1. Complication Profile
As an emerging surgical technique with known and well-established alternatives, it is important to characterize the complication profile of prone-transpsoas access-spine surgery early and often to ensure the benefits are conferred while maintaining an acceptable safety profile. To date, in cases where prone lateral surgery is undertaken, its novelty has precluded a large number of studies, but the recent literature from Farber et al., Soliman et al., and pooled analyses have shown that complications, of all causes, are comparable to those in conventional, two-position, lateral surgery
[1][2]. Likewise, looking at individual complications, it has been demonstrated that critical complications, including post-operative neurologic deficit, inadvertent anterior longitudinal ligament release, vascular or ureter injury, spinal fluid leak, and psoas hematoma, are comparable or decreased in relation to traditional lateral surgery.
1.1. Neuropathy
The most common complications arising from both prone lateral and traditional lateral access spine surgeries are new post-operative sensory and motor deficits. Defects include ipsilateral paresthesias, dysthesias, and lower-extremity weakness. In a systematic review examining thigh symptoms after traditional lateral interbody fusion, Gammal et al. reported an incidence range for new-onset postoperative sensory changes at 3.1–60.7%
[3]. Authors cite inconsistent reporting standards for this wide range, stating that many authors of the included studies view transient neurologic symptoms as side-effects of required psoas manipulation rather than a true complication. Comparatively, in a 365 PTP-patient retrospective study by Soliman et al., the authors showed that prone lateral fusion resulted in new onset radiculopathy or lower-extremity sensory symptoms in only 8.2% of patients
[2]. Farber et al. and Patel et al. reported similarly low rates of new onset of thigh neuropraxia among their PTP cohorts, at 13.3% and 11.9% respectively
[1][4].
With respect to motor deficits in lateral position surgery, Hijji et al., in a meta-analysis of nearly 7000 patients, cited an incidence of 14.1% for new onset transient motor weakness and 5.1% for permanent motor or sensory loss
[5]. Comparatively, in Soliman et al.’s multi-center PTP study, only 21 of 365 (5.8%) patients developed ipsilateral motor weakness—5 (1.3%) of which were persistent after 7-month follow-up
[2]. Likewise, Farber et al. and Patel et al. reported few long-term post-operative motor deficits during one-year follow up, 1.2% and 0%, in their respective retrospective studies
[1][4].
Although these data on prone lateral surgery are limited in sample size, the current evidence suggests that prone lateral surgery is safer than traditional lateral decubitus access with respect to new onset sensory and motor deficits. Taken together with the previously described cadaveric and radiographic studies describing more favorable access anatomy, the prone position anatomic augmentations are clinically translatable.
1.2. Inadvertent Anterior Longitudinal Ligament Release
In the aforementioned lateral–decubitus meta-analysis by Hijji et al., the rate of inadvertent anterior longitudinal ligament (ALL) release was reported to be 2.9%
[5]. Similarly, in their PTP cohort, Soliman et al. reported an ALL rupture incidence of 2.2%, totaling 8 of the 365 patients
[2]. Farber et al. (5, 2.3%) and Buckland et al. (3, 1.2%) describe similar rates of ALL release in their PTP cohorts
[1][6]. Further, in their single-surgeon, retrospective, prone lateral interbody fusion study, Patel et al. reported that all-cause complications, including ALL rupture, occurred only in the first 20% of patients, suggesting an inherent learning curve
[4]. It is expected that increased repetitions will lead to the identification and avoidance of intraoperative factors such as gravity-induced ventral retractor migration.
1.3. Vascular Injury
Vascular injury is a dreaded, but exceedingly rare, complication of spinal surgery and associated access. Hijji et al. cited a single (0.12%) aortic injury and two (0.25%) common iliac vein lacerations in their meta-analysis of lateral interbody fusions
[5]. Similarly, Soliman et al. cited the incidence of major vascular injury, common iliac vein laceration, at 1 (0.3%) in their multicenter study
[2]. Notably, this occurred during ALIF access, not the prone-transpsoas portion of the procedure. Farber et al. described five cases (2.0%) of segmental artery bleeding in their systematic review, all of which arose from the same study and were controlled intraoperatively with no sequalae
[1]. There were no universal reporting standards for vascular injuries in these studies; it may be the case that minor vascular injury, including controlled segmental bleeding, is largely underreported. The favorable neurovascular shifts while prone and the larger safe zone created by prone positioning may led to less blood loss in this position; however, this requires further study
[7][8][9].
1.4. Other (Durotomy, Hematoma, and Ureter Injury)
The last of the major prone-transpsoas surgery complications, durotomy, psoas hematoma, and ureter injury, have a comparable or better cited incidence than those described in traditional lateral surgery. Hijji et al. reported durotomy, psoas hematoma, and ureter injury rates of 1.8%, 1.1%, and 0.9%, respectively
[5]. Comparatively, Farber et al. (F) and Soliman et al. (S) reported a similar or lower incidence of these feared complications—durotomy: 0.6% (F) and 0% (S), psoas hematoma: 1.3% (F) and 0.5% (S), and ureter injury: 0.3% (S)
[1][2].
When evaluating the existing data within the published literature, it becomes evident that the emerging prone lateral technique exhibits a commendable safety record and acceptable complication profile. It is critical to acknowledge that all the studies on PTP published to date have a low level of evidence and are limited to retrospective case series. Additionally, it is important to note that the comparisons made to traditional lateral surgery are not direct comparisons with respect to patient selection and confounders; therefore, medical decisions cannot be made from these data alone. However, when synthesizing the available literature, it is clear that prone lateral surgery is at least as safe as its longer-standing counterparts. To gain a more comprehensive understanding of the long-term complication rates associated with this approach, further research involving extended follow-up and randomized prospective study is imperative.
2. Current Applications
The transpsoas approach is gaining traction in modern spine surgery due to its versatility in addressing various conditions, including degeneration, adjacent segment disease, deformity, anterior column realignment, corpectomy, and pseudarthrosis. This novel access trajectory combines the anatomic advantages of both prone and lateral surgery, without compromising, and in many cases improving, patient safety and outcomes, and without necessitating patient repositioning.
Only recently have lumbar corpectomies, anterior column realignments, and deformity corrections been performed via a lateral decubitus transpsoas approach. Lateral decubitus positioning confers several key advantages in these cases compared to the prone counterpart, such as the improved biomechanical stability imparted by larger interbody cages when combined with posterior fusion
[10]. The lateral decubitus position alone, however, does not facilitate complex cases involving trauma, deformities, or large tumors, which require multi-stage surgeries for direct, open, posterior column access. Taken together, in cases where lateral, transpsoas access facilitates key advantages and open posterior access is required, PTP surgery allows for the maintenance of operative efficiency without compromise.
2.1. Degenerative Spondylolisthesis
As PTP adoption increases, the literature has begun to demonstrate wide-ranging clinical applications that significantly overlap with the conditions currently treated with two-position surgery. In the case of spondylolisthesis, the gold standard treatment is decompression and fusion, as well as circumferential surgery
[11][12]. Similarly, in the case of adult degenerative scoliosis, surgical treatment options range from neural decompression alone to decompression plus arthrodesis
[13]. Although there is a paucity of studies describing PTP for de novo degenerative spondylolisthesis, a case series by Stone et al. describes several challenging degenerative cases that were aided by this access trajectory, including grade-1 spondylolisthesis, coronal deformity, and degenerative scoliosis
[14]. The advantage of PTP in these cases is clear: the posterior column is accessed in the more familiar and anatomically favorable prone position, neural elements are decompressed, and the spinal column is stabilized without patient repositioning.
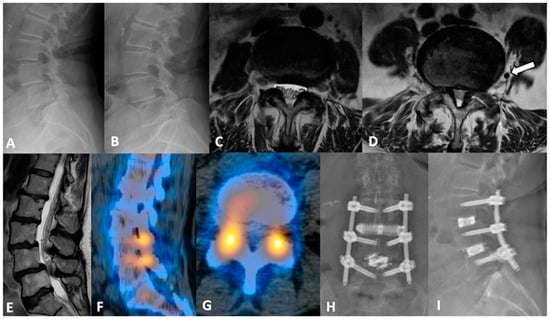
The authors present a representative case highlighting the correcting power of PTP, as well as its ability to be combined with other posterior approaches as needed. Case 2 is a 70-year-old-female who originally presented with lower back pain radiating to the right leg and grade 4+/5 weakness on ankle dorsiflexion. Prior to presentation, she exhausted all non-surgical treatment modalities. Preoperative imaging was notable for grade 1 spondylolisthesis at L3-4, dynamic instability affecting L4-5, and evidence of severe central stenosis and bilateral foraminal stenosis of L4-5. CT SPECT revealed an increased radiotracer uptake at both levels’ facet joints. Importantly, there appeared to be a vessel at the mid-point of the vertebral body at L4-5 (Figure 1D).
Figure 1. (A,B) dynamic lumbar films with variable grades of spondylolisthesis at L3-4 and L4-5. (C) axial MRI view at the L3-4 level, and (D) at L4-5 level with (white arrow) a sizable vessel in the left lateral space. Psoas muscle morphology and considerable canal stenosis are showcased via (E) sagittal view. (F,G) sagittal and axial CT SPECT slices demonstrating increased uptake at both L3-4 and L4-5 facets, confirming pain location. (H,I) postoperative AP and lateral lumbar films.
2.2. Adjacent Segment Disease
Adjacent segment disease (ASD) is a well-described sequalae of interbody fusion that often requires surgical correction
[15]. Single-position lateral decubitus surgery for ASD facilitates large interbody cage placement; however, it requires posterior instrumentation to achieve optimal construct stability
[10][16]. These ASD cases, which require instrument exchange and direct posterior decompression, require an intraoperative position change. PTP has gained traction in this avenue as it offers a means of harnessing the advantages of lateral access in prone positioning. The evidence on PTP for ASD is limited; however, in the largest case series to date, Wang et al. demonstrated the feasibility of PTP in ASD intervention without compromising safety
[17]. Again, this team was able to achieve lordosis correction matching their chosen interbody of 10 degrees without posterior osteotomy
[17].
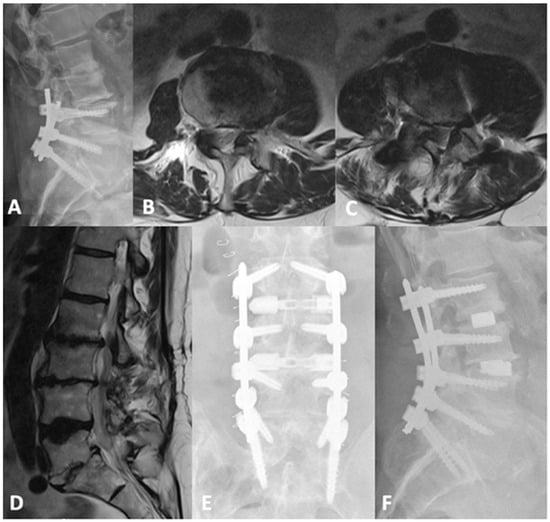
Below, the authors present a representative adjacent segment disease case. Case 3 is an 82-year-old male with remote history of L4-S1 minimally invasive decompression and fusion for back pain. Three years later, he re-presented with recurrent low back pain and intermittent radiation to both lower limbs. New imaging showed L2-L3 and L3-L4 moderate-to-severe spinal canal stenosis and moderate bilateral neuroforaminal narrowing. Since the offered L2-3 and L3-4 facet injections provided him with adequate but temporary pain relief and the evidence of ASD, here ultimately offered and proceeded with L2-4 PTP interbody fusion with extension of previous posterior instrumentation. Preoperative pelvic incidence (PI) and lumbar lordosis (LL) were 54° and 47°, respectively. LL improved to 56° postoperatively. The surgery was completed with 200 mL estimated blood loss, and without complication. The postoperative course was uneventful, and the patient was discharged home, Figure 2.
Figure 2. (A) lateral lumbar X-rays of the previous L4-S1 fusion with advanced degenerative changes and decreased disc heights at L2-3 and L3-4. Axial T2-weighted MRI sections of (B) L2-3 and (C) L3-4 levels and (D) a sagittal slice demonstrating the bilateral recess and central canal stenosis. (E,F) are postoperative AP and lateral views showing the extension of the fusion to L2 and augmented disc heights.
3. Complex Applications
3.1. Deformity
As is the case with other spine pathologies, deformity is often a quality-of-life-impacting condition
[18]. Definitive surgical correction is often required; however, these procedures are typically large, open cases associated with significant risks and complications
[19]. Minimally invasive surgery such as LLIF and its variations are effective means of deformity correction in many cases and mitigate many of the pitfalls of open spine surgery
[20]. Staged or two- or three-position surgeries paved the way for severe deformity correction necessitating open posterior access; however, patient repositioning and the increased time under general anesthesia also lead to the previously described increased morbidity. PTP surgery represents the logical progression in access trajectory and technique advancements; early reports of PTP-based deformity correction highlight its utility.
Below, the authors present two representative deformity cases. Case 4 is a 60-year-old female, with two previous operations, who was referred to people from another institution. She has a remote history of L3-4 decompressive laminectomies and, most recently, L3-S1 TLIF 3 years prior to presentation. She presented complaining of severe low back pain with radiation to both thighs anterolaterally. Her imaging was notable for L2-3 ASD, anterolisthesis, and positive sagittal imbalance with a PI-LL mismatch—flat-back deformity.
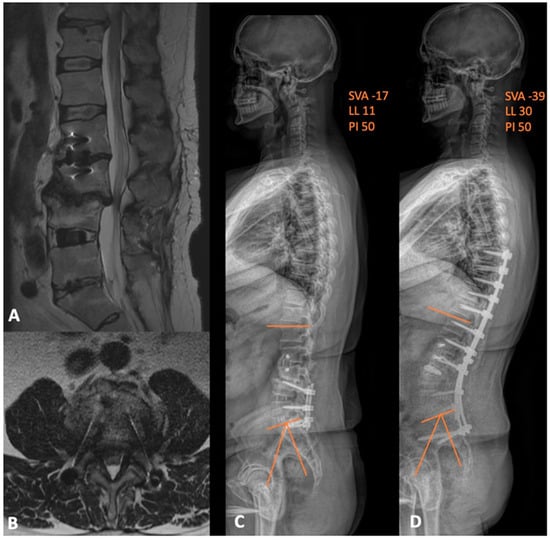
Case 5 is a 53-year-old male who was also referred to institution with prior history of L4-S1 fusion and standalone L2-3 lateral interbody fusion at another institution. He was wheelchair-bound and complaining of severe lower back and left-sided leg pain that radiated to his foot. Prior to presentation, he exhausted all conservative options without symptomatic improvement. His new imaging showed central canal stenosis with severe, diffuse disc bulge, degenerative facet changes, and posterior subluxation of L3 on L4 with significant PI-LL mismatch. He also had evidence of thoracic stenosis, which was worst at T9-T10 and T10-T11. Researchers proceeded with L3-4 PTP, L3-4 PCO, L4 PSO, and an extension of fusion from the T8-pelvis with thoracic decompression. The patient did well after surgery, with significant improvements in his preoperative symptoms and adequate correction of his PI-LL mismatch, as shown in Figure 3. Three months postoperatively, he began ambulating without assistance. This case is an excellent example of how single position surgery not only allows for maximized deformity corrections, but also facilitates other surgical goals, such as direct decompression.
Figure 3. (A) sagittal and (B) axial MRI views depicting the adjacent segment disease at L3-4 level with resultant severe central and lateral-recess stenosis. (C) preoperative and (D) postoperative whole-spine films demonstrating the improvement in both the global lumbar lordosis and PI-LL mismatch. SVA = sagittal vertical axis; LL = lumbar lordosis; PI = pelvic incidence.
3.2. Anterior Column Realignment
Traditional techniques to correct sagittal plane deformities include osteotomies, which require open posterior access. More recently, an anterior column, minimally invasive approach was developed, with demonstrated success in correcting sagittal plane misalignment by sectioning the anterior longitudinal ligament and placing a hyperlordotic cage, with anterior column realignment. Lateral minimally invasive anterior column realignment has repeatedly demonstrated superiority compared to traditional posterior osteotomy with respect to blood loss while maintaining a similar overall complication rate
[21][22][23]. In the case of severe, sagittal, plane fixed deformities, however, minimally invasive lateral ACR is not as effective as open posterior surgery. Combining the two methods in a hybrid approach can maximize their benefits—pedicle subtraction osteotomy optimizes achievable segmental lordosis at the adjacent ACR level
[24]. Further, anterior support via interbody cage placement provides support for PSO by providing a significant reduction in rod stress; the effect is amplified with additional cage placements
[25].
In cadaveric and clinical feasibility studies, this hybrid surgery resulted in a stepwise increase in lordotic correction, greater than that achieved by either procedure alone; however, these procedures were performed on separate days, depending on the length of the ACR
[24]. Here, PTP provides the key advantage of eliminating the requirement for multi-stage surgery and the morbidity associated with the previously described decreased surgical efficiency.
These ACR-PSO hybrid surgeries are not without inherent drawbacks, and prone surgery is not without limitations in the case of ACR. One underreported and feared complication, with an unknown precise incidence, is great vessel violation. In these circumstances, the patient must be flipped supine or rotated to a lateral decubitus position to extend the skin incision for vascular repair. As previously described, some patients have a lumbar-vascular anatomy that is favorably augmented by the prone position. In these patients, perhaps the advantages afforded by the prone position, anatomic and surgical duration balance the risk of major vascular injury—appropriate patient selection is paramount.
3.3. Corpectomy
Vertebral corpectomy is a powerful surgical technique that may be deployed to treat complex pathologies, including traumatic spinal cord injury, cancer, infection, and wide-ranging deformity corrections. Pathology and surgeon preference dictate access, either posterior, anterior, or lateral, each with its respective advantages and disadvantages. The posterior approach offers a familiar route to spinal surgeons while the anterior approach provides superior direct visualization of the ventral spinal elements
[26]. Combining the benefits from the anterior and posterior approaches, the lateral approach, traditionally in the lateral decubitus position, offers access to the anterior and lateral columns without damaging posterior musculature or requiring an access surgeon to navigate the peritoneal vasculature
[26]. Less studied, however, are corpectomies via PTP. This novel approach combines the advantages of the above access trajectories while additionally gaining the lordotic anatomic advantages imparted by the prone position.
In complex corpectomy cases requiring complete circumferential access to the anterior and posterior columns, the PTP approach has recently demonstrated its utility in several case studies. Gandhi et al. described two corpectomy cases necessitating simultaneous lateral and posterior access to the spinal column
[27]. Specifically, Gandhi and colleagues elected this approach to perform the more extensive decompression allowed in the prone position while maintaining the ability to manipulate the anterior column through lateral access
[27].
3.4. Oncology
In the case of oncologic resections, the larger safe zone imparted by both gravitational forces and the ability to extend the hips may theoretically allow for more tissue-sparing resections due to the better and more direct visualization of cancerous masses. Gandhi et al. described a case of a solitary plasmacytoma requiring aggressive local control and spinal column height restoration
[27]. Here, a PTP approach facilitated simultaneous posterior and lateral access for resection, direct posterior decompression, and the larger lateral interbody placement allowed via transpsoas access.
3.5. Pseudoarthrosis and Implant Retrieval.
Pseudoarthrosis, like ASD, is a well-described morbidity of arthrodesis. Traditionally, pseudoarthrosis is treated with a different surgical approach than the index procedure and with the addition of other materials such as bone grafts and instrumentation. The use of interbody devices in pseudoarthrosis correction has shown higher fusion rates, approaching 100%, in circumferential surgeries where an interbody is placed laterally or anteriorly, and instruments are exchanged or placed posteriorly
[28][29][30]. In such cases, where two-stage surgery has demonstrated superiority, the advantage imparted by PTP is clear; the patient and operating room staff may avoid the unnecessary repositioning procedures. Lastly, in these cases, which frequently require instrument exchange, the simultaneous dual access to the spinal column may be advantageous. A failed implant may be exchanged by simultaneous posterior manipulation and lateral retrieval. There is no description of such in the literature; however, simultaneous posterior and anterior column access may be advantageous in the appropriate clinical context and adapted for various scenarios.
This entry is adapted from the peer-reviewed paper 10.3390/jcm13041112