This review presents the common commercially available skin substitutes and their clinical use. Moreover, the choice of an appropriate hydrogel type to prepare cell-laden skin substitutes is discussed. Additionally, we present recent advances in the field of bioengineered human skin substitutes using three-dimensional (3D) bioprinting techniques. Finally, we discuss different skin substitute developments to meet different criteria for optimal wound healing.
- bioengineered skin
- skin substitute
- hydrogel scaffold
- 3D bioprinting
1. Introduction
Skin is the largest organ and protects the human body against the external environment [1]. Loss of the integrity of the skin barrier, as a result of injury or malformation may lead to major complications or even death. Therefore, wound healing represents a crucial ability of the human skin to repair any skin defect and to keep proper skin homeostasis.
Large and deep skin wounds caused by extensive burns or tissue trauma still pose a significant challenge for the surgeon. If those wounds do not heal in time after skin damage, they might cause infection or life-threatening complications. [2]. Therefore, it is pivotal to develop tissue-regenerating biomaterials with high biological activity. Accordingly, the ideal skin substitute should have good biocompatibility, antibacterial activity, proper hydrophilicity, and biodegradability [3].
2. Skin Injuries and Common Treatment Techniques
The human skin consists of three major components including a superficial epidermis, a dermis, and a hypodermis [4]. The epidermis is composed of several layers. The outermost layer contains dead cells, which shed periodically and are continually replaced by cells derived from the basal layer [5]. The dermis connects the epidermis to the hypodermis layer, and due to the high content of collagen and elastin fibers, the dermis gives skin its strength and elasticity [6]. The hypodermis is the deepest layer of the skin located underneath the dermis. The hypodermis consists mainly of adipocytes, which accumulate fat. It also plays a role in thermoregulation, protection and provides insulation and cushioning for the integument [7].
The integrity of skin can be disrupted by various factors, leading to different types of wounds including acute and chronic wounds. Furthermore, wounds can be further split into mechanical injuries such as those caused by external factors (abrasions and tears) and skin injuries raised from radiation, electricity, corrosive chemicals, and thermal sources causing severe burns [8].
Skin wound healing is a complex, multi-stage process, which can be divided into homeostasis, inflammation, proliferation, and remodeling (maturation) phases [1]. To facilitate skin repair, the fine-tuned activation of numerous cell types such as keratinocytes, fibroblasts, endothelial cells, and immune cells is required. Furthermore, these cells secrete a variety of proinflammatory mediators, growth factors, and cytokines that promote skin repair [2]. Among immune cells, macrophages appear to be pivotal in this process [9][10][11]. They appear early during wound healing as so-called M1-polarized macrophages and differentiate to M2-phenotype at later stages of skin wound healing [12][13]. The phenotype change from M1 to M2 seems to be crucial to support the appropriate wound healing process. In contrast, prolonged M1-macrophage persistence in the wound might results in enhanced inflammation, leading to excessive scarring and delayed wound healing [11][14].
The human body is capable of healing minor superficial skin injuries by epithelialization without any particular treatment. However, large and deep skin defects require skin substitution to heal properly [15].
In particular, non-healing chronic wounds impose an immense financial burden on the healthcare systems and societies [2]. The primary reason for the impaired healing of chronic wounds is repeated tissue insults or accompanying diseases such as diabetes [16]. Moreover, in hard-to-heal chronic wounds, impaired vascularization is the main cause of delayed healing that might lead to tissue necrosis and, eventually, amputation [13][17]. In fact, capillaries are responsible for the metabolic exchange between blood and tissues [18][19]. If the angiogenesis process is disturbed, the wound cannot heal properly and the healing period is prolonged [18][19]. Thus, rapid neovascularization within only days after skin substitute implantation is of vital importance for the efficient healing of those wounds [12][13][18][20][21][22][23].
3. Cell-Based Skin Substitutes
Chronic wounds influence a patient’s life quality, leading to impaired mobility, sleep disturbance, psychological stress, and chronic pain [24]. A central problem causing poor skin wound healing in chronic wounds is impaired vascularization and cell activity [25]. Therefore, progress in the tissue engineering field aims for the development of cell-based wound substitutes or wound coverages that improve wound healing by promoting cell migration, differentiation, and vascularization [24]. The majority of cell-based skin substitutes are comprised of a scaffold upon which cells are seeded/cultured. Scaffolds are designed to integrate into the host tissue and provide an appropriate environment for cell growth, infiltration, and differentiation [26]. Thus, those scaffolds need to exhibit some specific characteristics such as appropriate porosity distribution to deliver oxygen and nutrients to cells and drive out carbon dioxide and waste products to allow cell proliferation, and expansion and biocompatibility. Moreover, the scaffold should mimic the mechanical properties of native human skin, which has an elastic modulus in the range of 88–300 kPa [27]. Accordingly, different skin templates have been engineered worldwide and there are various commercial cell-based templates for wound healing applications. Figure 1 demonstrates a classification and summary of commercial skin substitutes with examples discussed in this review.
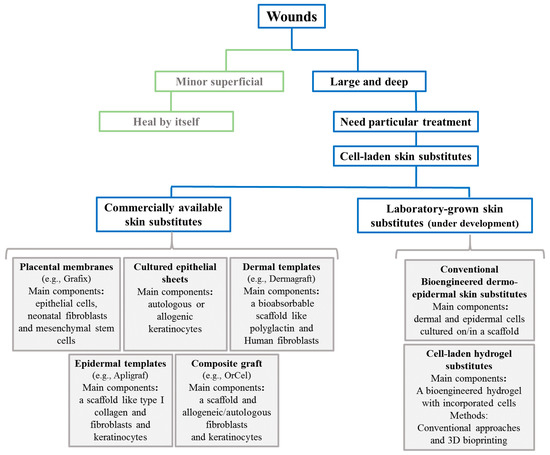
Figure 1. A schematic classification and summary of different commercial and bioengineered skin substitutes for large and hard-to-heal wounds.
This entry is adapted from the peer-reviewed paper 10.3390/app11041493
References
- Shevchenko, R.V.; James, S.E. A review of tissue-engineered skin bioconstructs available for skin reconstruction. J. R. Soc. Interface 2009, 7, 229–258.
- Lazarus, G.S.; Cooper, D.M.; Knighton, D.R.; Margolis, D.J.; Percoraro, R.E.; Rodeheaver, G.; Robson, M.C. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994, 2, 165–170.
- Tavakoli, S.; Mokhtari, H.; Kharaziha, M.; Kermanpur, A.; Talebi, A.; Moshtaghian, J. A multifunctional nanocomposite spray dressing of Kappa-carrageenan-polydopamine modified ZnO/L-glutamic acid for diabetic wounds. Mater. Sci. Eng. C 2020, 111, 110837.
- Kanitakis, J. Anatomy, histology and immunohistochemistry of normal human skin. Eur. J. Dermatol. 2002, 12, 390–401.
- Schmook, F.P.; Meingassner, J.G.; Billich, A. Comparison of human skin or epidermis models with human and animal skin in in-vitro percutaneous absorption. Int. J. Pharm. 2001, 215, 51–56.
- Tavakoli, S.; Klar, A.S. Advanced Hydrogels as Wound Dressings. Biomolecules 2020, 10, 1169.
- Subramanian, A.; Krishnan, U.M.; Sethuraman, S. Skin tissue regeneration. In Electrospinning for Tissue Regeneration; Woodhead Publishing: Cambridge, UK, 2011; Volume 1, pp. 298–316.
- Rowan, M.P.; Cancio, L.C.; Elster, E.A.; Burmeister, D.M.; Rose, L.F.; Natesan, S.; Chan, R.K.; Christy, R.J.; Chung, K.K. Burn wound healing and treatment: Review and advancements. Crit. Care 2015, 19, 1–12.
- Boateng, J.S.; Matthews, K.H.; Stevens, H.N.; Eccleston, G.M. Wound Healing Dressings and Drug Delivery Systems: A Review. J. Pharm. Sci. 2008, 97, 2892–2923.
- Gaur, M.; Dobke, M.K.; Lunyak, V.V. Mesenchymal Stem Cells from Adipose Tissue in Clinical Applications for Dermatological Indications and Skin Aging. Int. J. Mol. Sci. 2017, 18, 208.
- Roupé, K.M.; Nybo, M.; Sjöbring, U.; Alberius, P.; Schmidtchen, A.; Sørensen, O.E.; Roup, M.N.K.M. Injury Is a Major Inducer of Epidermal Innate Immune Responses during Wound Healing. J. Investig. Dermatol. 2010, 130, 1167–1177.
- Klar, A.S.; Güven, S.; Zimoch, J.; Zapiórkowska, N.A.; Biedermann, T.; Böttcher-Haberzeth, S.; Meuli-Simmen, C.; Martin, I.; Scherberich, A.; Reichmann, E.; et al. Characterization of vasculogenic potential of human adipose-derived endothelial cells in a three-dimensional vascularized skin substitute. Pediatr. Surg. Int. 2015, 32, 17–27.
- Klar, A.S.; Michalak-Mićka, K.; Biedermann, T.; Simmen-Meuli, C.; Reichmann, E.; Meuli, M. Characterization of M1 and M2 polarization of macrophages in vascularized human dermo-epidermal skin substitutes in vivo. Pediatr. Surg. Int. 2017, 34, 129–135.
- Delavary, B.M.; Van Der Veer, W.M.; Van Egmond, M.; Niessen, F.B.; Beelen, R.H. Macrophages in skin injury and repair. Immunobiology 2011, 216, 753–762.
- Sukari, H.A.; Khoo, T.L.; Yussof, S.J. Biologic and synthetic skin substitutes: An overview. Indian J Plast Surg 2010, 43, 23–28.
- Harding, K.G.; Morris, H.L.; Patel, G.K. Science, medicine, and the future: Healing chronic wounds. BMJ 2002, 324, 160–163.
- Guo, S.; DiPietro, L.A. Critical Review in Oral Biology & Medicine: Factors Affecting Wound Healing. J. Dent. Res. 2010, 89, 219–229.
- Johnson, K.E.; Wilgus, T.A. Vascular Endothelial Growth Factor and Angiogenesis in the Regulation of Cutaneous Wound Repair. Adv. Wound Care (New Rochelle) 2014, 3, 647–661.
- Demidova-Rice, T.N.; Durham, J.T.; Herman, I.M. Wound Healing Angiogenesis: Innovations and Challenges in Acute and Chronic Wound Healing. Adv. Wound Care 2012, 1, 17–22.
- Klar, A.S.; Güven, S.; Biedermann, T.; Luginbühl, J.; Böttcher-Haberzeth, S.; Meuli-Simmen, C.; Meuli, M.; Martin, I.; Scherberich, A.; Reichmann, E. Tissue-engineered dermo-epidermal skin grafts prevascularized with adipose-derived cells. Biomaterials 2014, 35, 5065–5078.
- Frueh, F.S.; Macedo, N.; Calcagni, M.; Giovanoli, P.; Lindenblatt, N. The Crucial Role of Vascularization and Lymphangiogenesis in Skin Reconstruction. Eur. Surg. Res. 2018, 59, 242–254.
- Shahin, H.; Elmasry, M.; Steinvall, L.; Söberg, F.; Serafi, A. Vascularization is the next challenge for skin tissue engineering as a solution for burn management. Burns Trauma 2020, 8, 022.
- Klar, A.S.; Böttcher-Haberzeth, S.; Biedermann, T.; Schiestl, C.; Reichmann, E.; Meuli, M. Analysis of blood and lymph vascularization patterns in tissue-engineered human dermo-epidermal skin analogs of different pigmentation. Pediatr. Surg. Int. 2014, 30, 223–231.
- Pourmoussa, A.; Gardner, D.J.; Johnson, M.B.; Wong, A.K. An update and review of cell-based wound dressings and their integration into clinical practice. Ann. Transl. Med. 2016, 4, 457.
- Klar, A.S.; Biedermann, T.; Simmen-Meuli, C.; Reichmann, E.; Meuli, M. Comparison of in vivo immune responses following transplantation of vascularized and non-vascularized human dermo-epidermal skin substitutes. Pediatr. Surg. Int. 2016, 33, 377–382.
- Pogorielov, M.; Hapchenko, A.; Pogorielov, O.O.M. Tissue Engineering: Challenges and Selected Application. Adv. Tissue Eng. Regen. Med. Open Access 2017, 3, 1–6.
- Li, C.; Guan, G.; Reif, R.; Huang, Z.; Wang, R.K. Determining elastic properties of skin by measuring surface waves from an impulse mechanical stimulus using phase-sensitive optical coherence tomography. J. R. Soc. Interface 2011, 9, 831–841.
