Breast-conserving surgery’s main goal is to fully remove the tumor with clear margins, while avoiding resection of healthy breast tissue in order to achieve better cosmetic results.
- breast cancer
- breast-conserving surgery
- image-guided localization
1. Introduction
Breast cancer (BC) is the most commonly diagnosed cancer and the leading cause of cancer-related death among women [1]. A successful BC treatment is based on a multidisciplinary use of surgery, chemotherapy and radiation therapy, with surgery as the central component of treatment for early-stage breast cancer [2,3]. Breast-conserving surgery (BCS) followed by adjuvant radiotherapy, known as breast conservation therapy (BCT), has become the alternative treatment to mastectomy for early stage breast cancer because of equivalent survival and lower morbidity [4,5,6].
Local recurrence after BCS is strongly correlated to the surgical margin status, as demonstrated by a large number of follow-up studies [7,8,9,10,11]. The main goal of BCS is to fully remove the tumor with clear margins, while avoiding resection of healthy breast tissue in order to achieve better cosmetic results. Image-guided preoperative localization is mandatory for guiding surgery of non-palpable lesions or surgically relevant extension of palpable lesions to improve both oncological and cosmetic outcomes [12,13]. Over the last decade, methods for preoperative localization of breast lesions for BCS have evolved rapidly due to innovative techniques and discovery of novel agents. However, cooperation and communication between breast surgeons and radiologists still play a crucial role.
Different image guided localization techniques are variably used in different institutions depending on personal choices, skills and available technologies. As a general rule, the method chosen should be the most precise to localize the lesion or marker left after biopsy, thus improving free margin rates and decreasing operative time, and possibly cause little to no discomfort to the patient. Preoperative breast lesions localization techniques currently available are wire localization, carbon marking, radio-guided occult lesion localization (ROLL), radioactive seed localization (RSL), magnetic seed localization and non-radioactive radar localization, intraoperative ultrasound and preoperative skin tattoo localization (Table 1). In this article, we provide an overview of current literature of all commercially available techniques. The aim of this review is to educate practicing radiologists and breast surgeons so they can knowingly select new techniques to improve patient care.
Table 1. Comparison of different localization techniques. Abbreviations: ROLL = radio-guided occult lesion localization; RSL = radioactive seed localization; Magseed = magnetic seed localization; IOUS = intraoperative ultrasound; Skin tattoo = preoperative localization with skin tattoo; OR = operating room; US = ultrasound; MRI = magnetic resonance imaging. * Success is defined as removal of target lesion. ** Authors’ experience.
| Technique | Materials/Procedures | Advantages | Disadvantages | Success * Rate | Clear Margins Rate |
|---|---|---|---|---|---|
| Wire localization | Wire Preloaded needle introducer |
Simple Cost-effective Different kinds of image-guidance |
Wire migration Scheduling difficulties Limits surgical decisions |
97.5% [14] | 70.8–87.4% [15] |
| Carbon marking | Diluted charcoal powder | Simple Different kinds of image-guidance Cost-effective Cannot dislodge Scheduling flexibility |
Carbon can distort or obscure lesion Unfit for large breasts Unfit for multifocal or extensive lesions |
99% [16] | 61–85% [17,18] |
| ROLL | Nuclear radiotracer Technetium 99 Gamma ray probe |
Different kinds of image-guidance Does not limit surgeon |
Scheduling difficulties Radiation Cost |
95–99% [19] | 92% [20,21] |
| RSL | Iodine 125 seed Preloaded needle introducer Gamma probe set for I-125 |
Scheduling flexibility Does not limit surgeon Different kinds of image-guidance |
Radiation Not repositionable after deployment |
100% [22,23] | 73.5–96.7% [22,23] |
| Magseed | Paramagnetic seed Preloaded needle introducer |
Scheduling flexibility No radiation Does not limit surgeon |
Cost Not repositionable after deployment Non magnetizable surgical equipment MRI artifacts |
99.86% [24,25,26,27] | 88.75% [24] |
| Radiofrequency identification tags | Radiofrequency reflector Needle introducer Detector |
Scheduling flexibility No radiation Does not limit surgeon |
Cost Depth limit Not repositionable after deployment Interference with halogen lights in the OR |
97–100% [28,29] | 85–100% [28,29,30] |
| IOUS | Portable or OR-stationed US machine and sterile transducer cover | Scheduling flexibility No radiation Does not limit surgeon Non-invasive |
Unemployable in US-invisible lesions Surgeon learning curve Interference with air during dissection |
100% [31,32,33,34,35] | 81–97% [32,34] |
| Skin tattoo | Dermographic marker Lead markers |
Simple and safe Cost-effective Non-invasive Different kinds of image-guidance Does not limit surgeon |
Scheduling difficulties Inability to depict marker |
99.5% ** | 95.9% ** |
2. Preoperative Localization with a Skin Tattoo
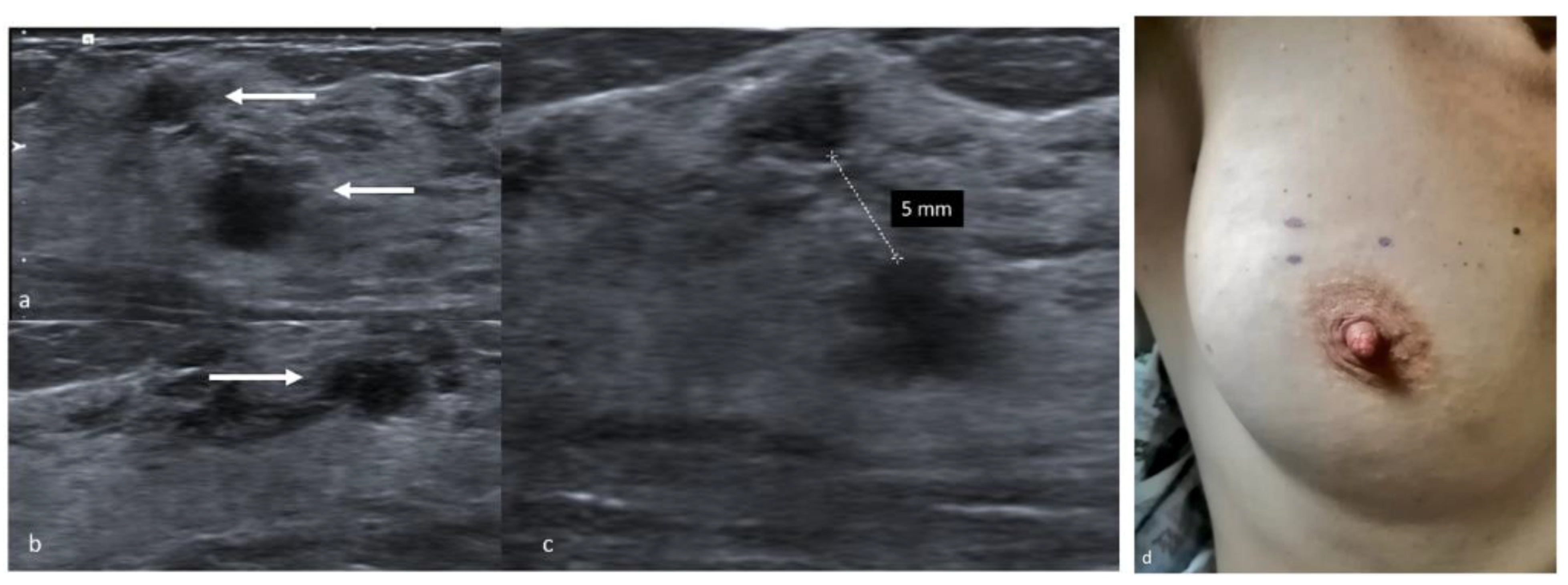
Preoperative localization with a skin tattoo is a simple and safe technique amply utilized in our centre, as it is easily performed, extremely well tolerated by patients and effective in terms of successful excision and clear margin rates. This method can be carried out by acquiring either sonographic or mammographic images, depending on the type of lesion, but ultrasounds are employed whenever possible because the procedure is easier. In this case, patients lie in the supine position with their arms extended to mimic the position held during surgery. The tumor is located, and its distance from the skin surface is measured taking care not to apply pressure with the probe, so as to report accurately the depth of the tumor in relation to the skin surface [65]. The distance between the lesion, the nipple and the pectoralis major muscle is also measured, as is the distance between separate lesions in case of multifocal or multicentric disease [44,66]. Radiologists with experience in this technique visualize the tumors at their largest diameter to achieve the optimal correspondence between the lesion and the skin markers. The tumor’s projection on the skin surface is pinpointed with a dermographic skin marker and the drawing is covered to avoid accidental erasure (Figure 4). The whole procedure, performed by an experienced radiologist, takes 5–10 min and provides minimum patient discomfort. Limitations include poor results in case of sonographically invisible lesions, microcalcifications or biopsy markers, but are easily overcome by implementing this technique with a mammographic approach. Stereotactic-guided skin marking is also a non-invasive technique, albeit it provides a little more discomfort to the patient due to breast compression. Mammograms are acquired in double projection and measurements are performed on the images to determine the distance between the lesion and the nipple, the skin surface and the fascia.
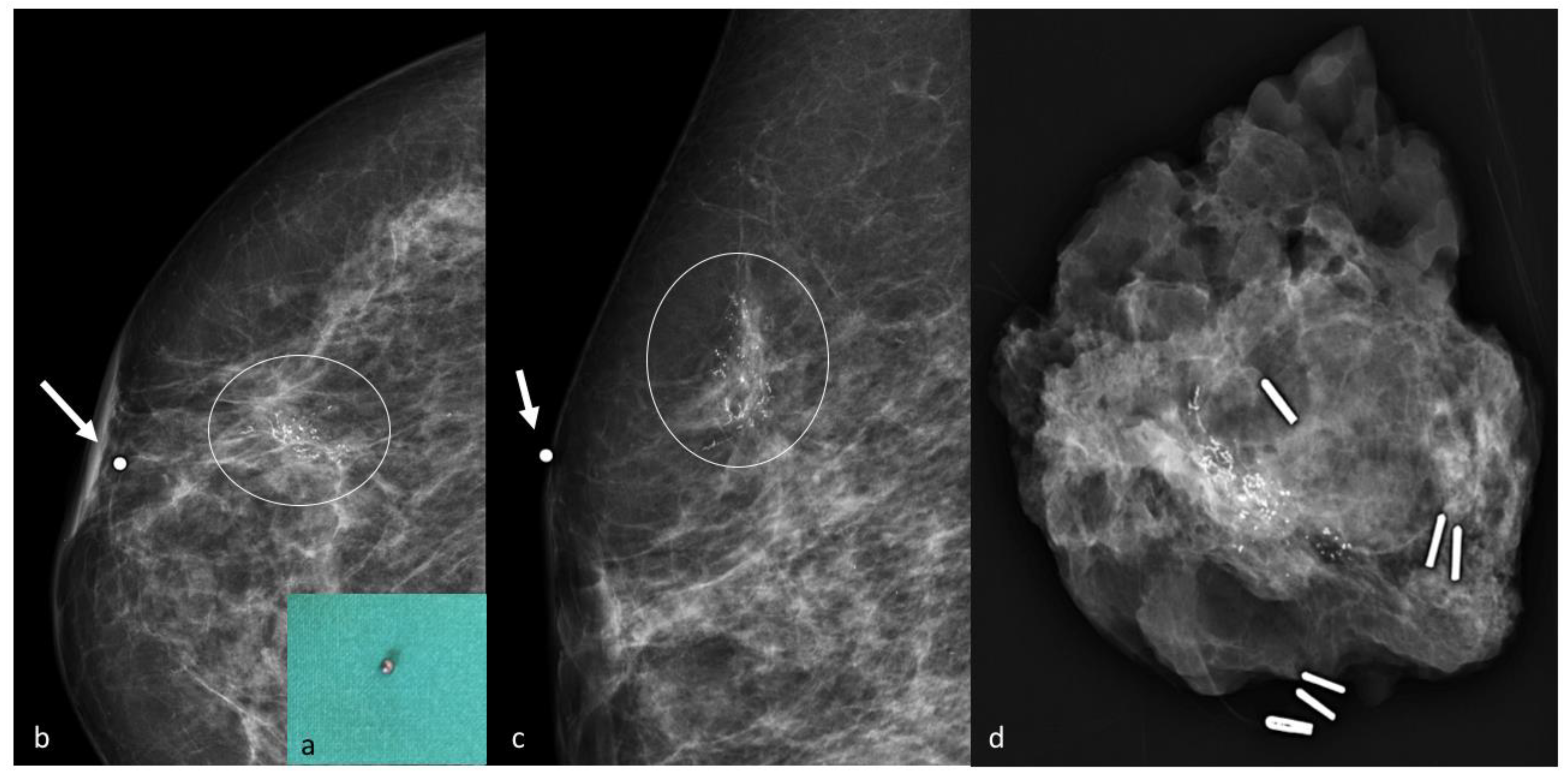
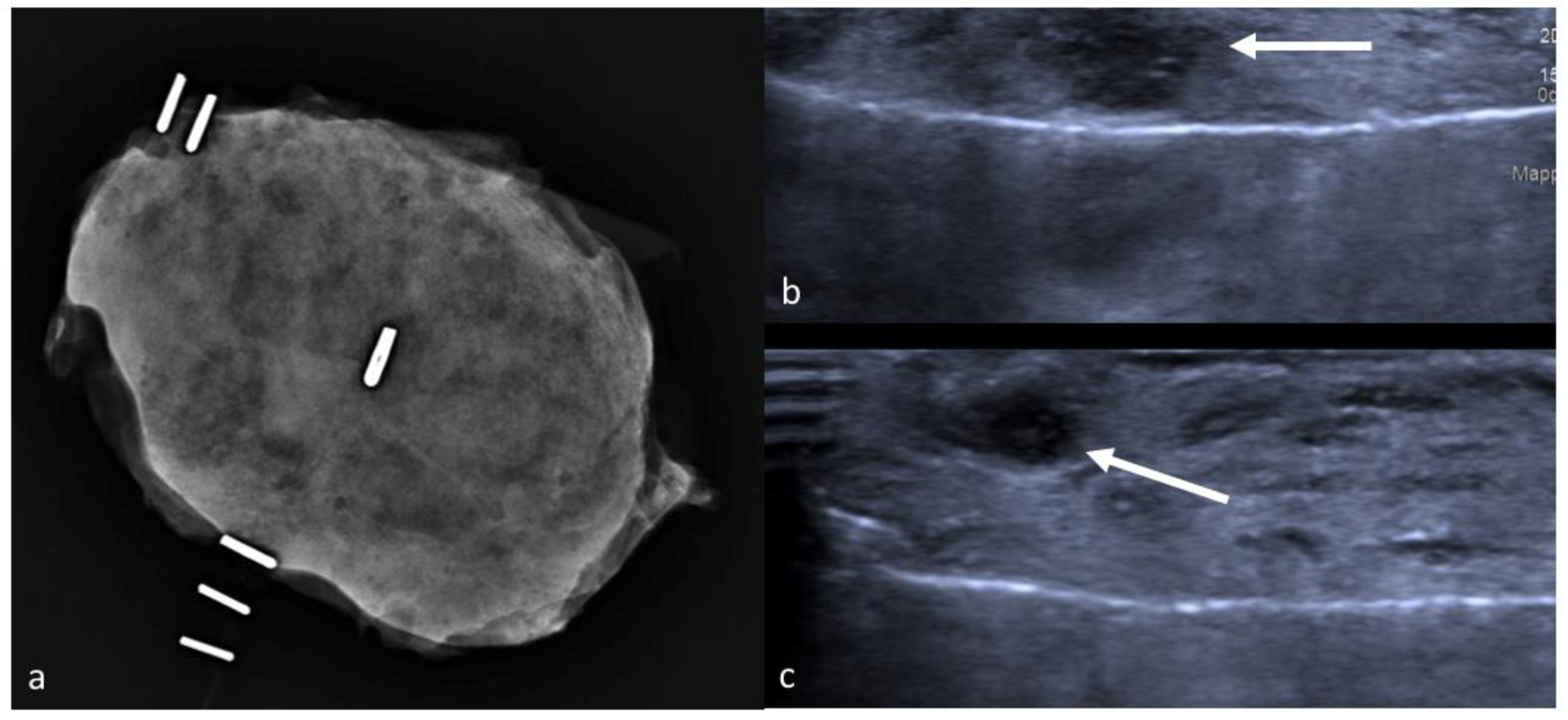
The radiologist then estimates the projection of the tumor on the skin surface and positions a lead marker in the corresponding spot. In case of bigger lesions, such as extensive microcalcifications, or multifocal disease, multiple lead markers can be employed to determine lesion margins. A second stereotactic pair of images is acquired to confirm the correct localization, and in case of inaccurate positioning, the lead markers can be repositioned more accurately and confirmed by a further mammogram [67] (Figure 5). At the end of the procedure the lead markers are removed, and the skin tattoo is drawn in their place. In the operating room, the mark is exposed and retraced with a specific marker resistant to antiseptic solutions, and painting and draping procedures are carried out carefully without wiping out the ink. Our centre strongly advocates pursuit of the maximum aesthetic result achievable with oncological safety, and because this localization technique employs only a temporary skin tattoo, the surgeon is granted total liberty in choice of incision and oncoplastic technique. The skin flap is dissected in the direction of the tattoo, then the incision is deepened and a lumpectomy is carried out taking into account tumor depth measured during the preoperative localization. In some cases, a non-palpable lesion becomes palpable after dissection of the skin flap, allowing the surgeon to easily complete the excision, however in most cases the excision has to be conducted by reassessing the original position of the skin mark from time to time. Once the excision is completed, metallic clips are placed on the orienting sutures in different numbers, so as to recognize margins in the specimen X-ray. The sample is then placed into a transparent plastic bag and sent to the Radiology Department, and mammograms are acquired in double projection. The tumor is usually visible as a radiopaque nodule, and its position inside the lumpectomy specimen is described as either well centered or close to one or more surgical margins, and reported to the operating surgeon. In dense, glandular specimens the nodule can be difficult to distinguish from the surrounding mammary parenchyma: in these cases, the exam can be completed with a specimen ultrasound [68] (Figure 6). If close margins are detected in either technique the surgeon can acquire further cavity shave margins on the affected border.
This technique is quick, easily performed by breast radiologists and extremely cost-effective. It does not require equipment that is not normally present in any breast surgery department, and is therefore feasible even with scarce resources. Limitations include accurate scheduling to time the procedure before surgery thus avoiding accidental mark erasure, and a certain degree of experience by the surgeon in reassessing the tumor’s position based on the skin mark during dissection. Reports on this technique are widely deficient in the literature, however a preliminary analysis of the data from our high-volume centre examining the outcome of 199 lumpectomies performed for non-palpable breast tumors between August and December 2019 identified a global success rate of 99.5% (198/199) and a clear margins rate of 95.9% (192/199). As these rates did not differ significantly from other localization techniques, this method appears safe and especially ideal in the case of limited resources or spending reviews.
This entry is adapted from the peer-reviewed paper 10.3390/jpm11020099
