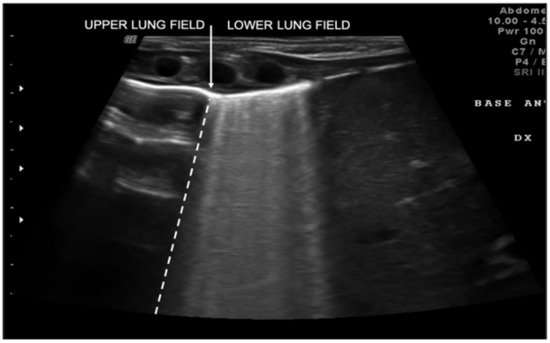
Transient tachypnea of the newborn (TTN), also known as “wet lung,” is caused by a failure in the reabsorption of fluid from the fetal lung. It is typical of term or post-term infants in the case of rapid delivery or cesarean section [24]. Infants with TTN present compact B-lines in the lower lung fields and fewer and less compact B-lines in the upper fields in one or both lungs. These signs, also known as double-lung points, appear because of the greater involvement of the lower lung fields in the disease and are characterized by a sharp ultrasound demarcation line between the upper and lower lung fields of both lungs (Figure 5) [17]. The pleural line is regular, with normal echogenicity and movement with respiratory acts. In contrast to NRDS, no subpleural consolidations are observed. Due to these typical ultrasonographic findings, much evidence has shown how pulmonary ultrasonography can be useful in the early diagnosis of TTN and differentiate TTN from NRDS already by the first hours of life [25].
Meconium aspiration syndrome (MAS) refers to a multitude of respiratory symptoms caused by meconium aspiration during delivery. It is more frequent in post-term newborns. The ultrasound findings of MAS are as follows: B-pattern appearance, with coalescent or noncoalescent B-lines, several subpleural consolidations asymmetrically spread on both lungs with few spared areas and in severe cases of MAS a white lung pattern [26].
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics11040652
