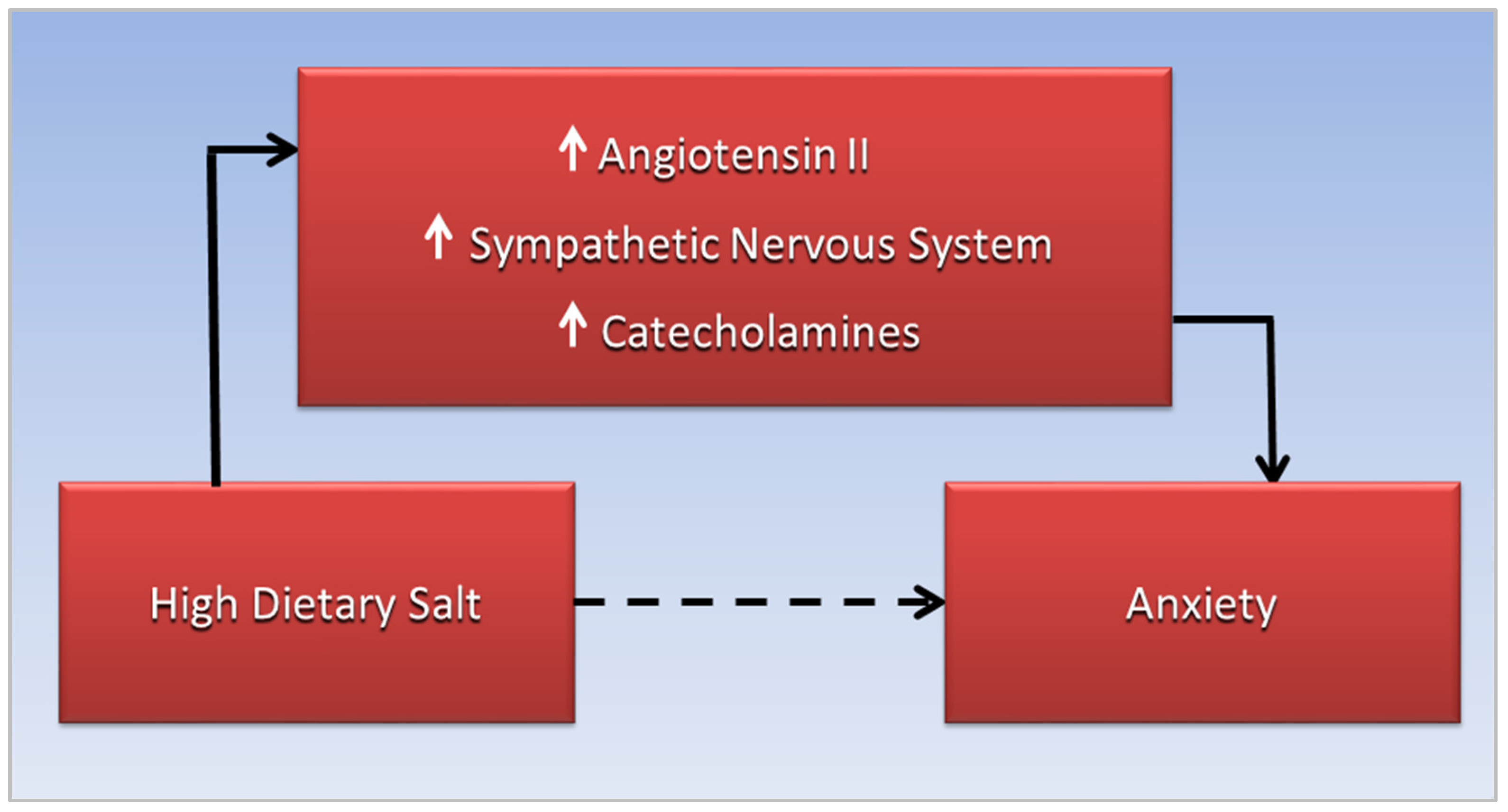
Increased anxiety in these conditions may be linked to a high-salt diet through stimulation of the sympathetic nervous system, which increases blood pressure while releasing catecholamines, causing a “fight or flight” response. A rostral shift of fluid overload from the lower to the upper body occurs in obstructive sleep apnea associated with COVID-19 and cardiovascular disease, and may be related to sodium and fluid retention triggered by hypertonic dehydration. Chronic activation of the renin-angiotensin-aldosterone system responds to salt-induced dehydration by increasing reabsorption of sodium and fluid, potentially exacerbating fluid overload. Anxiety may also be related to angiotensin II that stimulates the sympathetic nervous system to release catecholamines.
- hypertension
- anxiety
- obstructive sleep apnea
- cardiovascular disease
- COVID-19
- dietary salt
- renin-angiotensin-aldosterone system
- sympathetic nervous system
- catecholamines
1. Introduction
2. Anxiety, CVD, and Sodium Toxicity
3. OSA, Hypertension, and the Renin-Angiotensin-Aldosterone System
4. OSA, Anxiety, and Angiotensin II
This entry is adapted from the peer-reviewed paper 10.3390/diseases10040089
References
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2020, 75, 285–292.
- Wu, C.Y.; Hu, H.Y.; Chou, Y.J.; Huang, N.; Chou, Y.C.; Li, C.P. High Blood Pressure and All-Cause and Cardiovascular Disease Mortalities in Community-Dwelling Older Adults. Medicine 2015, 94, e2160.
- Hall, J.E.; Guyton, A.C.; Coleman, T.G.; Mizelle, H.L.; Woods, L.L. Regulation of arterial pressure: Role of pressure natriuresis and diuresis. Fed. Proc. 1986, 45, 2897–2903.
- Who.Int. Salt Reduction. Available online: https://www.who.int/news-room/fact-sheets/detail/salt-reduction (accessed on 30 August 2022).
- Choi, H.Y.; Park, H.C.; Ha, S.K. Salt Sensitivity and Hypertension: A Paradigm Shift from Kidney Malfunction to Vascular Endothelial Dysfunction. Electrolytes Blood Press. 2015, 13, 7–16.
- Grillo, A.; Salvi, L.; Coruzzi, P.; Salvi, P.; Parati, G. Sodium intake and hypertension. Nutrients 2019, 11, 1970.
- Rust, P.; Ekmekcioglu, C. Impact of Salt Intake on the Pathogenesis and Treatment of Hypertension. In Hypertension: From Basic Research to Clinical Practice; Islam, M.S., Ed.; Springer International Publishing: Cham, Switzerland, 2017; pp. 61–84.
- Luzardo, L.; Noboa, O.; Boggia, J. Mechanisms of Salt-Sensitive Hypertension. Curr. Hypertens. Rev. 2015, 11, 14–21.
- Janszky, I.; Ahnve, S.; Lundberg, I.; Hemmingsson, T. Early-Onset Depression, Anxiety, and Risk of Subsequent Coronary Heart Disease: 37-Year Follow-Up of 49,321 Young Swedish Men. J. Am. Coll. Cardiol. 2010, 56, 31–37.
- Roest, A.M.; Martens, E.J.; de Jonge, P.; Denollet, J. Anxiety and risk of incident coronary heart disease: A meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 38–46.
- Batelaan, N.M.; Seldenrijk, A.; Bot, M.; van Balkom, A.J.; Penninx, B.W. Anxiety and new onset of cardiovascular disease: Critical review and meta-analysis. Br. J. Psychiatry 2016, 208, 223–231.
- Reiner, I.C.; Tibubos, A.N.; Werner, A.M.; Ernst, M.; Brähler, E.; Wiltink, J.; Michal, M.; Schulz, A.; Wild, P.S.; Münzel, T.; et al. The association of chronic anxiousness with cardiovascular disease and mortality in the community: Results from the Gutenberg Health Study. Sci. Rep. 2020, 10, 12436.
- Dimsdale, J.E. What does heart disease have to do with anxiety? J. Am. Coll. Cardiol. 2010, 56, 47–48.
- Goddard, A.W.; Ball, S.G.; Martinez, J.; Robinson, M.J.; Yang, C.R.; Russell, J.M.; Shekhar, A. Current perspectives of the roles of the central norepinephrine system in anxiety and depression. Depress. Anxiety 2010, 27, 339–350.
- Ralph, A.F.; Grenier, C.; Costello, H.M.; Stewart, K.; Ivy, J.R.; Dhaun, N.; Bailey, M.A. Activation of the Sympathetic Nervous System Promotes Blood Pressure Salt-Sensitivity in C57BL6/J Mice. Hypertension 2021, 77, 158–168.
- Pan, Y.; Cai, W.; Cheng, Q.; Dong, W.; An, T.; Yan, J. Association between anxiety and hypertension: A systematic review and meta-analysis of epidemiological studies. Neuropsychiatr. Dis. Treat. 2015, 11, 1121–1130.
- Peskind, E.R.; Radant, A.; Dobie, D.J.; Hughes, J.; Wilkinson, C.W.; Sikkema, C.; Veith, R.C.; Dorsa, D.M.; Raskind, M.A. Hypertonic saline infusion increases plasma norepinephrine concentrations in normal men. Psychoneuroendocrinology 1993, 18, 103–113.
- Molosh, A.I.; Johnson, P.L.; Fitz, S.D.; Dimicco, J.A.; Herman, J.P.; Shekhar, A. Changes in central sodium and not osmolarity or lactate induce panic-like responses in a model of panic disorder. Neuropsychopharmacology 2010, 35, 1333–1347.
- Arnold, E. Anxiety DSM-5 Diagnostic Criteria and Treatment Overview. Available online: https://pro.psycom.net/assessment-diagnosis-adherence/anxiety (accessed on 30 August 2022).
- Yi, B.; Titze, J.; Rykova, M.; Feuerecker, M.; Vassilieva, G.; Nichiporuk, I.; Schelling, G.; Morukov, B.; Choukèr, A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: A longitudinal study. Transl. Res. 2015, 166, 103–110.
- da Silva, B.C.; Kasai, T.; Coelho, F.M.; Zatz, R.; Elias, R.M. Fluid Redistribution in Sleep Apnea: Therapeutic Implications in Edematous States. Front. Med. 2017, 4, 256.
- Bangash, A.; Wajid, F.; Poolacherla, R.; Mim, F.K.; Rutkofsky, I.H. Obstructive Sleep Apnea and Hypertension: A Review of the Relationship and Pathogenic Association. Cureus 2020, 12, e8241.
- Dominguez, A.; Muppidi, V.; Gupta, S. Hyperaldosteronism. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499983/ (accessed on 1 October 2022).
- Coble, J.P.; Grobe, J.L.; Johnson, A.K.; Sigmund, C.D. Mechanisms of brain renin angiotensin system-induced drinking and blood pressure: Importance of the subfornical organ. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 308, R238–R249.
- Tiarks, G. Hypertonic dehydration: What Is It, Causes, Treatment, and More. Available online: https://www.osmosis.org/answers/hypertonic-dehydration (accessed on 1 September 2022).
- Ames, M.K.; Atkins, C.E.; Pitt, B. The renin-angiotensin-aldosterone system and its suppression. J. Vet. Intern. Med. 2019, 33, 363–382.
- Augustine, R.; Abhilash, S.; Nayeem, A.; Salam, S.A.; Augustine, P.; Dan, P.; Maureira, P.; Mraiche, F.; Gentile, C.; Hansbro, P.M.; et al. Increased complications of COVID-19 in people with cardiovascular disease: Role of the renin–angiotensin-aldosterone system (RAAS) dysregulation. Chem. Biol. Interact. 2022, 351, 109738.
- Dudenbostel, T.; Calhoun, D.A. Resistant hypertension, obstructive sleep apnoea and aldosterone. J. Hum. Hypertens. 2012, 26, 281–287.
- Fereidoun, H.; Pouria, H. Effect of excessive salt consumption on night’s sleep. Pak J. physiol. 2014, 10, 6–9.
- Pimenta, E.; Stowasser, M.; Gordon, R.D.; Harding, S.M.; Batlouni, M.; Zhang, B.; Oparil, S.; Calhoun, D.A. Increased dietary sodium is related to severity of obstructive sleep apnea in patients with resistant hypertension and hyperaldosteronism. Chest 2013, 143, 978–983.
- Fiori, C.Z.; Martinez, D.; Montanari, C.C.; Lopez, P.; Camargo, R.; Sezerá, L.; Gonçalves, S.C.; Fuchs, F.D. Diuretic or sodium-restricted diet for obstructive sleep apnea—A randomized trial. Sleep 2018, 41, zsy016.
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review the Dietary Reference Intakes for Sodium and Potassium. The National Academies Collection: Reports funded by National Institutes of Health. In Dietary Reference Intakes for Sodium and Potassium; Oria, M., Harrison, M., Stallings, V.A., Eds.; National Academies Press (US): Washington, DC, USA, 2019.
- NHLBI. Implementing Recommendations for Dietary Salt Reduction: Where Are We? Where Are We Going? How Do We Get There?: A Summary of an NHLBI Workshop; National Institutes of Health, National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 1996.
- Kasai, T.; Arcand, J.; Allard, J.P.; Mak, S.; Azevedo, E.R.; Newton, G.E.; Bradley, T.D. Relationship between sodium intake and sleep apnea in patients with heart failure. J. Am. Coll. Cardiol. 2011, 58, 1970–1974.
- Kim, J.Y.; Ko, I.; Kim, D.K. Association of Obstructive Sleep Apnea With the Risk of Affective Disorders. JAMA Otolaryngol. –Head Neck Surg. 2019, 145, 1020–1026.
- Rezaeitalab, F.; Moharrari, F.; Saberi, S.; Asadpour, H.; Rezaeetalab, F. The correlation of anxiety and depression with obstructive sleep apnea syndrome. J. Res. Med. Sci. 2014, 19, 205–210.
- Cox, R.C.; Olatunji, B.O. Sleep in the anxiety-related disorders: A meta-analysis of subjective and objective research. Sleep Med. Rev. 2020, 51, 101282.
- Akberzie, W.; Hesselbacher, S.; Aiyer, I.; Surani, S.; Surani, Z.S. The Prevalence of Anxiety and Depression Symptoms in Obstructive Sleep Apnea. Cureus 2020, 12, e11203.
- Duan, X.; Zheng, M.; Zhao, W.; Huang, J.; Lao, L.; Li, H.; Lu, J.; Chen, W.; Liu, X.; Deng, H. Associations of Depression, Anxiety, and Life Events With the Risk of Obstructive Sleep Apnea Evaluated by Berlin Questionnaire. Front. Med. 2022, 9, 799792.
- Daabis, R.; Gharraf, H. Predictors of anxiety and depression in patients with obstructive sleep apnea. Egypt. J. Chest Dis. Tuberc. 2012, 61, 171–177.
- Garbarino, S.; Bardwell, W.A.; Guglielmi, O.; Chiorri, C.; Bonanni, E.; Magnavita, N. Association of Anxiety and Depression in Obstructive Sleep Apnea Patients: A Systematic Review and Meta-Analysis. Behav. Sleep Med. 2020, 18, 35–57.
- Batzikosta, A.; Antoniadou, M.; Tiga, P.; Nena, E.; Xanthoudaki, M.; Voulgaris, A.; Sotiropoulou, R.; Kouratzi, M.; Froudarakis, M.; Steiropoulos, P. AB011. Assessment of anxiety and depressive symptoms in obstructive sleep apnea patients. Ann. Transl. Med. 2016, 4, 11.
- Wong, J.L.; Martinez, F.; Aguila, A.P.; Pal, A.; Aysola, R.S.; Henderson, L.A.; Macey, P.M. Stress in obstructive sleep apnea. Sci. Rep. 2021, 11, 12631.
- Sharafkhaneh, A.; Giray, N.; Richardson, P.; Young, T.; Hirshkowitz, M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 2005, 28, 1405–1411.
- Mansukhani, M.P.; Kara, T.; Caples, S.M.; Somers, V.K. Chemoreflexes, sleep apnea, and sympathetic dysregulation. Curr. Hypertens. Rep. 2014, 16, 476.
- Benigni, A.; Cassis, P.; Remuzzi, G. Angiotensin II revisited: New roles in inflammation, immunology and aging. EMBO Mol. Med. 2010, 2, 247–257.
- Wang, Y.; Seto, S.W.; Golledge, J. Angiotensin II, sympathetic nerve activity and chronic heart failure. Heart Fail. Rev. 2014, 19, 187–198.
- Dendorfer, A.; Thornagel, A.; Raasch, W.; Grisk, O.; Tempel, K.; Dominiak, P. Angiotensin II induces catecholamine release by direct ganglionic excitation. Hypertension 2002, 40, 348–354.
- Hakim, F.; Gozal, D.; Kheirandish-Gozal, L. Sympathetic and catecholaminergic alterations in sleep apnea with particular emphasis on children. Front. Neurol. 2012, 3, 7.
- Sica, E.; De Bernardi, F.; Nosetti, L.; Martini, S.; Cosentino, M.; Castelnuovo, P.; Marino, F. Catecholamines and children obstructive sleep apnea: A systematic review. Sleep Med. 2021, 87, 227–232.
