Chronic obstructive pulmonary disease (COPD), the sixth leading cause of death in the United States in 2022 and the third leading cause of death in England and Wales in 2022, is associated with high symptom burden, particularly dyspnoea. Frailty is a complex clinical syndrome associated with an increased vulnerability to adverse health outcomes. The aim of this review was to explore the current evidence of the influence of frailty on symptoms in patients with a confirmed diagnosis of COPD according to GOLD guidelines. Fourteen studies report a positive association between frailty and symptoms, including dyspnoea, assessed with the COPD Assessment Test (CAT) and the modified Medical Research Council (mMRC) scale. Data were analysed in a pooled a random-effects meta-analysis of mean differences (MDs). There was an association between COPD patients living with frailty and increased CAT score versus COPD patients without frailty [pooled SMD, 1.79 (95% CI 0.72–2.87); I2 = 99%]. A lower association was found between frailty and dyspnoea measured by the mMRC scale versus COPD patients without frailty [pooled SMD, 1.91 (95% CI 1.15–2.66); I2 = 98%]. The prevalence of frailty ranged from 8.8% to 82% and that of pre-frailty from 30.4% to 73.7% in people living with COPD. The available evidence supports the role of frailty in worsening symptom burden in COPD patients living with frailty. The review shows that frailty is common in patients with COPD. Future research is needed to have further details related to the data from CAT to improve our knowledge of the frailty impact in this population.
1. Introduction
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of morbidity and remains one of the top three causes of death worldwide [
1]. The global prevalence of COPD increases with age, and the burden related to is expected to rise over the next years due to persistent exposure to risk factors and ageing of the world’s population [
1,
2]. According to the GOLD criteria, roughly 400 million people have been reported to suffer from COPD globally in 2019 [
3]. COPD is characterised by chronic respiratory symptoms, including dyspnoea and activity limitation, that have a negative impact on patients’ quality of life and increase the risk of depression and anxiety [
1].
Frailty is a complex syndrome described as a state of reduced physiological reserve causing increased vulnerability to adverse events and external stressors. This vulnerability can result in disability, admission to a hospital or a long-term facility, and increased risk of all-cause mortality. There are different validated tools available to measure frailty, ranging from simple assessment of functional status to complex, multi-domain scoring systems that evaluate cognitive, physical, and functional ability [
4,
5,
6,
7]. Two main classifications of frailty (the deficit model and the phenotype model) are widely accepted and frequently used in clinical practice [
5,
8]. The frailty phenotype model proposed by Fried et al. [
5] is defined as the presence of three or more of the following domains: exhaustion, weakness, slowness, low activity, and unintentional weight loss. The frailty index (FI) [
8] is a quantification of the cumulative burden of health deficits including laboratory findings, physical function disabilities, diseases, symptoms, sensory difficulties, and cognition difficulties.
2. Overview of Symptoms in COPD
Dyspnoea, also known as shortness of breath or breathlessness, is the most typical symptom and debilitating for patients with COPD and is associated with a deterioration in their physical activity [
10]. Dyspnoea is defined as “a subjective experience of breathing discomfort that consists of qualitatively distinct sensation that vary in intensity” [
11] and results from multiple mechanism, including air trapping, dynamic hyperinflation, and gas exchange abnormalities [
12].
Fatigue, described as an individual feeling of tiredness and being drained of energy until exhaustion, is one of the most common symptoms in COPD. It has an impact on activities of daily living and is associated with frustration and problems with concentration [
13]. The intensity of fatigue is variable and, similar to dyspnoea, can be increased by intercurrent exacerbation of COPD. Other cardinal symptoms of patients with COPD include
chronic cough with sputum production, chest tightness, and
wheezing which may be recurrent as well [
1].
The prevalence of dyspnoea is high across all stages of airflow obstruction [
14]. Dyspnoea intensity has been associated with age ≥70 years, higher severity of airflow obstruction, female gender, obesity, history of moderate-to-severe exacerbations, and comorbidities [
15]. Fatigue has been also reported in mild COPD [
16].
3. Assessment of Symptoms in COPD
The degree of airflow obstruction can be a poor effective predictor of symptom burden in COPD, especially for dyspnoea and fatigue. Validated questionnaires have been developed to promote a more comprehensive evaluation of breathlessness and other relevant symptoms in these patients. All symptoms in COPD represent an individual experience, difficult to quantify numerically with questionnaires; hence, several scales are available both in research settings and clinical practice [
1].
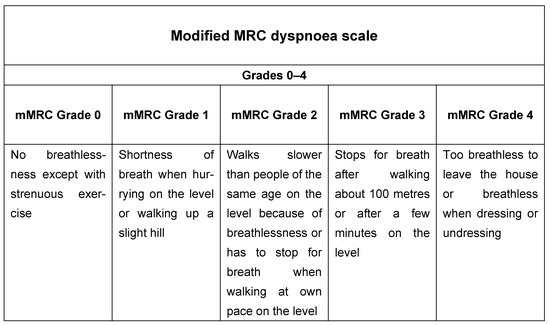
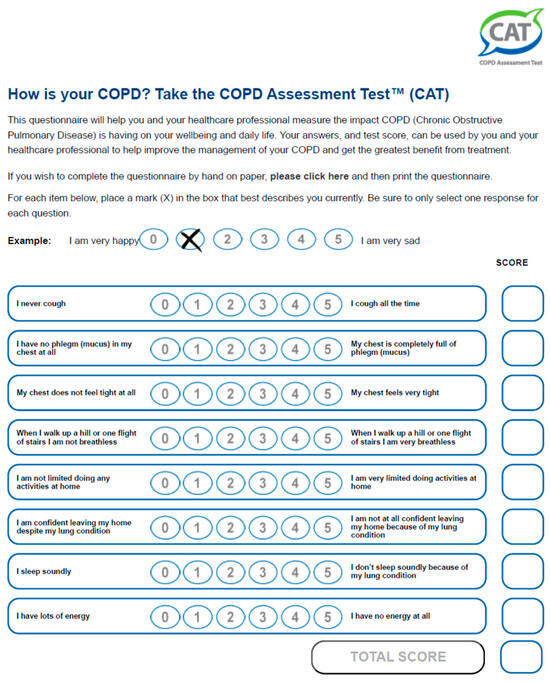
These include the modified Medical Research Council (mMRC) dyspnoea scale (
Figure 1), including five statements to measure the degree of disability due to breathlessness in daily activities on a scale from 0 to 4 [
17,
18], and multidimensional questionnaires such as the COPD Assessment Test (CAT) (
Figure 2), which includes eight items describing the clinical manifestations of COPD. Cough, presence of mucus, chest tightness, dyspnoea, limitation in activities of daily living, feeling confident, sleeping, and energy are the components of the test, scoring 0 to 40 [
19]. Both are used to describe level of symptoms in the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations that suggest a therapeutic strategy based on the history of exacerbations and burden of symptoms in stable COPD (GOLD 2023) [
1].
Figure 1. Modified Medical Research Council dyspnoea scale.
Figure 2. COPD Assessment Test.
4. Psychological Burden of Symptoms in COPD Patients
Dyspnoea and fatigue have been associated with anxiety and depression in COPD [
20]. These comorbidities may result from the distress related to breathlessness and fatigue that are perceived as negative emotions associated with fear and feeling of sadness by patients [
11], resulting in worse patient health and quality of life. Whilst these comorbidities have not been fully studied, the reported prevalences, mainly due to the population assessed in primary or secondary care settings, vary widely with mean range of 35–40% for depression and 28–36% for anxiety [
21,
22]. Anxiety and fear related to COPD are prevalent complications that widely contribute to disability and difficulties in activities of daily living in this population. Many patients adopt a sedentary lifestyle in anticipation of dyspnoea, and fear of exhaustion can result in experiencing more severe shortness of breath during exercise [
23]. It has been noted that patients with COPD and associated depression experience more dyspnoea than their counterparts without depression [
24]. The depression symptoms may range from sub-clinical depressive symptoms to clinical depression and, along with anxiety, have an effect on lack of energy, irritability, and feelings of demoralisation [
23,
25].
This entry is adapted from the peer-reviewed paper 10.3390/jcm13040984