eHealth interventions play a growing role in shaping the future healthcare system. The integration of eHealth interventions can enhance the efficiency and quality of patient management and optimize the course of treatment for chronically ill patients.
- digital health
- eHealth
- multiple sclerosis
1. Introduction
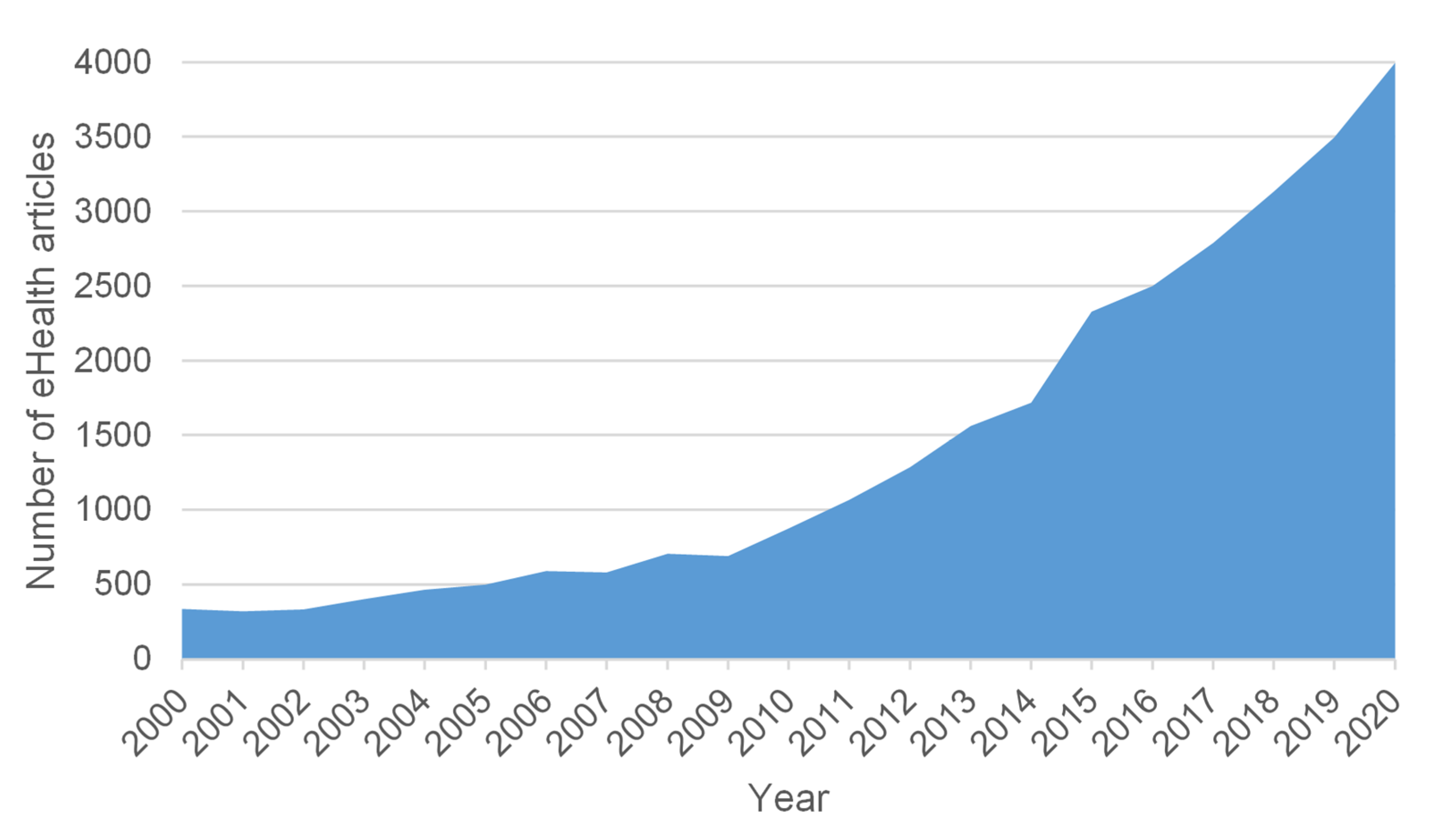
In a society of growing digital proficiency, 80 percent of all Internet users go online to seek health information [1]. The use of health information technology (HIT) in healthcare has become increasingly prominent since the late 1980s [2]. Early HIT mainly referred to the digitization of traditional processes in the public health sector. With the development of new technologies, the term has become more general [3]. Focusing on eHealth-assisted patient management, we have also witnessed a steady increase of research interest in the last two decades (Figure 1) [4].
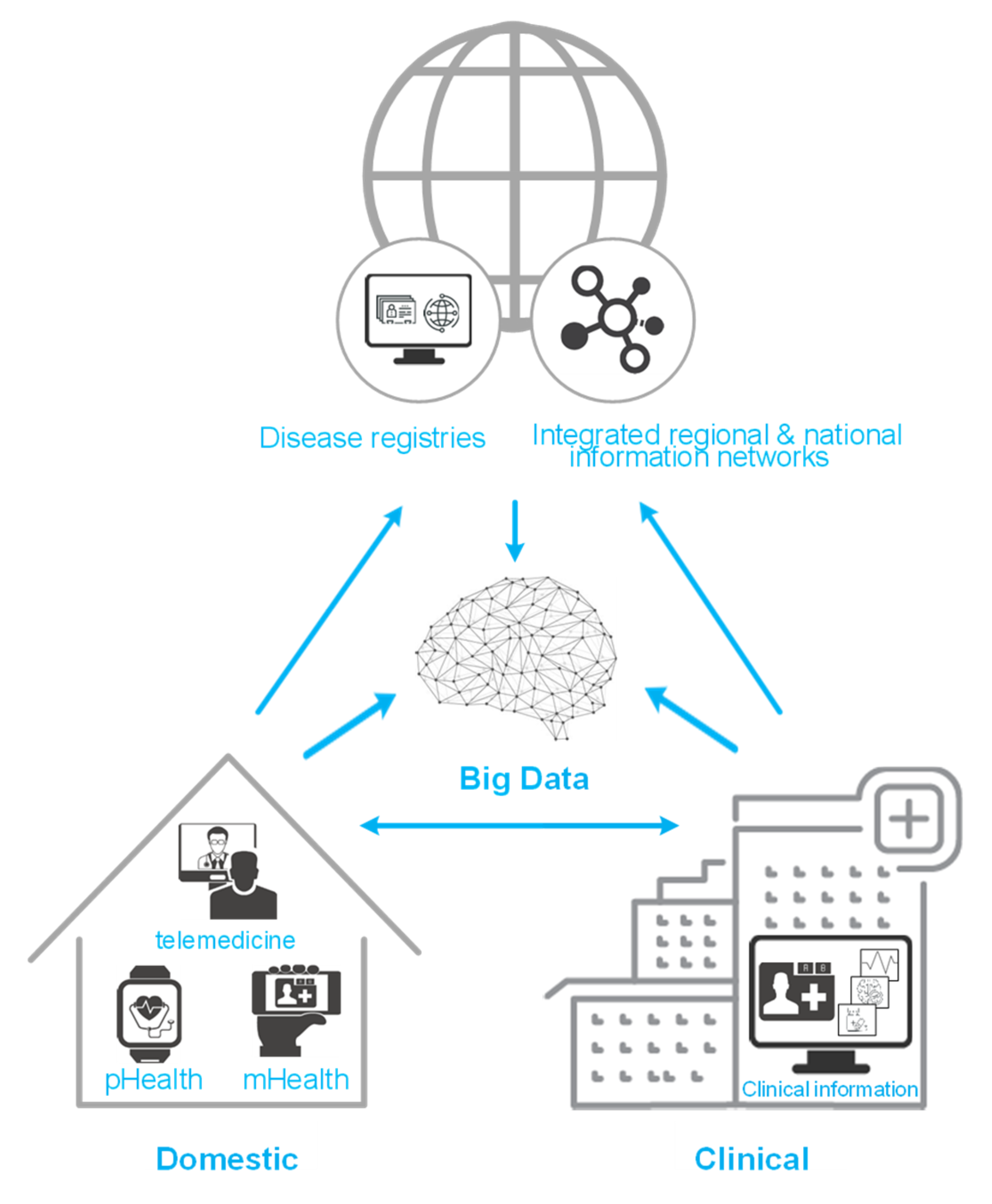
Several approaches exist to defining constructs such as eHealth, telehealth and other HIT terms [5], but we want to provide a common ground for our review: eHealth is defined as “an emerging field in the intersection of medical informatics, public health and business” using information and communication technologies [3]. Such technologies are shown in Figure 2 and may contain personalized health (pHealth), telemedicine and telecare, mobile health (mHealth), clinical information systems (e.g., electronic health record), disease registries and other non-clinical systems, integrated regional and national information networks and Big Data approaches [2][6][7].
Good eHealth interventions are easy to use and should enhance efficiency and quality, translate evidence-based knowledge into practice, enable patient empowerment by giving them more control over their health, education and information exchange as well as facilitate specific interventions [8][9][10]. Especially for people with chronic diseases, adequate treatment and monitoring are difficult to supply [11]. eHealth interventions are an effective way to identify the health needs of people with complex chronic diseases and may meet their long-term care needs because many areas can be addressed and acceptance as well as satisfaction with such interventions is supposed to be high [12].
Use Case Multiple Sclerosis
An important chronic disease is multiple sclerosis (MS), one of the world’s most common neurological disorders of young adults that results in central demyelination and neurodegeneration causing multifocal neurological problems [13][14][15][16]. Usually, people with MS (pwMS) show their first symptoms at the age of 20 to 40 years; consequently, they live with this chronic disease for the following decades, which is why these patients may be important early adopters of emerging eHealth trends [17]. Additionally, their physical and cognitive impairments complicate traditional face-to-face interventions for pwMS. Such disabilities and the willingness to use digital media for communication with healthcare providers make MS an excellent model for innovative improvements in care delivery, including eHealth interventions [18][19][20]. In addition to individual disabilities, there are other circumstances that make a face-to-face visit even more challenging. On the one hand, these include geographical barriers. Long distances to specialists, especially in rural areas, mean an enormous effort for patients to obtain the required care. On the other hand, there are special situations such as the recent coronavirus disease (COVID-19) pandemic making smooth patient care problematic. Reducing person-to-person contact in order to stop a rapid spread of the disease is a preventive measure against proliferation [21]. This commandment and the fear of possible infection lead patients to cancel their medical appointments. To enable continuous patient care without a face-to-face visit and to overcome geographical barriers [22], eHealth interventions can serve as a helpful tool. By extending the collection of health data electronically beyond the consultation itself, a continuous recording of all facets of this complex disease may enable a safe and efficient management of the individual disease course. Therefore, HIT serves as a support for medical and health policy practice [11] that reduces costs. Since the quality of care achieved by eHealth interventions may deviate from traditional face-to-face interactions, cost reductions and treatment outcomes need to be balanced. To optimize the specific treatments of pwMS, eHealth interventions can support physicians in long-term documentation and management of treatment steps in any disease-modifying therapy (DMT) [23].
2. Advantages
EHealth interventions are helpful tools to close the supply shortfall in the healthcare system and to improve the care of chronically ill patients because they can present the course of illness more comprehensively and more accurately than face-to-face visits. They are designed for various use cases and different users. On the one hand, individual health parameters of patients can be entered and interactions with physicians or other patients can take place. On the other hand, health systems are interconnected to exchange data, give feedback and receive optimal disease management. For the implementation of eHealth interventions, a number of requirements for various deficits in relation to different diseases must be considered. Well-designed interventions can provide relief to the patient and all other persons involved in the recovery process if the digital divide in chronic care can be minimized [24].
PwMS may be an ideal, trend-adopting group of eHealth users. There are already several eHealth interventions on the market for MS, specifically targeted to the impairments of the disease. One example is the MSDS3D. A special feature of MSDS3D is the focus on the management of individual DMTs, which ensures a comprehensive and safe treatment of the patient. The system also includes a module focusing on treatment satisfaction. Treatment satisfaction is an important factor for patient compliance and an indication of comorbidity; therefore, it should be added to any eHealth intervention directly [25]. Being connected to MSDS3D via the IBMS portal, both physicians and patients are able to follow the course of disease exactly. In addition, patients and their family can exchange information with healtcare professionals via the platform and obtain the latest information.
Future research should focus on patients’ self-monitoring to empower them in viewing and understanding their disease progression independently of the physician and in making self-determined decisions regarding treatment. For this, interventions should not only be able to display data and results in an easy-to-understand manner but should also enable specific treatment options for each outcome (e.g., specific exercises for foot drop; different medication options). An option to make appointments with specialists would complement the intervention. This all leads us to a system that combines all health-related aspects in a patient- centered eHealth approach.
This entry is adapted from the peer-reviewed paper 10.3390/brainsci11020180
References
- Ploeg, J.; Markle-Reid, M.; Valaitis, R.; McAiney, C.; Duggleby, W.; Bartholomew, A.; Sherifali, D. Web-based interventions to improve mental health, general caregiving outcomes, and general health for informal caregivers of adults with chronic conditions living in the community: Rapid evidence review. J. Med. Internet Res. 2017, 19, e263.
- Gray, C.S.; Mercer, S.; Palen, T.; McKinstry, B.; Hendry, A. EHealth advances in support of people with complex care needs: Case examples from Canada, Scotland and the US. Healthc. Q. 2016, 19, 29–37.
- Eysenbach, G. What is e-health? J. Med. Internet Res. 2001, 3, E20.
- Barello, S.; Triberti, S.; Graffigna, G.; Libreri, C.; Serino, S.; Hibbard, J.; Riva, G. EHealth for patient engagement: A systematic review. Front. Psychol. 2015, 6, 2013.
- Oh, H.; Rizo, C.; Enkin, M.; Jadad, A. What is eHealth, (3): A systematic review of published definitions. J. Med. Internet Res. 2005, 7, e1.
- Saner, H.; van der Velde, E. eHealth in cardiovascular medicine: A clinical update. Eur. J. Prev. Cardiol. 2016, 23, 5–12.
- Vorderstrasse, A.; Lewinski, A.; Melkus, G.D.; Johnson, C. social support for diabetes self-management via eHealth interventions. Curr. Diabetes Rep. 2016, 16, 56.
- Allam, A.; Kostova, Z.; Nakamoto, K.; Schulz, P.J. The effect of social support features and gamification on a Web-based intervention for rheumatoid arthritis patients: Randomized controlled trial. J. Med. Internet Res. 2015, 17, e14.
- Marziniak, M.; Brichetto, G.; Feys, P.; Meyding-Lamade, U.; Vernon, K.; Meuth, S.G. The use of digital and remote communication technologies as a tool for multiple sclerosis management: Narrative review. JMIR Rehabil. Assist. Technol. 2018, 5, e5.
- Conway, N.; Webster, C.; Smith, B.; Wake, D. eHealth and the use of individually tailored information: A systematic review. Health Inform. J. 2017, 23, 218–233.
- Abaza, H.; Marschollek, M. mHealth application areas and technology combinations *. A comparison of literature from high and low/middle income countries. Methods Inf. Med. 2017, 56, e105–e122.
- Wallin, E.E.; Mattsson, S.; Olsson, E.M. The preference for internet-based psychological interventions by individuals without past or current use of mental health treatment delivered online: A survey study with mixed-methods analysis. JMIR Ment. Health 2016, 3, e25.
- Browne, P.; Chandraratna, D.; Angood, C.; Tremlett, H.; Baker, C.; Taylor, B.V.; Thompson, A.J. Atlas of multiple sclerosis 2013: A growing global problem with widespread inequity. Neurology 2014, 83, 1022–1024.
- Goldenberg, M.M. Multiple sclerosis review. P T Peer Rev. J. Formul. Manag. 2012, 37, 175–184.
- Khan, F.; Amatya, B.; Kesselring, J.; Galea, M. Telerehabilitation for persons with multiple sclerosis. Cochrane Database Syst. Rev. 2015, 4, CD010508.
- Vickrey, B.G.; Hays, R.D.; Harooni, R.; Myers, L.W.; Ellison, G.W. A health-related quality of life measure for multiple sclerosis. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 1995, 4, 187–206.
- Nielsen, A.S.; Halamka, J.D.; Kinkel, R.P. Internet portal use in an academic multiple sclerosis center. J. Am. Med. Inform. Assoc. JAMIA 2012, 19, 128–133.
- Atreja, A.; Mehta, N.; Miller, D.; Moore, S.; Nichols, K.; Miller, H.; Harris, C.M. One size does not fit all: Using qualitative methods to inform the development of an Internet portal for multiple sclerosis patients. AMIA Annu. Symp. Proc. AMIA Symp. 2005, 2005, 16–20.
- Haase, R.; Schultheiss, T.; Kempcke, R.; Thomas, K.; Ziemssen, T. Use and acceptance of electronic communication by patients with multiple sclerosis: A multicenter questionnaire study. J. Med. Internet Res. 2012, 14, e135.
- Leavitt, V.M.; Riley, C.S.; de Jager, P.L.; Bloom, S. eSupport: Feasibility trial of telehealth support group participation to reduce loneliness in multiple sclerosis. Mult. Scler. 2019, 26, 1797–1800.
- Prem, K.; Liu, Y.; Russell, T.W.; Kucharski, A.J.; Eggo, R.M.; Davies, N.; Jit, M.; Klepac, P. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health 2020, 5, e261–e270.
- Marrie, R.A.; Leung, S.; Tyry, T.; Cutter, G.R.; Fox, R.; Salter, A. Use of eHealth and mHealth technology by persons with multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 27, 13–19.
- Hobart, J.; Bowen, A.; Pepper, G.; Crofts, H.; Eberhard, L.; Berger, T.; Boyko, A.; Boz, C.; Butzkueven, H.; Celius, E.G.; et al. International consensus on quality standards for brain health-focused care in multiple sclerosis. Mult. Scler. 2018, 25, 1809–1818.
- Gammon, D.; Berntsen, G.K.; Koricho, A.T.; Sygna, K.; Ruland, C. The chronic care model and technological research and innovation: A scoping review at the crossroads. J. Med. Internet Res. 2015, 17, e25.
- Zettl, U.K.; Bauer-Steinhusen, U.; Glaser, T.; Hechenbichler, K.; Limmroth, V. Evaluation of an electronic diary for improvement of adherence to interferon beta-1b in patients with multiple sclerosis: Design and baseline results of an observational cohort study. BMC Neurol. 2013, 13, 117.
