Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Cardiac arrest occurs as a result of a sudden stop of the heartbeat and its mechanical activity, which causes cessation of systemic circulation and blood flow in the brain, which triggers global brain ischemia. Brain neuropathology after cardiac arrest includes primary ischemic injury and secondary reperfusion injury, which occur sequentially, acutely during cardiac arrest and resuscitation, and chronically in the post-resuscitation stag.
- cardiac arrest
- cerebral ischemia
- reperfusion
1. Cardiac Arrest
Cardiac arrest occurs as a result of a sudden stop of the heartbeat and its mechanical activity, which causes cessation of systemic circulation and blood flow in the brain, which triggers global brain ischemia [1][2]. A comprehensive analysis of studies conducted in Europe, China, and the USA showed that the average age of patients who suffered cardiac arrest was 60–66 years, and 58–81% of them were men [3][4][5]. However, rates of mortality, depression, anxiety, and cognitive impairment were higher in women than in men [6][7]. The incidence of cardiac arrest worldwide exceeds 3.7 million annually [8][9]. Among others, in Europe there are 275,000, in the USA 450,000, in Taiwan 10,000, of whom about 10–15% survive until discharge from hospital [10][11][12][13]. The annual incidence of in-hospital cardiac arrest is estimated at 35–55 per 100,000 in Europe and the USA and 28–43 per 100,000 in Asia [9][14][15][16]. In Europe, based on data from the EuReCa ONE and EuReCa TWO studies, the annual incidence of out-of-hospital cardiac arrest was estimated at 84 per 100,000 patients and 89 per 100,000 patients, respectively [17][18], with a moderate average survival rate of 8% [18][19]. In European countries, it is estimated that 56–62 people per 100,000 are treated by emergency services for out-of-hospital cardiac arrest each year [15][18]. In Latin America and Colombia, the epidemiological characteristics and treatment outcomes of patients with out-of-hospital cardiac arrest are similar to those described in the world literature [20]. Similar statistics apply to the United States, Australia, and New Zealand [21][22]. Generally, the return of spontaneous circulation after cardiac arrest ranges from 33.7 to 35.5% [5][23]. Male gender and advanced age have been shown to be independent factors for failure to return spontaneous circulation after cardiac arrest [3][4][5].
Patients who are successfully resuscitated suffer from cerebral hypoxia and ischemia, which is the main cause of side-effects and death after admission to the intensive care unit [24]. Brain damage after cardiac arrest is the leading cause of death in patients resuscitated after cardiac arrest and the leading cause of long-term disability in those who survive the acute phase [25][26]. Therefore, cardiopulmonary resuscitation is the most important therapeutic activity that restores life to patients after cardiac arrest [1][2]. Despite progress in the use of cardiopulmonary resuscitation and targeted brain temperature control by lowering the head temperature to 32–34 °C [12][27][28][29], only 10–15% of patients after cardiac arrest survive until discharge from the hospital [12][13]. Therefore, cardiac arrest and cardiopulmonary resuscitation constitute a serious challenge for emergency physicians around the world and their actions are crucial for patients’ survival. Two key prognostic indicators that are extremely important in post-cardiac arrest are the return of spontaneous systemic circulation and the patient’s neurological status after resuscitation. Unfortunately, cardiac arrest is characterized by a high incidence, limited return of spontaneous systemic circulation, poor neurological outcomes, and poor survival to discharge. Despite significant progress in pre-hospital and in-hospital care, sudden cardiac arrest is still characterized by high morbidity and mortality. Therefore, the impact of cardiac arrest on the quality of life is of great importance worldwide.
2. Brain Neurodegeneration after Cardiac Arrest
Brain neuropathology after cardiac arrest includes primary ischemic injury and secondary reperfusion injury, which occur sequentially, acutely during cardiac arrest and resuscitation, and chronically in the post-resuscitation stage [24]. Transient global brain ischemia resulting from cardiac arrest in humans and animals causes neurodegeneration of neurons in the hippocampus, brain cortex, amygdala, basal ganglia, thalamus, dorsal and lateral septum, olfactory tubercle, primary olfactory cortex, entorhinal cortex, and brainstem [2][13][30][31][32][33][34][35][36]. The hippocampus is one of the brain regions most susceptible to ischemia after cardiac arrest in humans [37][38][39] and in animals [40][41][42][43]. Transient global brain ischemia causes selective neurodegeneration in the CA1 area of the hippocampus in humans and animals within 2–7 days after reperfusion [30][42]. Two years after ischemia in animals, in addition to neuronal loss in ischemia-sensitive areas, various stages of neuronal pathology were also observed in other areas [42]. Acute and chronic neuronal changes have been demonstrated in brain areas unrelated to primary ischemic pathology, i.e., hippocampal areas CA2, CA3, and CA4 [42]. In the hippocampus, activation of glial cells precedes neuronal loss and continues for a long time after an ischemic event in animals [44][45] and humans [46]. In the brains of humans and animals after ischemia, changes in the white matter combined with the proliferation of glial cells have been documented [42][44][45]. Autopsy of brains after experimental ischemia with a survival time of up to 2 years and in humans after ischemia showed severe hippocampal atrophy [42][47][48]. These neuropathological alterations have been clearly associated with progressive cognitive decline in humans [48][49][50] as well as in animals [51][52].
Brain ischemia caused by cardiac arrest increases the permeability of the blood–brain barrier in humans [53] as well as animals to cellular and non-cellular blood elements, i.e., platelets [54] and amyloids [55]. In the case of post-ischemic blood–brain barrier leakage, two facts deserve attention: the first is related to the passage of amyloid into the brain, and the second is the penetration of, among others, platelets containing huge amounts of soluble amyloid, which causes additional neurotoxic damage to the brain parenchyma [42][56]. Additionally, the permeability of the blood–brain barrier was influenced by oxidative stress, neuroinflammation [45][46][57], and the LRP1 and RAGE genes related to amyloid transport, described in detail later in the work. Soluble amyloid is delivered to the brain after cardiac arrest from the circulatory system [4][58] and additionally contributes to brain vessel vasoconstriction, amyloidosis, and cerebral amyloid angiopathy [49][50].
After brain ischemia, hippocampal atrophy was demonstrated with simultaneous neurodegenerative damage to the cortex of the temporal lobe [42][49][50]. Neuronal death after cerebral ischemia due to cardiac arrest may be dependent and independent of caspase. Moreover, neuronal death dependent on amyloid and modified tau protein has been demonstrated. Current preclinical and clinical evidence indicates that cardiac arrest causes chronic neuroinflammatory responses in the brain, which further exacerbate neurodegenerative changes [44][45][46]. Particularly extensive microglial activation and neurodegeneration in the CA1 area of the hippocampus in humans and animals are evident after cardiac arrest and lead to serious neurological sequelae [45][46][57].
3. Cognitive Deficits after Cardiac Arrest
The most sensitive brain regions to ischemic damage from cardiac arrest are the hippocampus, brain cortex, basal ganglia, thalamus, and amygdala [13][32][47]. These areas are closely related to cognitive domains (Figure 1) [13][51][52]. Cognitive functions depend on complex interactions between cortical and subcortical areas through various brain networks (Figure 1) [13]. Cognitive problems develop in 42–50% of patients who survive cardiac arrest up to several years after discharge from hospital [13][59]. Other studies have reported that in people who survived cardiac arrest, 50–100% of them experienced cognitive, mood, and functioning disorders [6][7][60]. Even among patients who returned to good neurological condition after discharge from the hospital, 29% experienced memory problems (short-term memory and spatial or contextual memory) and 43% experienced cognitive impairment [28][59].
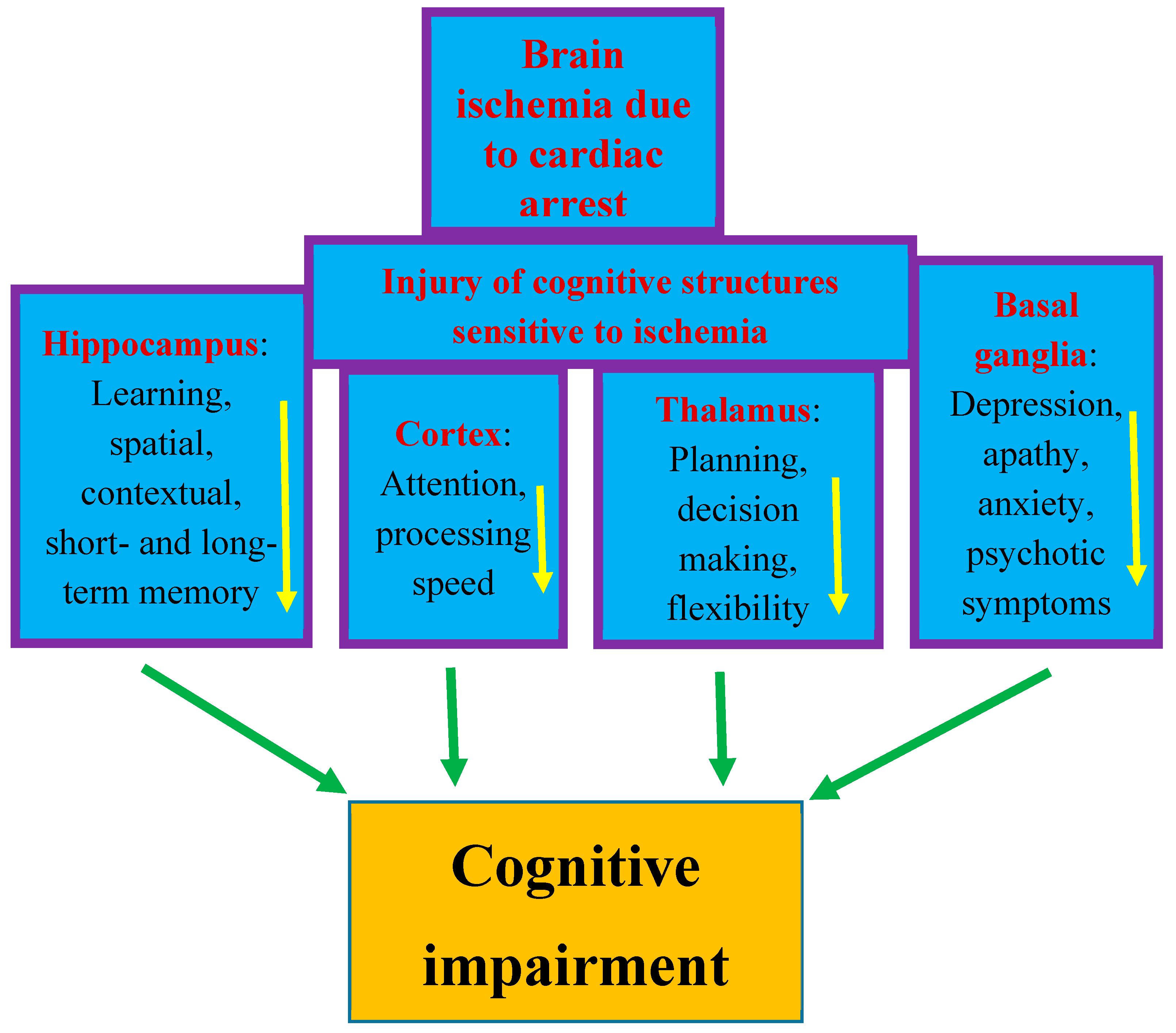
Figure 1. Structures susceptible to ischemic brain injury due to cardiac arrest and responsible for cognition. The figure shows damage to structures affecting memory, behavior, and cognitive impairment after cardiac arrest in an identical manner to that seen in Alzheimer’s disease. Arrows indicate decreased activity.
The post-ischemic hippocampus is believed to be the main structure underlying episodic memory impairment, which is the earliest and most visible clinical symptom preceding the development of dementia (Figure 1) [42][48][49][50][51]. Ischemia causes damage to the temporal cortex, which is the target area of the main axon output network from the hippocampus, so these areas are structurally and functionally related to each other and are important for learning and memory processes [13][49][50]. Thus, existing evidence indicates that cognitive and functional impairment after cardiac arrest is one of the important areas of concern for physicians [61][62][63][64][65][66][67]. The primary goal of research in the past was to improve survival after cardiac arrest. Currently, in clinical conditions, there is a search for methods that can improve neurological outcomes. Therefore, it is not surprising that research has moved beyond prognostication in the acute period following successful cardiopulmonary resuscitation to identifying mechanisms of long-term brain damage. Another currently promising area of research is the implementation of therapies that can reduce neuronal damage resulting from cerebral hypoxia and ischemia. It should be added that it is unlikely that survivors could be considered fully recovered immediately after being discharged from the hospital. Typically, sooner or later during long-term follow-up, they develop cognitive deficits, mainly related to memory and executive functions, or mild to severe impairment, including memory loss, deterioration of psychomotor, executive, and visuospatial functions, and emotional problems, including anxiety and depression [28][68][69][70]. The above-mentioned disorders affect the vast majority of patients after cardiac arrest—estimated to be as many as 88% [71]. The most frequently stated cognitive deficit is memory loss in patients who regain consciousness after cardiac arrest. It should be noted that memory with delayed recall and recognition is usually most affected, while isolated memory loss is rare. It can be summarized that the typical pattern of impairment after cardiac arrest includes deficits in memory, fine motor skills, and in executive functions [72]. According to the latest recommendations, before leaving the hospital, patients should be thoroughly assessed for short- and long-term memory deficits, cognitive and executive dysfunction, depression, and possible progression to dementia [62]. Overall, the prognosis for recovery of cognitive function to pre-arrest levels is uncertain. Despite uncertain prognoses, long-term rehabilitation has been shown to improve overall performance across a wide range of activities and should be pursued [73]. In most cases, patients are unable to return to daily activities within the first year after injury, and deficiencies are detected up to 8 years after cardiac arrest [74][75]. A study from Sweden, with an extremely long-term follow-up of 17 years after cardiac arrest, found a trend towards lower scores on cognitive tests and lower self-reported quality of life [71]. The authors concluded that survivors of cardiac arrest may experience permanent cognitive impairment, progressing to Alzheimer’s disease-type dementia [71][76]. It is suggested that the above-mentioned population is at increased risk of dementia due to the hypoxia occurring during cardiac arrest. It has been noted that the progression of cognitive decline following cardiac arrest in humans is characterized by greater memory impairment than executive dysfunction, making it similar to the prodromal form of Alzheimer’s disease dementia [76].
Cardiac arrest in humans and animals has been shown to significantly increase the risk of mild cognitive impairment, vascular cognitive impairment, and dementia, and dementia of Alzheimer’s disease type [46][51][52][77][78]. More than a quarter of patients experienced cognitive impairment four years after cardiac arrest [46][79]. Cohort studies have shown a high prevalence (54.4%) of long-term cognitive deficits and functional limitations in cardiac arrest survivors [46][80], even in those with apparently favorable neurological outcomes [46][81].
This entry is adapted from the peer-reviewed paper 10.3390/ijms25021291
References
- Stub, D.; Bernard, S.; Duffy, S.J.; Kaye, D.M. Post cardiac arrest syndrome: A review of therapeutic strategies. Circulation 2011, 123, 1428–1435.
- Sandroni, C.; Cronberg, T.; Sekhon, M. Brain injury after cardiac arrest: Pathophysiology, treatment, and prognosis. Intensiv. Care Med. 2021, 47, 1393–1414.
- Andersen, L.W.; Holmberg, M.J.; Berg, K.M.; Donnino, M.W.; Granfeldt, A. In-hospital cardiac arrest: A review. JAMA 2019, 321, 1200–1210.
- Ashton, N.J.; Moseby-Knappe, M.; Benedet, A.L.; Grötschel, L.; Lantero-Rodriguez, J.; Karikari, T.K.; Hassager, C.; Wise, M.P.; Stammet, P.; Kjaergaard, J.; et al. Alzheimer Disease Blood Biomarkers in Patients with Out-of-Hospital Cardiac Arrest. JAMA Neurol. 2023, 80, 388–396.
- Li, Z.; Xing, J. A model for predicting return of spontaneous circulation and neurological outcomes in adults after in-hospital cardiac arrest: Development and evaluation. Front. Neurol. 2023, 14, 1323721.
- Green, C.R.; Botha, J.A.; Tiruvoipati, R. Cognitive function, quality of life and mental health in survivors of our-of-hospital cardiac arrest: A review. Anaesth. Intensive Care 2015, 43, 568–576.
- Glimmerveen, A.; Verhulst, M.; Verbunt, J.; Van Heugten, C.; Hofmeijer, J. Predicting Long-Term Cognitive Impairments in Survivors after Cardiac Arrest: A Systematic Review. J. Rehabil. Med. 2023, 55, jrm00368.
- Mehra, R. Global public health problem of sudden cardiac death. J. Electrocardiol. 2007, 40, S118–S122.
- Jung, E.; Park, J.H.; Ro, Y.S.; Ryu, H.H.; Cha, K.C.; Do Shin, S.; Hwang, S.O. Cardiac Arrest Pursuit Trial with Unique Registration, Epidemiologic Surveillance (CAPTURES) project investigators. Family history, socioeconomic factors, comorbidities, health behaviors, and the risk of sudden cardiac arrest. Sci. Rep. 2023, 13, 21341.
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013, 310, 1377–1384.
- Wang, C.Y.; Wang, J.Y.; Teng, N.C.; Chao, T.T.; Tsai, S.L.; Chen, C.L.; Hsu, J.Y.; Wu, C.P.; Lai, C.C.; Chen, L. The secular trends in the incidence rate and outcomes of out-of-hospital cardiac arrest in Taiwan-A nationwide population-based study. PLoS ONE 2015, 10, e0122675.
- Hosseini, M.; Wilson, R.H.; Crouzet, C.; Amirhekmat, A.; Wei, K.S.; Akbari, Y. Resuscitating the Globally Ischemic Brain: TTM and Beyond. Neurotherapeutics 2020, 17, 539–562.
- Hagberg, G.; Ihle-Hansen, H.; Sandset, E.C.; Jacobsen, D.; Wimmer Hand Ihle-Hansen, H. Long Term Cognitive Function after Cardiac Arrest: A Mini-Review. Front. Aging Neurosci. 2022, 14, 885226.
- de Vreede-Swagemakers, J.J.; Gorgels, A.P.; Dubois-Arbouw, W.I.; van Ree, J.W.; Daemen, M.J.; Houben, L.G.; Wellens, H.J. Out-of-hospital cardiac arrest in the 1990’s: A population-based study in the Maastricht area on incidence, characteristics and survival. J. Am. Coll. Cardiol. 1997, 30, 1500–1505.
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487.
- Hwang, S.O.; Cha, K.C.; Jung, W.J.; Roh, Y.I.; Kim, T.Y.; Chung, S.P.; Kim, Y.M.; Park, J.D.; Kim, H.S.; Lee, M.J.; et al. Steering Committee of the 2020 Korean Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 2. Environment for cardiac arrest survival and the chain of survival. Clin. Exp. Emerg. Med. 2021, 8, S8–S14.
- Gräsner, J.T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016, 105, 188–195.
- Gräsner, J.T.; Wnent, J.; Herlitz, J.; Perkins, G.D.; Lefering, R.; Tjelmeland, I.; Koster, R.W.; Masterson, S.; Rossell-Ortiz, F.; Maurer, H.; et al. Survival after out-of-hospital cardiac arrest in Europe –Results of the EuReCa TWO study. Resuscitation 2020, 148, 218–226.
- Nichol, G.; Thomas, E.; Callaway, C.W.; Hedges, J.; Powell, J.L.; Aufderheide, T.P.; Rea, T.; Lowe, R.; Brown, T.; Dreyer, J.; et al. Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008, 300, 1423–1431.
- Medina, J.A.; Quintero, J.A.; de Paz, D.A.; Scarpetta, D.F.; Castro, C.A.; Paker, N.A.; Carvajal, S.M. Cardiac arrest in an emergency department in Colombia during 2011–2020: A descriptive study. Int. J. Crit. Illn. Inj. Sci. 2023, 13, 132–137.
- Beck, B.; Bray, J.; Cameron, P.; Smith, K.; Walker, T.; Grantham, H.; Hein, C.; Thorrowgood, M.; Smith, A.; Inoue, M.; et al. Aus-ROC Steering Committee. Regional variation in the characteristics, incidence and outcomes of out-of-hospital cardiac arrest in Australia and New Zealand: Results from the Aus-ROC Epistry. Resuscitation 2018, 126, 49–57.
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American Heart Association. Circulation 2019, 139, e56–e528.
- Shao, F.; Li, C.S.; Liang, L.R.; Qin, J.; Ding, N.; Fu, Y.; Yang, K.; Zhang, G.Q.; Zhao, L.; Zhao, B.; et al. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation 2016, 102, 51–56.
- Sekhon, M.S.; Ainslie, P.N.; Griesdale, D.E. Clinical pathophysiology of hypoxic ischemic brain injury after cardiac arrest: A “two-hit” model. Crit. Care 2017, 21, 90.
- Lemiale, V.; Dumas, F.; Mongardon, N.; Giovanetti, O.; Charpentier, J.; Chiche, J.D.; Carli, P.; Mira, J.P.; Nolan, J.; Cariou, A. Intensive care unit mortality after cardiac arrest: The relative contribution of shock and brain injury in a large cohort. Intensive Care Med. 2013, 39, 1972–1980.
- Geocadin, R.G.; Callaway, C.W.; Fink, E.L.; Golan, E.; Greer, D.M.; Ko, N.U.; Lang, E.; Licht, D.J.; Marino, B.S.; McNair, N.D.; et al. Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: A scientific statement from the American Heart Association. Circulation 2019, 140, e517–e542.
- Varon, J.; Marik, P.E.; Einav, S. Therapeutic hypothermia: A state-of-the-art emergency medicine perspective. Am. J. Emerg. Med. 2012, 30, 800–810.
- Lilja, G.; Nielsen, N.; Friberg, H.; Horn, J.; Kjaergaard, J.; Nilsson, F.; Pellis, T.; Wetterslev, J.; Wise, M.P.; Bosch, F.; et al. Cognitive function in survivors of out-of-hospital cardiac arrest after target temperature management at 33 °C versus 36 °C. Circulation 2015, 131, 1340–1349.
- Ahn, J.H.; Lee, T.K.; Tae, H.J.; Kim, B.; Sim, H.; Lee, J.C.; Kim, D.W.; Kim, Y.S.; Shin, M.C.; Park, Y.; et al. Neuronal Death in the CNS Autonomic Control Center Comes Very Early after Cardiac Arrest and Is Not Significantly Attenuated by Prompt Hypothermic Treatment in Rats. Cells 2021, 10, 60.
- Weng, Y.C.; Huang, Y.T.; Chiang, I.C.; Chuang, H.C.; Lee, T.H.; Tan, T.H.; Chou, W.H. DUSP6 deficiency attenuates neurodegeneration after global cerebral ischemia. Int. J. Mol. Sci. 2023, 24, 7690.
- Kagstrom, E.; Smith, M.L.; Siesjo, B.K. Local cerebral blood flow in the recovery period following complete cerebral ischemia in the rat. J. Cereb. Blood Flow Metab. 1983, 3, 170–182.
- Blomqvist, P.; Wieloch, T. Ischemic brain damage in rats following cardiac arrest using a long-term recovery model. J. Cereb. Blood Flow Metab. 1985, 5, 420–423.
- Kawai, K.; Nitecka, L.; Ruetzler, C.A.; Nagashima, G.; Joó, F.; Mies, G.; Nowak TSJr Saito, N.; Lohr, J.M.; Klatzo, I. Global cerebral ischemia associated with cardiac arrest in the rat: I. Dynamics of early neuronal changes. J. Cereb. Blood Flow Metab. 1992, 12, 238–249.
- Krajewski, S.; Mai, J.K.; Krajewska, M.; Sikorska, M.; Mossakowski, M.J.; Reed, J.C. Upregulation of bax protein levels in neurons following cerebral ischemia. J. Neurosci. 1995, 15, 6364–6376.
- Kawai, K.; Nowak, T.S., Jr.; Klatzo, I. Loss of parvalbumin immunoreactivity defines selectively vulnerable thalamic reticular nucleus neurons following cardiac arrest in the rat. Acta Neuropathol. 1995, 89, 262–269.
- Böttiger, B.W.; Schmitz, B.; Wiessner, C.; Vogel, P.; Hossmann, K.A. Neuronal stress response and neuronal cell damage after cardiocirculatory arrest in rats. J. Cereb. Blood Flow Metab. 1998, 18, 1077–1087.
- Petito, C.K.; Feldmann, E.; Pulsinelli, W.A.; Plum, F. Delayed hippocampal damage in humans following cardiorespiratory arrest. Neurology 1987, 37, 1281–1286.
- Hu, B.R.; Liu, C.L.; Park, D.J. Alteration of MAP kinase pathways after transient forebrain ischemia. J. Cereb. Blood Flow Metab. 2000, 20, 1089–1095.
- Sawe, N.; Steinberg, G.; Zhao, H. Dual roles of the MAPK/ERK1/2 cell signaling pathway after stroke. J. Neurosci. Res. 2008, 86, 1659–1669.
- Sadowski, M.; Wisniewski, H.M.; Jakubowska-Sadowska, K.; Tarnawski, M.; Lazarewicz, J.W.; Mossakowski, M.J. Pattern of neuronal loss in the rat hippocampus following experimental cardiac arrest-induced ischemia. J. Neurol. Sci. 1999, 168, 13–20.
- Sadowski, M.; Lazarewicz, J.W.; Jakubowska-Sadowska, K.; Wisniewski, H.M.; Mossakowski, M.J.; Brown, W.T. Long-term changes in calbindin D(28K) immunoreactivity in the rat hippocampus after cardiac arrest. Neurosci. Lett. 2002, 321, 90–94.
- Pluta, R.; Ułamek, M.; Jabłoński, M. Alzheimer’s mechanisms in ischemic brain degeneration. Anat. Rec. 2009, 292, 1863–1881.
- Warenits, A.M.; Hatami, J.; Müllebner, A.; Ettl, F.; Teubenbacher, U.; Magnet, I.A.M.; Bauder, B.; Janata, A.; Miller, I.; Moldzio, R.; et al. Motor Cortex and Hippocampus Display Decreased Heme Oxygenase Activity 2 Weeks after Ventricular Fibrillation Cardiac Arrest in Rats. Front. Med. 2020, 7, 513.
- Sekeljic, V.; Bataveljic, D.; Stamenkovic, S.; Ułamek, M.; Jabłoński, M.; Radenovic, L.; Pluta, R.; Andjus, P.R. Cellular markers of neuroinflammation and neurogenesis after ischemic brain injury in the long-term survival rat model. Brain Struct. Funct. 2012, 217, 411–420.
- Radenovic, L.; Nenadic, M.; Ułamek-Kozioł, M.; Januszewski, S.; Czuczwar, S.J.; Andjus, P.R.; Pluta, R. Heterogeneity in brain distribution of activated microglia and astrocytes in a rat ischemic model of Alzheimer’s disease after 2 years of survival. Aging 2020, 12, 12251–12267.
- Traub, J.; Frey, A.; Störk, S. Chronic Neuroinflammation and Cognitive Decline in Patients with Cardiac Disease: Evidence, Relevance, and Therapeutic Implications. Life 2023, 13, 329.
- Pluta, R. The role of apolipoprotein E in the deposition of β-amyloid peptide during ischemia–reperfusion brain injury. A model of early Alzheimer’s disease. Ann. N. Y. Acad. Sci. 2000, 903, 324–334.
- Gemmell, E.; Tam, E.; Allan, L.; Hall, R.; Khundakar, A.; Oakley, A.E.; Thomas, A.; Deramecourt, V.; Kalaria, R.N. Neuron volumes in hippocampal subfields in delayed poststroke and aging-related dementias. J. Neuropathol. Exp. Neurol. 2014, 73, 305–311.
- Goulay, R.; Mena Romo, L.; Hol, E.M.; Dijkhuizen, R.M. From stroke to dementia: A Comprehensive review exposing tight interactions between stroke and amyloid-β formation. Transl. Stroke Res. 2020, 11, 601–614.
- Rost, N.S.; Brodtmann, A.; Pase, M.P.; van Veluw, S.J.; Biffi, A.; Duering, M.; Hinman, J.D.; Dichgans, M. Post-stroke cognitive impairment and dementia. Circ. Res. 2022, 130, 1252–1271.
- Kiryk, A.; Pluta, R.; Figiel, I.; Mikosz, M.; Ulamek, M.; Niewiadomska, G.; Jablonski, M.; Kaczmarek, L. Transient brain ische-mia due to cardiac arrest causes irreversible long-lasting cognitive injury. Behav. Brain Res. 2011, 219, 1–7.
- Cohan, C.H.; Neumann, J.T.; Dave, K.R.; Alekseyenko, A.; Binkert, M.; Stransky, K.; Lin, H.W.; Barnes, C.A.; Wright, C.B.; Perez Pinzon, M.A. Effect of cardiac arrest on cognitive impairment and hippocampal plasticity in middle-aged rats. PLoS ONE 2015, 10, e0124918.
- Park, J.S.; You, Y.; Min, J.H.; Yoo, I.; Jeong, W.; Cho, Y.; Ryu, S.; Lee, J.; Kim, S.W.; Cho, S.U.; et al. Study on the timing of severe blood-brain barrier disruption using cerebrospinal fluid-serum albumin quotient in post cardiac arrest patients treated with targeted temperature management. Resuscitation 2019, 135, 118–123.
- Pluta, R.; Lossinsky, A.S.; Walski, M.; Wisniewski, H.M.; Mossakowski, M.J. Platelet occlusion phenomenon after short- and long-term survival following complete cerebral ischemia in rats produced by cardiac arrest. J. Hirnforsch. 1994, 35, 463–471.
- Pluta, R.; Barcikowska, M.; Januszewski, S.; Misicka, A.; Lipkowski, A.W. Evidence of blood-brain barrier permeability/leakage for circulating human Alzheimer’s beta-amyloid-(1-42)-peptide. Neuroreport 1996, 7, 1261–1265.
- Pluta, R.; Miziak, B.; Czuczwar, S.J. Post-Ischemic Permeability of the Blood-Brain Barrier to Amyloid and Platelets as a Factor in the Maturation of Alzheimer’s Disease-Type Brain Neurodegeneration. Int. J. Mol. Sci. 2023, 24, 10739.
- Ousta, A.; Piao, L.; Fang, Y.H.; Vera, A.; Nallamothu, T.; Garcia, A.J., 3rd; Sharp, W.W. Microglial Activation and Neurological Outcomes in a Murine Model of Cardiac Arrest. Neurocrit. Care 2022, 36, 61–70.
- Zetterberg, H.; Mörtberg, E.; Song, L.; Chang, L.; Provuncher, G.K.; Patel, P.P.; Ferrell, E.; Fournier, D.R.; Kan, C.W.; Campbell, T.G.; et al. Hypoxia due to cardiac arrest induces a time-dependent increase in serum amyloid β levels in humans. PLoS ONE 2011, 6, e28263.
- Peeters-Scholte, C.; Meilin, S.; Berckovich, Y.; Westers, P. 2-iminobiotin, a selective inhibitor of nitric oxide synthase, improves memory and learning in a rat model after four vessel occlusion, mimicking cardiac arrest. PLoS ONE 2023, 18, e0291915.
- Moulaert, V.R.; Verbunt, J.A.; van Heugten, C.M.; Wade, D.T. Cognitive impairments in survivors of out-of-hospital cardiac arrest: A systematic review. Resuscitation 2009, 80, 297–305.
- Sabedra, A.R.; Kristan, J.; Raina, K.; Holm, M.B.; Callaway, C.W.; Guyette, F.X.; Dezfulian, C.; Doshi, A.A.; Rittenberger, J.C.; Post Cardiac Arrest Service. Neurocognitive outcomes following successful resuscitation from cardiac arrest. Resuscitation 2015, 90, 67–72.
- Perez, C.A.; Samudra, N.; Aiyagari, V. Cognitive and Functional Consequence of Cardiac Arrest. Curr. Neurol. Neurosci. Rep. 2016, 16, 70.
- Steinbusch, C.V.M.; van Heugten, C.M.; Rasquin, S.M.C.; Verbunt, J.A.; Moulaert, V.R.M. Cognitive impairments and subjective cognitive complaints after survival of cardiac arrest: A prospective longitudinal cohort study. Resuscitation 2017, 120, 132–137.
- Wagner, M.K.; Berg, S.K.; Hassager, C.; Armand, S.; Møller, J.E.; Ekholm, O.; Rasmussen, T.B.; Fisher, P.M.; Knudsen, G.M.; Stenbæk, D.S. Cognitive impairment and psychopathology in out-of-hospital cardiac arrest survivors in Denmark: The REVIVAL cohort study protocol. BMJ Open 2020, 10, e038633.
- Joshi, V.L.; Tang, L.H.; Borregaard, B.; Zinckernagel, L.; Mikkelsen, T.B.; Taylor, R.S.; Christiansen, S.R.; Nielsen, J.F.; Zwisler, A.D. Long-term physical and psychological outcomes after out-of-hospital cardiac arrest-protocol for a national cross-sectional survey of survivors and their relatives (the DANCAS survey). BMJ Open 2021, 11, e045668.
- Amacher, S.A.; Bohren, C.; Blatter, R.; Becker, C.; Beck, K.; Mueller, J.; Loretz, N.; Gross, S.; Tisljar, K.; Sutter, R.; et al. Long-term survival after out-of-hospital cardiac arrest: A systematic review and meta-analysis. JAMA Cardiol. 2022, 7, 633–643.
- Huebschmann, N.A.; Cook, N.E.; Murphy, S.; Iverson, G.L. Cognitive and Psychological Outcomes Following Pediatric Cardiac Arrest. Front. Pediatr. 2022, 10, 780251.
- Lilja, G.; Nilsson, G.; Nielsen, N.; Friberg, H.; Hassager, C.; Koopmans, M.; Kuiper, M.; Martini, A.; Mellinghoff, J.; Pelosi, P.; et al. Anxiety and depression among out-of-hospital cardiac arrest survivors. Resuscitation 2015, 97, 68–75.
- Mion, M.; Simpson, R.; Johnson, T.; Oriolo, V.; Gudde, E.; Rees, P.; Quinn, T.; Vopelius-Feldt, V.J.; Gallagher, S.; Mozid, A.; et al. British cardiovascular intervention society consensus position statement on out-of-hospital cardiac arrest 2: Post-discharge rehabilitation. Interv. Cardiol. 2022, 17, e19.
- Kim, J.S.; Kim, Y.J.; Ryoo, S.M.; Ahn, S.; Kim, W.Y. Telephone-based evaluation of cognitive impairment and mood disorders in cardiac arrest survivors with good neurologic outcomes: A retrospective cohort study. Sci. Rep. 2023, 13, 18065.
- Andersson, A.E.; Rosén, H.; Sunnerhagen, K.S. Life after cardiac arrest: A very long-term follow-up. Resuscitation 2015, 91, 99–103.
- Lim, C.; Verfaellie, M.; Schnyer, D.; Lafleche, G.; Alexander, M.P. Recovery, long-term cognitive outcome and quality of life following out-of-hospital cardiac arrest. J. Rehabil. Med. 2014, 46, 691–697.
- Fertl, E.; Vass, K.; Sterz, F.; Gabriel, H.; Auff, E. Neurological rehabilitation of severely disabled cardiac arrest survivors. Part I. Course of post-acute inpatient treatment. Resuscitation 2000, 47, 231–239.
- Lundgren-Nilsson, Å.; Rosén, H.; Hofgren, C.; Sunnerhagen, K.S. The first year after successful cardiac resuscitation: Function, activity, participation and quality of life. Resuscitation 2005, 66, 285–289.
- Mateen, F.J.; Josephs, K.A.; Trenerry, M.R.; Felmlee-Devine, M.D.; Weaver, A.L.; Carone, M.; White, R.D. Long-term cognitive outcomes following out-of-hospital cardiac arrest. Neurology 2011, 77, 1438–1445.
- Czuczwar, M. Cognitive impairment and dementia following ischemic stroke and cardiac arrest in humans. In Brain Ischemia: Alzheimer’s Disease Mechanisms; Pluta, R., Ed.; Nova Science Publishers, Inc.: New York, NY, USA, 2019; pp. 1–10.
- Wolters, F.J.; Segufa, R.A.; Darweesh, S.K.L.; Bos, D.; Ikram, M.A.; Sabayan, B.; Hofman, A.; Sedaghat, S. Coronary heart disease, heart failure, and the risk of dementia: A systematic review and meta-analysis. Alzheimers Dement. 2018, 14, 1493–1504.
- Zhang, W.; Luo, P. Myocardial Infarction Predisposes Neurodegenerative Diseases. J. Alzheimers Dis. 2020, 74, 579–587.
- Buanes, E.A.; Gramstad, A.; Sovig, K.K.; Hufthammer, K.O.; Flaatten, H.; Husby, T.; Langorgen, J.; Heltne, J.K. Cognitive function and health-related quality of life four years after cardiac arrest. Resuscitation 2015, 89, 13–18.
- Caro-Codon, J.; Rey, J.R.; Lopez-de-Sa, E.; Gonzalez Fernandez, O.; Rosillo, S.O.; Armada, E.; Iniesta, A.M.; Fernandez de Bobadilla, J.; Ruiz Cantador, J.; Rodriguez Sotelo, L.; et al. Long-term neurological outcomes in out-of-hospital cardiac arrest patients treated with targeted-temperature management. Resuscitation 2018, 133, 33–39.
- Byron-Alhassan, A.; Collins, B.; Bedard, M.; Quinlan, B.; Le May, M.; Duchesne, L.; Osborne, C.; Wells, G.; Smith, A.M.; Tulloch, H.E. Cognitive dysfunction after out-of-hospital cardiac arrest: Rate of impairment and clinical predictors. Resuscitation 2021, 165, 154–160.
This entry is offline, you can click here to edit this entry!
