Vertebral lumbar surgery can be performed under both general anesthesia (GA) and spinal anesthesia. A clear benefit from spinal anesthesia (SA) remains unproven.
- general anesthesia
- spinal anesthesia
1. Introduction
Vertebral lumbar surgery can be performed under both general anesthesia (GA) and spinal anesthesia (SA). Each has possible advantages and complications in the perioperative period [1]. In particular, SA does not require airway device placement for intraoperative sedation and analgesia; however, it could be associated with patient discomfort and intraoperative patient movements [2]. Moreover, fear of neuraxial damage caused by either local anesthetic toxicity or direct damage with an associated prolonged hospital length of stay (LOS) may discourage its use [3].
According to a systematic review and meta-analysis published in 2016 [4], patients undergoing lumbar spine surgery under SA required less analgesia in post-anesthesia care units and had less nausea and vomiting (PONV) in the first postoperative day, but no difference in intraoperative hypotension, bradycardia, blood loss, and surgical time was reported.
Given the above, a clear benefit from SA during lumbar spine surgery remains unproven. Furthermore, relevant clinical outcomes remain unexplored.
2. Study Selection and Data Retrieval
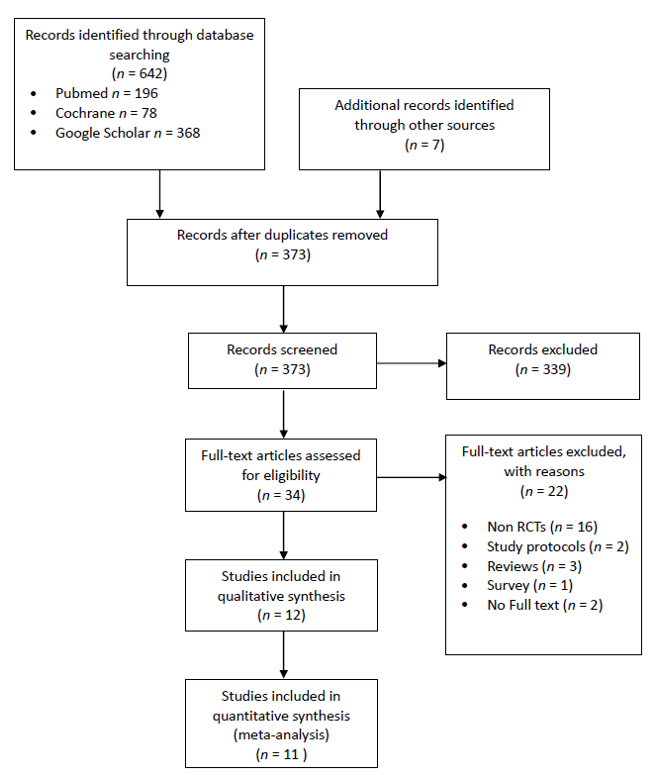
Bibliographic search results are shown in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram (Figure 1). Notably, three RCTs did not report quantitative data. Two papers were excluded because, despite our best efforts, we were not able to retrieve the full text [11,12], in one case [13] the paper did not contain any variable of interest and the authors were not able to provide any missing information.
Figure 1. The PRISMA flowchart.
Eleven studies counting a total of 896 patients entered the quantitative and qualitative analysis [14–24]. All controversies were solved by discussion and the third reviewer was not required.
We asked all the corresponding authors for missing data, and five of them replied to our query. Only two of them, nevertheless, provided part of the missing data required [16–24].
Additional records were identified by checking the reference lists of included studies.
3. Study Characteristics
Among the 896 patients, half (449; 50.12%) underwent GA, while the remainder underwent SA (447; 49.88%). The characteristics of included studies are shown in Table 1 and Table S2.
Table 1. Study characteristics.
|
Study |
N (% F) |
Inclusion Criteria |
Protocols |
Surgery |
Time to Pain Assessment |
||||
|
Age |
ASA-PS |
BMI (Kg/m2) |
SA |
GA |
PO Therapy |
||||
|
Attari (2011) [14] |
72 (46%) |
18–60 |
I–II |
NR |
3.0–3.2 mL Hyperbaric Bupivacaine 0.5% + 25 mcg Fentanyl |
- Induction: propofol, lidocaine, fentanyl, atracurium - Maintenance: isoflurane 1,2%, N20 50% |
Pethidine 0.4 mg/kg on VAS (rescue pethidine 0.2 mg/kg). |
Laminectomy, Discectomy |
NR |
|
Baenziger (2020) [22] |
100 (46%) |
Adult |
I–III |
NR |
3.0–4.0 mL Hyperbaric Bupivacaine 0.5% + 25 mcg Fentanyl |
- Induction: propofol, fentanyl, atracurium - Maintenance: Propofol TCI, Remifentanil TCI |
NR |
Laminectomy, Discectomy |
3 h |
|
Chowdhury (2010) [15] |
80 (38%) |
Adult |
I–II |
NR |
2.5–2.8 mL Hyperbaric Bupivacaine 0.5% + 12.5 mcg Fentanyl |
- Induction: propofol, fentanyl, rocuronium - Maintenance: halothane 0.8%, N20 60% |
Pethedine 2 mg/kg six hourly and on request. |
Discectomy |
6 h |
|
Hussain (2015) [16] |
60 (50%) |
20–50 |
I–II |
NR |
2 mL Bupivacaine 0.75% |
- Induction: propofol, atracurium - Maintenance: sevoflurane 1.5–2%, nalbuphine |
NR |
Micro- discectomy |
Peak at 6 h |
|
Jellish (1996) [17] |
122 (46%) |
Adult |
I–III |
NR |
1.5 mL Hyperbaric Bupivacaine 0.75% |
- Induction: thiopental, fentanyl, vecuronium - Maintenance: isoflurane, N2O 70% |
PACU: morphine 2 mg IV ward:meperidine 25–50 mg IV or 50–100 mg intramuscularly. |
Laminectomy, Discectomy |
Peak |
|
Kahveci (2014) [18] |
80 (38%) |
≥18 |
I–II |
≤25 |
3 mL Hyperbaric Bupivacaine 0.5% |
- Induction: propofol, fentanyl, atracurium - Maintenance: sevoflurane 1.5–2%, atracurium |
Pethedine 25 mg IV on VAS. |
Single-level spinal surgery |
NR |
|
Kara (2011) [21] |
60 (45%) |
Adult |
I–II |
NR |
2 mL Levobupivacaine 0.5% |
- Induction: propofol, fentanyl, rocuronium - Maintenance: desflurane 6%, N2O 40–60% |
Morphine 2 mg on VAS. |
Discectomy |
Peak |
|
Kilic (2019) [23] |
111 (45%) |
18–65 |
I–III |
NR |
3 mL Hyperbaric Bupivacaine 0.5% |
- Induction: propofol, fentanyl, rocuronium - Maintenance: sevoflurane 1.5–2%, remifentanil |
NR |
Micro- discectomy |
3 h |
|
Sadrolsadat (2009) [19] |
100 (-) |
Adult |
I–III |
NR |
4 mL Bupivacaine 0.5% |
- Induction: propofol, fentanyl, atracurium - Maintenance: propofol, alfentanil, atracurium |
Pethedine 25 mg IV on VAS (lock 30 min in PACU and 4 h in ward). |
Laminectomy |
NR |
|
Vural (2014) [20] |
66 (-) |
23–74 |
ND |
NR |
4 mL Hyperbaric Bupivacaine 0.5% |
- Induction: thiopental, fentanyl, rocuronium - Maintenance: desflurane 5–6%, N2O 40–60%,fentanyl |
NR |
Disc herniation surgery |
6 h |
|
Yildirim Güçlü (2014) [24] |
56 (-) |
18–60 |
I–II |
≤35 |
3 mL Hyperbaric Bupivacaine 0.5% |
- Induction: thiopental, fentanyl, vecuronium - Maintenance: desflurane 4–5%, N2O 50%, remifentanil |
Pethidine 0.5 mg/kg on VAS (Rescue pethidine 0.2 mg/kg). |
Micro- discectomy |
NR |
ASA-PS: ASA Physical Status, F: females, GA: General Anesthesia, SA: Spinal Anesthesia, PACU: Post-Anesthesia Care Unit, PO: Post-Operative, NR: Not Reported.
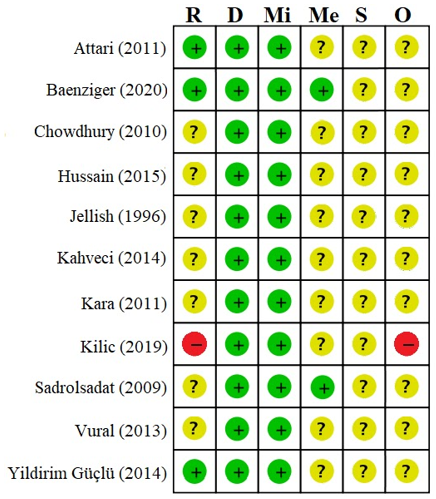
There were concerns of bias in ten studies, where one study was evaluated at high risk of bias [23] (Figure 2). Details on risk of bias assessment are available as Table S3.
Figure 2. Summary of bias evaluated by the Risk of Bias 2 Tool. R: Bias arising from the randomization process, D: Bias due to deviations from intended interventions, Mi: Bias due to missing outcome data, Me: Bias in measurement of the outcome, S: Bias in the selection of the reported result, and O: Overall risk of bias. Green “+”: Low risk of bias, Yellow “?”: Some concerns, Red “-”: High risk of bias.
References
- Parker, M.J.; Unwin, S.C.; Handoll, H.H.; Griffiths, R. General versus spinal/epidural anaesthesia for surgery for hip fractures in adults. Cochrane Database Syst. Rev. 2000, 4, CD000521.
- Mergeay, M.; Verster, A.; Van Aken, D.; Vercauteren, M. Regional versus general anesthesia for spine surgery. A comprehensive review. Acta Anaesthesiol. Belg. 2015, 66, 1–9.
- Zorrilla-Vaca, A.; Healy, R.J.; Mirski, M.A. A Comparison of Regional versus General Anesthesia for Lumbar Spine Surgery: A Meta-Analysis of Randomized Studies. Neurosurg. Anesthesiol. 2017, 29, 415–425.
- Meng, T.; Zhong, Z.; Meng, L. Impact of spinal anaesthesia vs. general anaesthesia on peri-operative outcome in lumbar spine surgery: A systematic review and meta-analysis of randomised, controlled trials. Anaesthesia 2017, 72, 391–401.
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700.
- De Cassai, A. Comparison of Spinal Anesthesia and General Anesthesia for Spine Surgery: A Meta-analysis of Randomized Controlled Trials. OSF 2020, doi:10.17605/OSF.IO/KXP3C.
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898.
- Schünemann, H.J.; Vist, G.E.; Higgins, J.P.T.; Santesso, N.; Deeks, J.J.; Glasziou, P.; Guyatt, G.H. Interpreting results and drawing conclusions. In Cochrane Handbook for Systematic Reviews of Interventions; Higgins, J.; Thomas,; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V.; Cochrane: London, UK, 2020, Available online: https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions (accessed on 1 December 2020)
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560.
- Wetterslev, J.; Jakobsen, J.C.; Gluud C. Trial Sequential Analysis in systematic reviews with meta-analysis. BMC Med. Res. Methodol. 2017, 17, 39.
- Dagher, C.; Naccache, N.; Narchi, P.; Hage, P.;Antakly, M.C. Regional anesthesia for lumbar microdiscectomy. J. Liban. 2002, 50, 206–210.
- Khan, M.W.; Ibrahim, N.O.; Iqbal, M.; Khan, A.A.; Abbasi, S.M. A prospective randomized trial comparing the spinal and general anesthesia in lumbar disc surgery: A study of 44 cases. Forum. Mon. 2012, 23, 61–64.
- Pınar, H.U.; Kaşdoğan, Z.E.A.; Başaran, B.; Çöven, İ.; Karaca, Ö.; Doğan, R. The effect of spinal versus general anesthesia on intraocular pressure in lumbar disc surgery in the prone position: A randomized, controlled clinical trial. Clin. Anesth. 2018, 46, 54–58.
- Attari, M.A.; Mirhosseini, S.A.; Honarmand, A.; Safavi, M.R. Spinal anesthesia versus general anesthesia for elective lumbar spine surgery: A randomized clinical trial. Res. Med. Sci. 2011, 16, 524–529.
This entry is adapted from the peer-reviewed paper 10.3390/jcm10010102