People increasingly seek dental treatment to improve their smile's aesthetics. A common concern is a hyperpigmented gingiva and high frenum attachment. Gingival recession can result from high frenum attachment, either by interfering with the toothbrush's correct positioning or by causing a muscular pull through the opening of gingival crevice. We present a case of a young patient concerned with the presence of hyperpigmented gingiva. On intraoral examination high frenal attachment was also observed. After providing the patient all the available treatment options and their advantages and disadvantages respectively, patient decided to opt for conventional surgical scalpel method for depigmentation as well as frenectomy. Patient was recalled for periodontal dressing removal after 1 week and follow up was performed at 6 months.
- aesthetics
- hyperpigmented gingiva
- high frenum attachment
- conventional surgical scalpel method
- periodontal dressing.
1. Introduction
A female patient of 21 years age reported to the Department of Periodontology, with the chief complaint of concern about dark gums. On intraoral examination high frenal attachment was also observed. Her medical history suggested that she may have physiological melanin pigmentation because this problem has existed since his childhood. Melanin hyperpigmentation was found on both maxillary and mandibular labial gingiva (Figure 1). The patient had no systemic illness and had no harmful habits like smoking or tobacco chewing and maintained good oral hygiene. The patient was explained about all the treatment choices available, including the use of diodes, lasers, electrocautery, and the traditional scalpel procedure, along with their benefits and drawbacks. The possibility of re-pigmentation over time was also addressed.

Patient found it comfortable to proceed with conventional method of scalpel surgical technique for gingival depigmentation.
On the first visit phase I therapy was conducted, which included scaling, polishing and oral hygiene instructions.
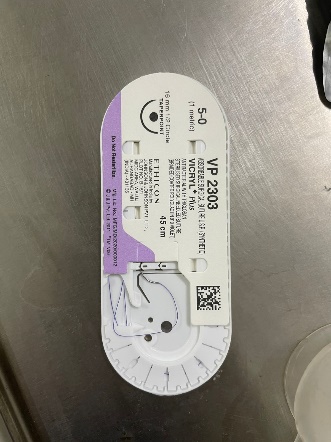
Under all aseptic conditions and precautions and under local anesthesia, the whole pigmented layer of the gingival epithelium and some of the underlying connective tissue was removed (Figure 2). Sterile gauze was employed to manage the bleeding. A hemostat was used to engage the frenum. It was entered into the vestibule's depth, and incisions were made on both its upper and lower surfaces until it was free (Figure 3). The frenum's triangularly resected haemostat section was taken out. To release the fibrous attachment, the bone was bluntly dissected. The area was sutured with the help of 5-0 vicryl absorbable synthetic sutures (Figure 4,5) and the depigmented area was covered with a periodontal dressing (Figure 6). Post-operative care included analgesics and an antiseptic mouthwash. Dressing was removed after a week.




Follow up was done after 6 months to check for any repigmentation (Figure7,8)


The mandibular gingival area was not depigmented because the patient did not find it to be an aesthetic concern.
2. Learning Points
-The gingiva is the most prevalent location of mucosal pigmentation, and the most frequent biologic pigment is melanin which is responsible for intrinsic discoloration of the gums [1].
-Gingivectomy, mucosal excision using a scalp, abrasion procedures, free gingival grafts, chemical methods utilizing caustic chemicals, electrosurgery, cryotherapy, and the use of newly created lasers are some of the treatment modalities that have been employed to obtain pigmentation-free gingiva [2].
-While surgical scalpel method method promotes faster wound healing, it tends to be more painful. Since secondary intentional healing takes place for the exposed tissues, a periodontal dressing is required to decrease bleeding, ache, and the risk of surgical site infection [3].
-Careful attention is needed to safeguard the marginal gingiva during this procedure, as improper use can cause gingival recession and damage to the periosteum and bone [4].
-Absorbable sutures when used resulted in a remarkable reduced risk of infection in contrast to the conventional non-absorbable sutures [5].
3. Conclusion
A person's increasing desire for aesthetics necessitates the removal of high frenal attachment and hyperpigmented gingival areas in order to produce a confident and attractive smile, which can be accomplished with ease utilizing the surgical scalpel procedure. Absorbable sutures are a safe option for treating traumatic wound lacerations in terms of infection rates and wound healing. They also reduce postoperative hospital visits because they are not intended to be removed. Additionally, by preventing unforeseen outcomes from non-removal or self-removal of non-absorbable sutures, the use of absorbable sutures may promote wound healing.
References
- Disorders of Oral Pigmentation: Background, Pathophysiology, Etiology. 2021 Nov 8 [cited 2024 Nov 10]; Available from: https://emedicine.medscape.com/article/1078143-overview?form=fpf
- Patil KP, Joshi V, Waghmode V, Kanakdande V. Gingival depigmentation: A split mouth comparative study between scalpel and cryosurgery. Contemp Clin Dent. 2015 Mar;6(Suppl 1):S97–101.
- Grover HS, Dadlani H, Bhardwaj A, Yadav A, Lal S. Evaluation of patient response and recurrence of pigmentation following gingival depigmentation using laser and scalpel technique: A clinical study. J Indian Soc Periodontol. 2014 Sep;18(5):586–92.
- Roshna T, Nandakumar K. Anterior esthetic gingival depigmentation and crown lengthening: report of a case. J Contemp Dent Pract. 2005 Aug 15;6(3):139–47.
- Parell GJ, Becker GD. Comparison of Absorbable With Nonabsorbable Sutures in Closure of Facial Skin Wounds. Arch Facial Plast Surg. 2003 Nov 1;5(6):488–90.
