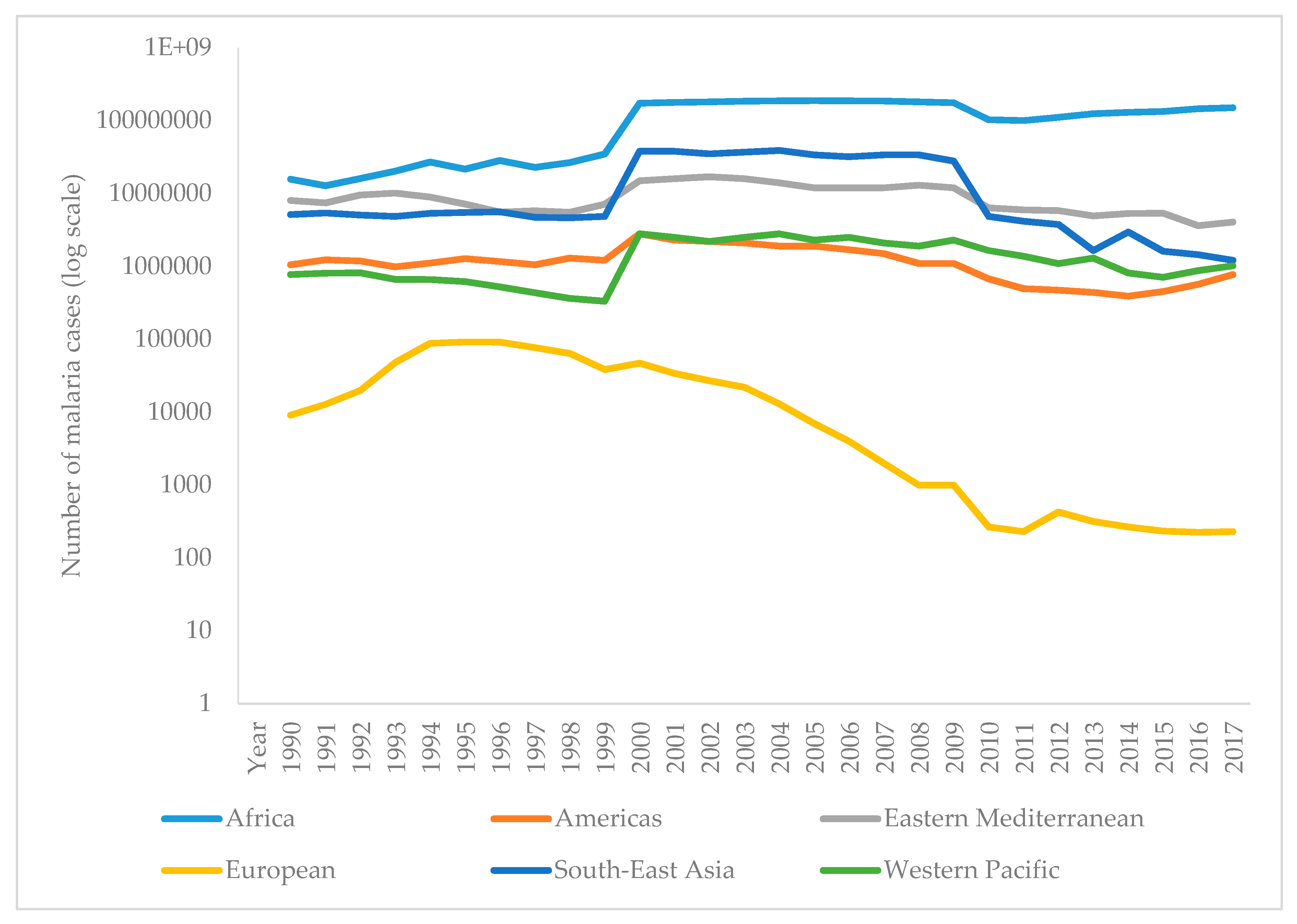
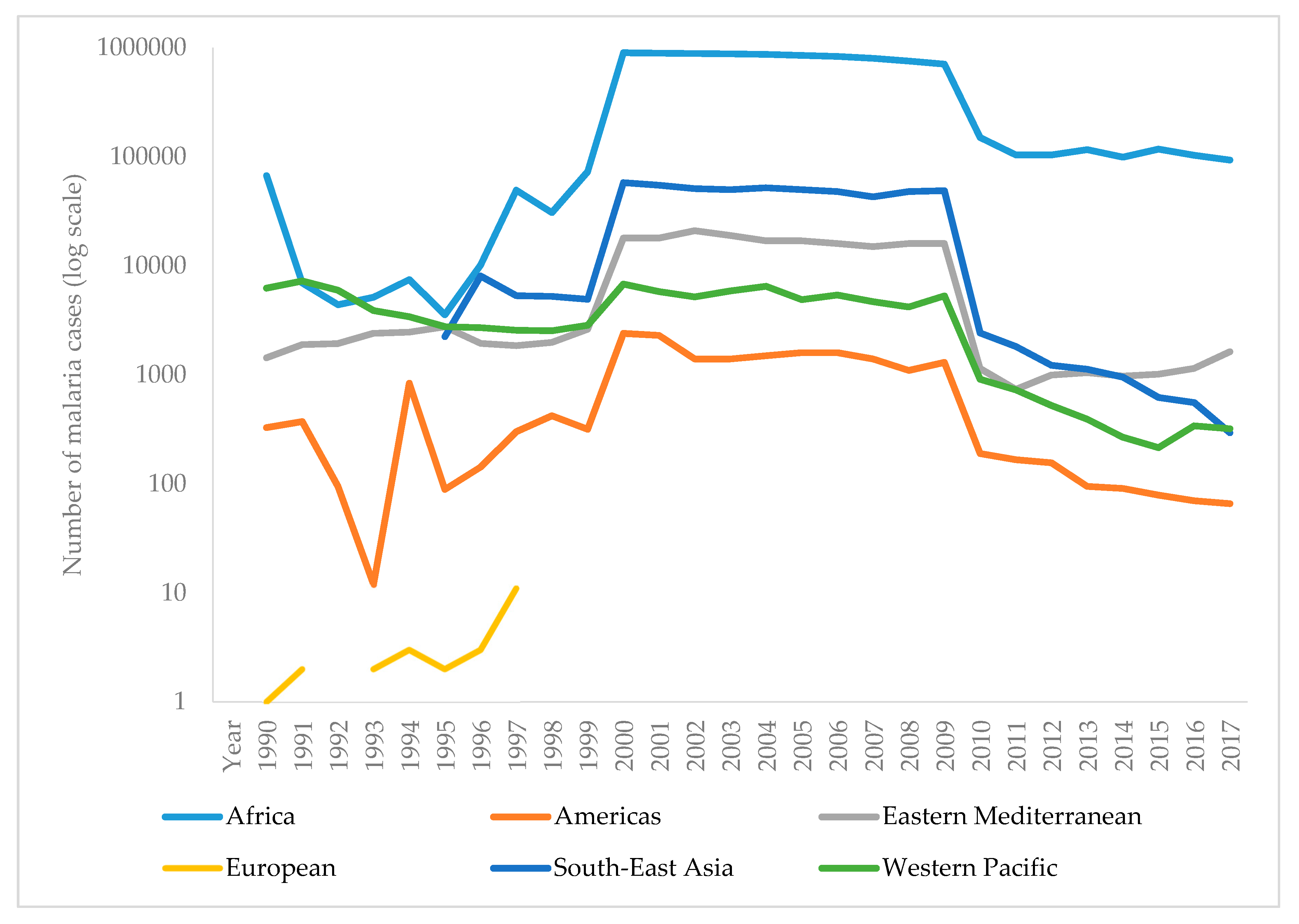
Malaria is a severe disease caused by parasites of the genus Plasmodium, which is transmitted to humans by a bite of an infected female mosquito of the species Anopheles. Malaria remains the leading cause of mortality around the world, and early diagnosis and fast-acting treatment prevent unwanted outcomes. It is the most common disease in Africa and some countries of Asia, while in the developed world malaria occurs as imported from endemic areas. The sweet sagewort plant was used as early as the second century BC to treat malaria fever in China. Much later, quinine started being used as an antimalaria drug. A global battle against malaria started in 1955. The World Health Organization carries out a malaria control program on a global scale, focusing on local strengthening of primary health care, early diagnosis of the disease, timely treatment, and disease prevention. Globally, the burden of malaria is lower than ten years ago. However, in the last few years, there has been an increase in the number of malaria cases around the world. It is moving towards targets established by the WHO, but that progress has slowed down.
- Anopheles
- antimalarials
- malaria
- Plasmodium
Introduction
Discovery of Malaria
The Development of Diagnostic Tests for Proving Malaria through History
| Advantages | Disadvantages | |
|---|---|---|
| Direct methods | ||
| Microscopic analysis | Fast test, cheap | Required much experience as well as equipment |
| Rapid diagnostic tests | Quick and simple | Less sensitive and accurate, price |
| Molecular tests | Correct determination of type, highly sensitive and accurate | Price, long-term in a large number of cases |
| Indirect methods | ||
| Indirect immunofluorescence | Specific, sensitive | Long time to perform, subjective evaluation of results |
| ELISA | Correct determination of type, specific, sensitive | Long time to perform, price |
Malaria Treatment through History
| Medication Name | Year of Discovery/Synthesis | Origin | Usage | Mechanism of Action | Side Effects | Advantages/Disadvantages |
|---|---|---|---|---|---|---|
| Quinine | 1600 | Cinchona tree, South America | Resistance to chloroquine, prophylaxis, and treatment of malaria | Inhibition of DNA and RNA synthesis | Headache, abortion, or congenital malformations if taken during pregnancy | Toxic, less effective than other medication |
| Chloroquine | 1934 | Synthesized by German scientist Hans Andersag | A most powerful remedy for the prophylaxis and treatment of malaria | Inhibition of DNA and RNA synthesis | Gastrointestinal disturbances, headache, skin irritation | Developed resistance of most strains of P. falciparum to the medication |
| Primaquine | 1953 | The 8-aminoquinoline derivative | Infections with P. vivax and P. ovale, prophylaxis and treatment of malaria | Interferes in transport chain of electrons and destroys parasite mitochondria | Anorexia, nausea, anemia, headaches, contraindicated in pregnancy and children under 4 years of age | Prevent relapse in P. vivax and P. ovale infection |
| Doxycycline | 1960 | Pfizer Inc. New York | Prophylaxis in areas with chloroquine resistance and against mefloquine-resistant P. falciparum | Inhibition of protein synthesis by binding to 30S ribosomal subunit | Gastrointestinal disorders, nausea, vomiting, photosensitivity | Effective and cheap, use for treatment and prophylaxis in all malarious areas |
| Mefloquine | 1971 | USA army and WHO | Multiresistant P. falciparum strains, prophylaxis, and treatment of malaria | Damage to parasite membrane | Gastrointestinal disorders, CNS disorder, contraindicated in pregnancy and patients with epilepsy | Partial resistance, brain damage |
| Proguanil (chloroguanide) | 1953 | Biguanide derivate | Prophylaxis in infections with P. falciparum | Inhibition of DNA synthesis | Digestive problems only in large doses | The least toxic antimalarial drug |
| Pyrimethamine | 1953 | Pyrimidine derivatives | For tissue parasites, prophylaxis, and treatment of malaria | Folic acid antagonist | Gastrointestinal disorders, neuropathy, in high doses also megaloblastic anemia | The rapid development of resistance |
| Atovaquone/proguanil | 2000 | Ubiquinone analog | For the prophylaxis and treatment of malaria | Inhibition of cytochrome bc1 in Plasmodium | Nausea, vomiting, diarrhea, headache, dizziness, anxiety, difficulty falling asleep, rash, fever | Most commonly used, fewer side effects and more expensive than mefloquine, P. falciparum resistance |
Malaria in Europe
Malaria in Croatia
Malaria Trends in the World
References
- World Health Organization. World Malaria Report 2018; WHO: Geneva, Switzerland,
- White, N.J.N.; Pukrittayakamee, S.; Hien, T.T.T.; Faiz, M.A.; Mokuolu, O.A.O.; Dondorp, A.A.M. Malaria. Lancet 2014, 383, 723–735, doi:10.1016/S0140-6736(13)60024-0.
- Pan American Health Organization; World Health Organization. Epidemiological Alert, Increase of Malaria in the Americas; PAHO: Washington, DC, USA, 2018.
- Dhiman, S. Are malaria elimination efforts on right track? An analysis of gains achieved and challenges ahead. Dis. Poverty 2019, 8, 14, doi:10.1186/s40249-019-0524-x.
- Walker, N.; Nadjm, B.; Whitty, C. Malaria. Medicine 2017, 42, 52–58, doi:10.1016/j.mpmed.2013.11.011.
- Antinori, S.; Galimberti, L.; Milazzo, L.; Corbellino, M. Biology of human malaria plasmodia including Plasmodium knowlesi. J. Hematol. Infect. Dis. 2012, 4, e2012013, doi:10.4084/MJHID.2012.013.
- Ashley, E.A.; Pyae Phyo, A.; Woodrow, C.J. Malaria. Lancet 2018, 391, 1608–1621, doi:10.1016/S0140-6736(18)30324-6.
- Singh, B.; Daneshvar, C. Human Infections and Detection of Plasmodium knowlesi. Microbiol. Rev. 2013, 26, 165–184, doi:10.1128/CMR.00079-12.
- Vuk, I.; Rajic, Z.; Zorc, B. Malaria and antimalarial drugs. Farm Glas 2008, 64, 51–60.
- Soulard, V.; Bosson-Vanga, H.; Lorthiois, A.; Roucher, C.; Franetich, J.-F.; Zanghi, G.; Bordessoulles, M.; Tefit, M.; Thellier, M.; Morosan, S.; et al. Plasmodium falciparum full life cycle and Plasmodium ovale liver stages in humanized mice. Commun. 2015, 6, 7690, doi:10.1038/ncomms8690.
- Josling, G.A.; Llinás, M. Sexual development in Plasmodium parasites: Knowing when it’s time to commit. Rev. Genet. 2015, 13, 573–587, doi:10.1038/nrmicro3519.
- Blut, A. Untergruppe “Bewertung Blutassoziierter Krankheitserreger.” Transfus. Med. Hemother. 2009, 36, 48–60, doi:10.1159/000197327.
- Cowman, A.; Healer, J.; Marapana, D.; Marsh, K. Malaria, Biology and Disease. Cell 2016, 167, 610–624, doi:10.1016/j.cell.2016.07.055.
- Cartwright, F.; Biddis, M. Disease and History; Naklada Ljevak: Zagreb, Croatia, 2006.
- Lehrer, S. Vitezi Medicine; Prosveta: Beograd, Serbia, 1981.
- Moss, W.; Shah, S.; Morrow, R. The History of Malaria and its Control. Encycl. Public Health 2008, 389–398, doi:10.1016/B978-012373960-5.00374-9.
- Dugacki, V. Dr. Rudolf Battara operation in Nin in 1902, the first systematic battle attempt against malaria in Croatia. Jaderina 2005, 35, 33–40.
- Jovic, S. Istorija Medicine i Zdravstvene Kulture na tlu Dansnje Vojvodine 1718–1849 II; dio. Matica srpska, Srpska akademija nauka i umetnosti: Novi Sad, Serbia, 1998.
- Tan, S.Y.; Ahana, A. Charles Laveran (1845–1922), Nobel laureate pioneer of malaria. Med. J. 2009, 50, 657–658.
- Saifi, M.A.; Wajihullah, Siddiqui, M.I.; Al-Khalifa, M.S.; Malaria: Patterns of relapse and resistance. King Saud Univ. Sci. 2010, 22, 31–36, doi:10.1016/J.JKSUS.2009.12.005.
- Chu, C.S.; White, N.J. Management of relapsing Plasmodium vivax malaria. Expert Rev. Anti-Infect. Ther. 2016, 14, 885, doi:10.1080/14787210.2016.1220304.
- Murphy, S.C.; Shott, J.P.; Parikh, S.; Etter, P.; Prescott, W.R.; Stewart, V.A. Malaria diagnostics in clinical trials. J. Trop. Med. Hyg. 2013, 89, 824–839, doi:10.4269/ajtmh.12-0675.
- Tangpukdee, N.; Duangdee, C.; Wilairatana, P.; Krudsood, S. Malaria diagnosis, a brief review. Korean J. Parasitol. 2009, 47, 93–102, doi:10.3347/kjp.2009.47.2.93.
- Trampuz, A.; Jereb, M.; Muzlovic, I.; Prabhu, R.M. Clinical review, Severe malaria. Care 2003, 7, 315–323, doi:10.1186/cc2183.
- She, R.C.; Rawlins, M.L.; Mohl, R.; Perkins, S.L.; Hill, H.R.; Litwin, C.M. Comparison of Immunofluorescence Antibody Testing and Two Enzyme Immunoassays in the Serologic Diagnosis of Malaria. Travel Med. 2007, 14, 105–111, doi:10.1111/j.1708-8305.2006.00087.x.
- Oh, J.S.; Kim, J.S.; Lee, C.H.; Nam, D.H.; Kim, S.H.; Park, D.W.; Lee, C.K.; Lim, C.S.; Park, G.H. Evaluation of a malaria antibody enzyme immunoassay for use in blood screening. Inst. Oswaldo Cruz 2008, 103, 75–78, doi:10.1590/S0074-02762008005000008.
- Kakkilaya, B. Rapid Diagnosis of Malaria. Med. 2003, 34, 602–608, doi:10.1309/J4ANKCCJ147JB2FR.
- Abba, K.; Kirkham, A.J.; Olliaro, P.L.; Deeks, J.J.; Donegan, S.; Garner, P.; Takwoingi, Y. Rapid diagnostic tests for diagnosing uncomplicated non-falciparum or Plasmodium vivax malaria in endemic countries. Cochrane Database Syst. Rev. 2014, 12, doi:10.1002/14651858.CD011431.
- World Health Organization. Guidelines for the Treatment of Malaria, 3rd ed.; WHO: Geneva, Switzerland, 2015.
- World Health Organization. Malaria Rapid Diagnostic Test Performance, Results of WHO Product Testing of Malaria RDTs, Round 8 (2016–2018); WHO: Geneva, Switzerland, 2018.
- Ranadive, N.; Kunene, S.; Darteh, S.; Ntshalintshali, N.; Nhlabathi, N.; Dlamini, N.; Chitundu, S.; Saini, M.; Murphy, M.; Soble, A. Limitations of Rapid Diagnostic Testing in Patients with Suspected Malaria, A Diagnostic Accuracy Evaluation from Swaziland, a Low-Endemicity Country Aiming for Malaria Elimination. Infect. Dis. 2017, 64, 1221, doi:10.1093/CID/CIX131.
- Berhane, A.; Russom, M.; Bahta, I.; Hagos, F.; Ghirmai, M.; Uqubay, S. Rapid diagnostic tests failing to detect Plasmodium falciparum infections in Eritrea, an investigation of reported false negative RDT results. J. 2017, 16, 105, doi:10.1186/s12936-017-1752-9.
- Kozycki, C.T.; Umulisa, N.; Rulisa, S.; Mwikarago, E.I.; Musabyimana, J.P.; Habimana, J.P.; Karema, C.; Krogstad, D.J. False-negative malaria rapid diagnostic tests in Rwanda: Impact of Plasmodium falciparum isolates lacking hrp2 and declining malaria transmission. J. 2017, 16, 123, doi:10.1186/s12936-017-1768-1.
- World Health Organization. False-negative RDT results and implications of new reports of P. falciparum histidine-rich protein 2/3 gene deletions. WHO 2017, doi:10.1186/1475-2875-10-166.
- Murray, C.K.; Gasser, R.A.; Magill, A.J.; Miller, R.S. Update on Rapid Diagnostic Testing for Malaria. Microbiol. Rev. 2008, 21, 97–110, doi:10.1128/CMR.00035-07.
- Mathison, B.A.; Pritt, B.S. Update on Malaria Diagnostics and Test Utilization. Clin. Microbiol. 2017, 55, 2009–2017, doi:10.1128/JCM.02562-16.
- Rougemont, M.; Van Saanen, M.; Sahli, R.; Hinrikson, H.P.; Bille, J.; Jaton, K. Detection of Four Plasmodium Species in Blood from Humans by 18S rRNA Gene Subunit-Based and Species-Specific Real-Time PCR Assays. Clin. Microbiol. 2004, 42, 5636–5643, doi:10.1128/JCM.42.12.5636-5643.2004.
- Hsu, E. The history of qing hao in the Chinese materia medica. R. Soc. Trop. Med. Hyg. 2006, 100, 505–508, doi:10.1016/j.trstmh.2005.09.020.
- Achan, J.; O Talisuna, A.; Erhart, A.; Yeka, A.; Tibenderana, J.K.; Baliraine, F.N.; Rosenthal, P.J.; D’Alessandro, U. Quinine, an old anti-malarial drug in a modern world: Role in the treatment of malaria. J. 2011, 10, 144.
- Meshnick, S.R.; Dobson, M.J. The History of Antimalarial Drugs. In Antimalarial Chemotherapy, Mechanisms of Action, Resistance, and New Directions in Drug Discovery; Rosenthal, P., Ed.; Humana Press: Totowa NJ, USA, 2001; p. 396.
- World Health Organization. Antimalarial Drug Combination Therapy. Report of a WHO Technical Consultation; WHO: Geneva, Switzerland, 2001.
- Guo, Z. Artemisinin anti-malarial drugs in China. Acta Pharm. Sin. B 2016, 6, 115–124, doi:10.1016/j.apsb.2016.01.008.
- Ray, D. Organochlorine and Pyrethroid Insecticides. Toxicol. 2010, 13, 445–457, doi:10.1016/B978-0-08-046884-6.01327-0.
- Flannery, E.L.; Chatterjee, A.K.; Winzeler, E.A. Antimalarial drug discovery—Approaches and progress towards new medicines. Rev. Microbiol. 2013, 11, 849–862, doi:10.1038/nrmicro3138.
- Zhao, X.; Smith, D.L.; Tatem, A.J. Exploring the spatiotemporal drivers of malaria elimination in Europe. J. 2016, 15, 122, doi:10.1186/s12936-016-1175-z.
- Karunamoorthi, K. Malaria vaccine, a future hope to curtail the global malaria burden. J. Prev. Med. 2014, 5, 529–538.
- Moreno, A.; Joyner, C. Malaria vaccine clinical trials, what’s on the horizon. Opin. Immunol. 2015, 35, 98–106, doi:10.1016/j.coi.2015.06.008.
- Coelho, C.H.; Doritchamou, J.Y.A.; Zaidi, I.; Duffy, P.E. Advances in malaria vaccine development, report from the 2017 malaria vaccine symposium. NPJ Vaccines 2017, 2, 34, doi:10.1038/s41541-017-0035-3.
- Mahmoudi, S.; Keshavarz, H. Efficacy of phase 3 trial of RTS, S/AS01 malaria vaccine, The need for an alternative development plan. Vaccines Immunother. 2017, 13, 2098–2101, doi:10.1080/21645515.2017.1295906.
- Rénia, L.; Goh, Y.S.; Peng,. K, Mauduit, M.; Snounou, G. Assessing Malaria Vaccine Efficacy. In Towards Malaria Elimination: A Leap Forw; Manguin, S., Dev, V., Eds.; IntechOpen: London, UK, 2018; pp. 339–362, doi:10.5772/intechopen.77044.
- Draper, S.J.; Sack, B.K.; King, C.R.; Nielsen, C.M.; Rayner, J.C.; Higgins, M.K.; et al. Malaria Vaccines, Recent Advances and New Horizons. Cell Host Microbe 2018, 24, 43–56, doi:10.1016/j.chom.2018.06.008.
- Clinical Trials Register—Clinical Trials for Malaria 2019. Available online: https://www.clinicaltrialsregister.eu/ctr-search/search?query=Malaria (accessed on 30 April 2019).
- Crompton, P.D.; Pierce, S.K.; Miller, L.H. Advances and challenges in malaria vaccine development. Clin. Investig. 2010, 120, 4168–4178, doi:10.1172/JCI44423.
- Arama, C.; Troye-Blomberg, M. The path of malaria vaccine development, challenges and perspectives. Intern. Med. 2014, 275, 456–466, doi:10.1111/joim.12223.
- Kisalu, N.K.; Idris, A.H.; Weidle, C.; Flores-Garcia, Y.; Flynn, B.J.; Sack, B.K.; Murphy, S.; Schön, A.; Freire, E.; Francica, J.R.; et al. A human monoclonal antibody prevents malaria infection by targeting a new site of vulnerability on the parasite. Med. 2018, 24, 408–416, doi:10.1038/nm.4512.
- Claudia, F. Malaria vaccine–is it still required? Are vaccine alternatives enough to achieve malaria control? Asian Pac. J. Trop. Biomed. 2014, 4, S541–S544, doi:10.12980/APJTB.4.2014APJTB-2014-0181.
- Greenwood, B.; Targett, G. Malaria vaccines and the new malaria agenda. Microbiol. Infect. 2011, 17, 1600–1607, doi:10.1111/j.1469-0691.2011.03612.x.
- Hoffman, S.L.; Vekemans, J.; Richie, T.; Duffy, P. The March Toward Malaria Vaccines. J. Prev. Med. 2015, 49, S319–S333, doi:10.1016/j.amepre.2015.09.011.
- Shingadia, D. Treating malaria in the UK. Child Health 2014, 24, 232–235, doi:10.1016/j.paed.2013.10.003.
- Kremsner, P.G.; Krishna, S. Antimalarial combinations. Lancet 2004, 364, 285–294, doi:10.1016/S0140-6736(04)16680-4.
- Price, R.N.; Douglas NM. Artemisinin combination therapy for malaria, beyond good efficacy. Infect. Dis. 2009, 49, 1638–1640, doi:10.1086/647947.
- Nabudere, H.; Upunda, G.L.; Juma, M. Policy brief on improving access to artemisinin-based combination therapies for malaria in the East African community. J. Technol. Assess Health Care 2010, 26, 255–259, doi:10.1017/S026646231000019X.
- Sallares, R. Malaria and Rome: A History of Malaria in Ancient Italy; Oxford University Press: Oxford, UK, 2002; doi:10.1093/acprof,oso/9780199248506.001.0001.
- Micallef, M.J. The Roman fever, observations on the understanding of malaria in the ancient Roman world. J. Aust. 2016, 205, 501–503, doi:10.5694/mja16.00206.
- Jugoslavenski Leksikografski Zavod. Medical Encycolpedia; Jugoslavenski Leksikografski Zavod: Zagreb, Yugoslavia, 1969; p. 374.
- Trausmiller, O. Malarija i civilizacija. Priroda 1936, 3, 76–83.
- Odolin, S.; Gautret, P.; Parola, P. Epidemiology of imported malaria in the mediterranean region. J. Hematol. Infect. Dis. 2012, 4, e2012031.
- World Health Organization. Fact Sheet—History of Malaria Elimination in the European Region; WHO: Geneva, Switzerland, 2016.
- Mlinaric, D. Eco-historical area of the istrian borderland as a framework of the development of endemic diseases. Istar. Arh. 2010, 17, 155–177.
- Radosevic, M. Health conditions in the municipality of Medulin through history. In Municipality of Medulin Monograph; Bader, A., Ed.; Opcina Medulin: Medulin, Croatia, 2013; pp. 314–325.
- Rudetic, I. Malaria. In Istarska Enciklopedija; Bertosa, M., Matijasic, R., Eds.; Leksikografski Zavod Miroslav Krleza: Zagreb, Croatia, 2005; p. 544.
- Bakic, J. Seven centuries of the prevention of spreading of the infectious diseases into Croatia—Overview of the 60th anniversary of establishment of modern pest control in Croatia. Cas. Zavod Javno Zdr. 2011, 7, 1–17.
- Bakic, J. Trust worthy facts on first medically-entomological laboratory and introduction of Gambusia holbrooki into Croatia. Cas. Zavod Javno Zdr. 2006, 2, 20–25.
- Nezic, E. Ribica gambuzija u borbi protiv malarije. J. Fish. 1938, 1, 62–66.
- Mulic, R.; Aljinovic, L.; Gizdic, Z.; Petri, N.M. Malaria in Republic of Croatia, past, present and future. Vjesn. 2000, 122, 51–55.
- Fortis, A. Put Po Dalmaciji; Globus: Zagreb, Croatia, 1984.
- Wokaunn, M.; Juric, I.; Vrbica, Z. Between stigma and dawn of medicine, the last leprosarium in Croatia. Med. J. 2006, 47, 759–766.
- Tomasic, P. Malarija i blagostanje čovjeka. Priroda 1947, 4, 126–130.
- Skenderovic, R. Health Reforms Introduced by Maria Theresa in Provincial Slavonia and Generale Normativum Sanitatis of 1770. Slavon. 2005, 5, 115–143.
- Von Taube, F.W. Slavonija i Srijem 1777./1778; Drzavni Arhiv u Osijeku: Osijek, Croatia, 2012.
- Holzer, A. Asaniranje domacih predjela malarije. Liecnicki Viest. 1877, 4, 56–59.
- Majcen, V. The film funds of the school of national health (Andrija Stampar) at the Croatian film-library within the Croatian archive. Vjesn. 1987, 30, 71–88.
- Miletic-Medved, M.; Bozikov, J.; Uzarević, Z. Branko Cvjetanovic i Branimir Richter—Suradnici Andrije Stampara. Zavoda Za Znan. Umjetnicki Rad Osijeku 2012, 28, 103–113.
- Piperaki, E.T.; Daikos, G.L. Malaria in Europe, emerging threat or minor nuisance? Microbiol. Infect. 2016, 22, 487–493, doi:10.1016/J.CMI.2016.04.023.
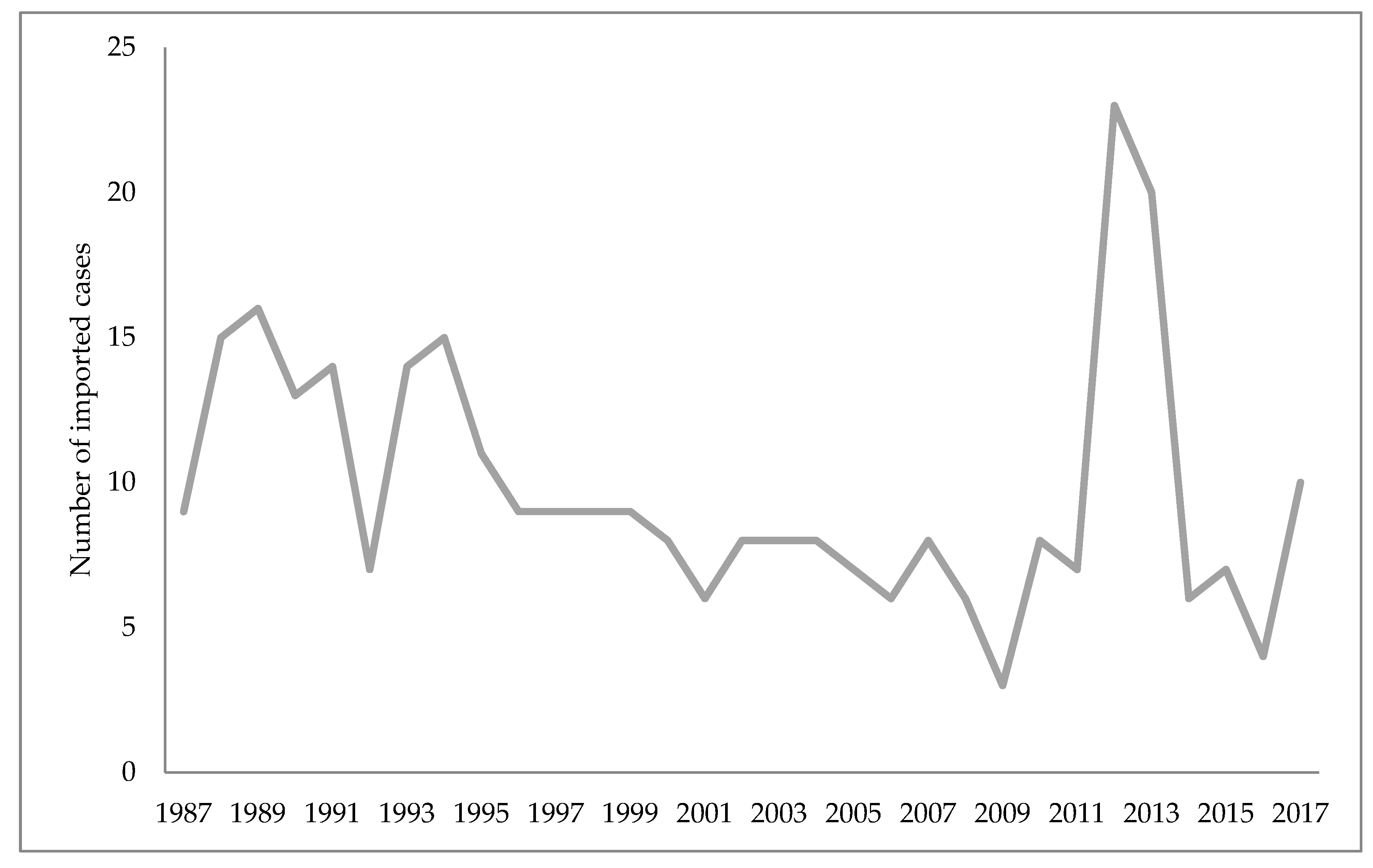
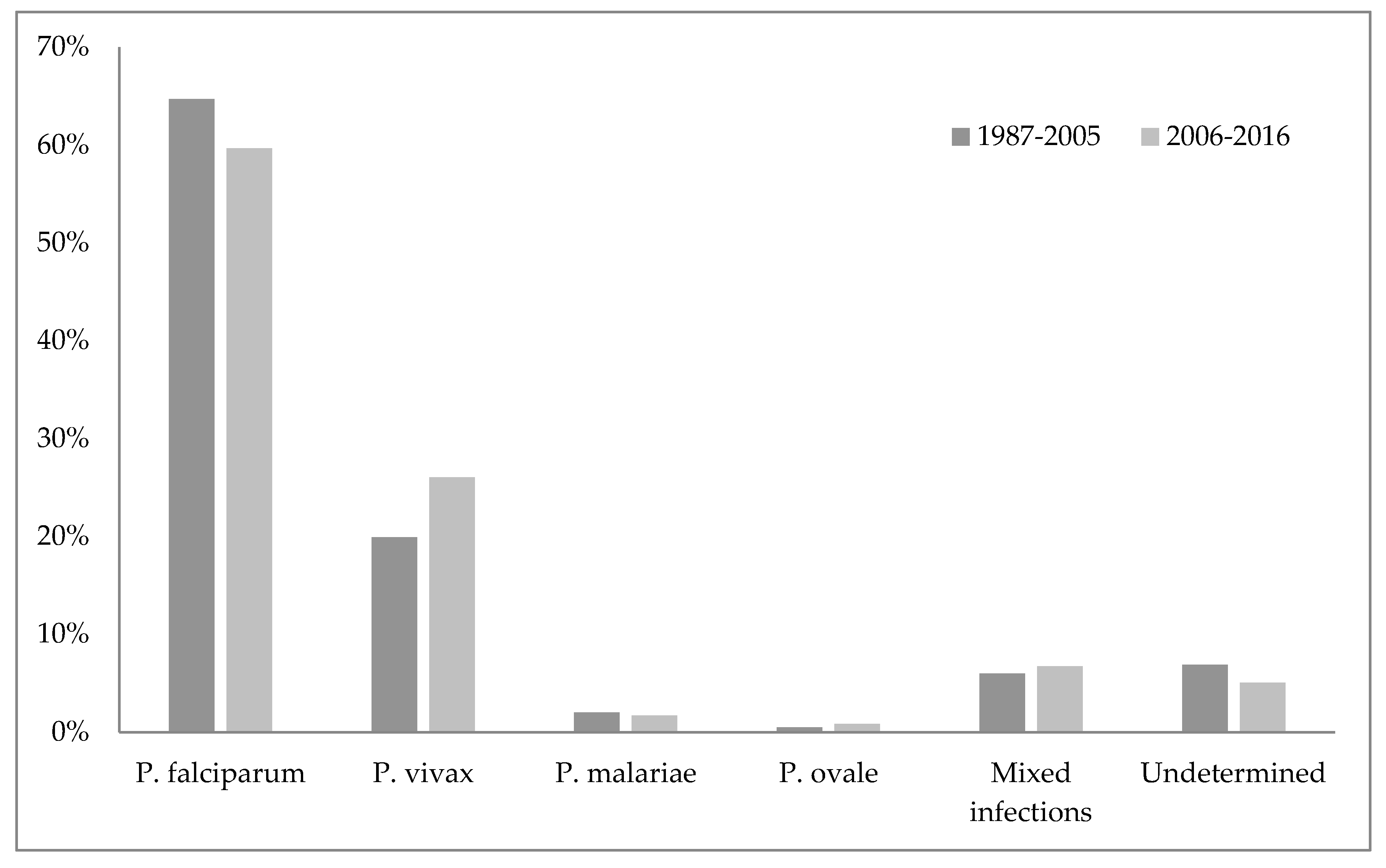
- Mulic, R. Malaria in Croatia, from eradication until today. J. 2012, 11, P135, doi:10.1186/1475-2875-11-S1-P135.
- Peric, D. Skrobonja, I.; Skrobonja, A.; Peric, D.; Skrobonja, I.; Skrobonja, A. Malaria in Croatia in the period between 1987 to 2006. Vjesn. 2009, 131, 192–195.
- Stevanovic, R.; Capak, K.; Brkic, K. Croatian Health Statistics Yearbook 2017; Croatian Institute of Public Health: Zagreb, Croatia, 2018.
- Talapko, J. Optimizacija metoda za uništavanje komaraca, ali i zaštite okoline. Vjesn. 1986, 2, 353–356.
- Tucak, A.; Dimitrijevic, M.; Gucunski, D.; Konstantinovic, B.; Miljus, B.; Grgic, Z.; Balog, Z.; Paulus, R.; Talapko, J. Multicentricni Program Istraživanja Ekologije Komaraca na Podrucju Sjeveroistocne Slavonije; Sveuciliste u Osijeku, Znanstvena Jedinica za Klinicko-Medicinska Istraživanja Opce bolnice Osijek: Osijek, Croatia, 1985.
- World Health Organization. World Malaria Report 2010; WHO: Geneva, Croatia, 2010.
- Patouillard, E.; Griffin, J.; Bhatt, S.; Ghani, A.; Cibulskis, R. Global investment targets for malaria control and elimination between 2016 and 2030. BMJ Glob. Health 2017, 2, e000176, doi:10.1136/bmjgh-2016-000176.
- World Health Organization. Global Report on Insecticide Resistance in Malaria Vectors, 2010–2016; WHO: Geneva, Croatia, 2018.
- Alonso, P.; Noor, A,M. The global fight against malaria is at crossroads. Lancet 2017, 390, 2532–2534, doi:10.1016/S0140-6736(17)33080-5.
