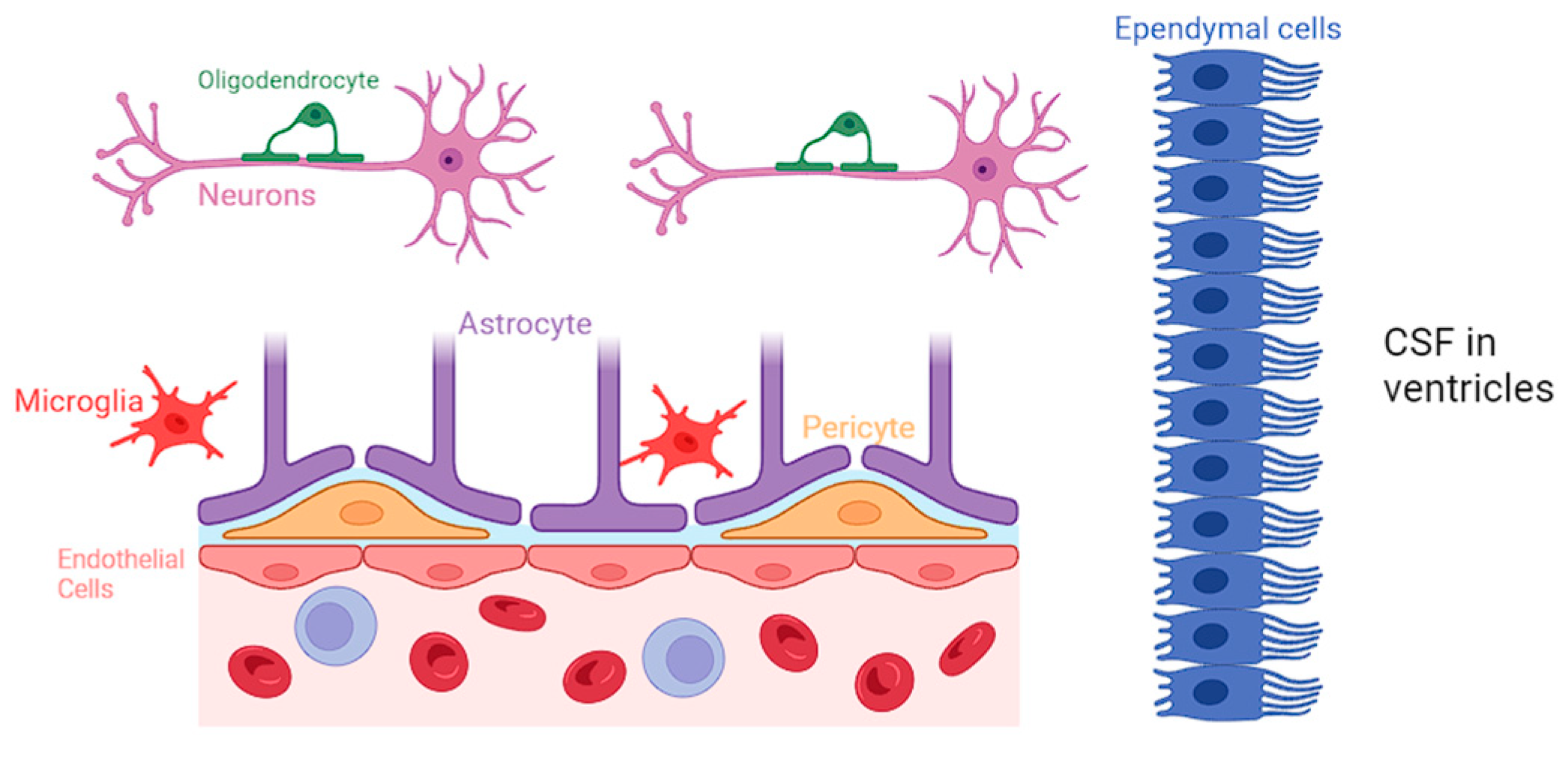
Dysfunction of the neuroglia can have profound consequences on the blood–brain barrier (BBB). Studies have shown that the disruption of astrocytic–endothelial interaction can compromise the permeability of BBB and its effectiveness in selectively regulating the exchange of substances. Microglia have been recognized to have a significant role in the initiation of chronic pain and in its interactions with various nerve blockers and anesthetic agents. Microglia have a role in pain resolution via a pathway that involves Cannabinoid receptor type 2 activation and MAP kinase phosphorylation.
- neuroglia
- blood–brain barrier
- MAP kinase phosphorylation
- chronic pain
1. Introduction
2. Pathophysiology of Pain
3. Introduction to Various Nerve Blockers Used in Anesthesia
|
Procedure |
Mechanism |
Indication |
Side Effects |
Reference |
|---|---|---|---|---|
|
Celiac plexus block (CPB) |
Targets visceral afferent pain fibers from the liver, gallbladder, omentum, pancreas, mesentery, and stomach to the mid-transverse colon |
Pain secondary to pancreatic cancer, chronic pancreatitis, and intractable abdominal pain |
Transient or persistent diarrhea, paraplegia (anterior spinal artery syndrome), postural hypotension, pneumothorax |
|
|
Epidural nerve block |
Injected anesthetic in the epidural space temporarily numbs spinal nerves, blocking pain signals from spinal cord levels |
Surgical procedures: pelvic fractures, cesarean delivery, labor analgesia, hepatic, gastric, and colonic surgeries Nonsurgical: myasthenia gravis, malignant hyperthermia, hyperreflexia |
Hypotension, nausea, vomiting, post-puncture headache after dural perforation. [9] Incidence of transient paralysis is 0.1%; that of permanent paralysis is 0.02% [10]. Paresthesia with or without motor weakness, epidural hematoma, abscess, hypoalgesia of lower extremities |
|
|
Genicular nerve block (GNB) |
Anesthetizes sensory nerve terminal branches of genicular arteries or at the junction of the epiphysis and diaphysis of the femur and tibia, sparing motor function |
Chronic knee osteoarthritis, post-operative knee pain, total knee arthroplasty, alternative to femoral, fascia iliaca, and adductor canal nerve blocks in knee injuries [11] |
Leg muscle weakness, dizziness, and discomfort at injection site |
|
|
Intercostal nerve block (ICNB) |
Anesthetic injection to intercoastal nerves below each rib |
Rib fracture neuralgia, thoracostomy analgesia, herpes zoster neuralgia, upper abdominal surgery, palliative cancer pain for rib and chest wall tumors |
Self-limited bruising and soreness at the injection site. Serious: bleeding, infection, pneumothorax, nerve damage |
|
|
Lumbar sympathetic nerve block |
Disrupts the nerve supply from the preganglionic neurons exiting the spinal cord via the white rami of the ventral root of spinal nerves L1 to L4 and synapse at the lumbar sympathetic ganglion to the postganglionic neurons innervating the lower extremities |
Sciatica, Complex Regional Pain Syndrome (CPRS), phantom limb pain, and lower limb painful ischemia |
Flushing of skin, bleeding, bruising, soreness at the injection site, headache, and leg weakness on ipsilateral injection. Serious: infection, visceral injury, Horner’s syndrome |
|
|
Occipital nerve block |
C2 sensory neurons of the greater occipital nerve create a nociceptive pathway with the trigeminal nucleus caudalis, relieving compression and nerve irritation when targeted with an anesthetic |
Occipital neuralgia, chronic intractable migraine, and cervicogenic and cluster headache treatment alternative in elderly and pregnant populations |
Dizziness, vertigo, numbness, lightheadedness, vasovagal syncope, facial edema, and alopecia at injection if administered with steroid |
|
|
Pudendal nerve block |
Transcutaneous (perineal) or transvaginal approach targets the pudendal nerve trunk and its sensorimotor innervation |
Pudendal neuralgia, obstetric (e.g., second stage of vaginal birth, vaginal repairs, hemorrhoidectomy), and urologic procedures (e.g.,transrectal ultrasound-guided prostate biopsy, transurethral prostatectomy) |
Discomfort at the injection site, serious side effect of bladder and rectum structural injury, and pudendal artery puncture infection |
|
|
Stellate ganglion block |
Interrupts signals to the cervical sympathetic chain and postganglionic fibers for sympathetic innervation of upper limbs |
CRPS of head and upper limbs, peripheral vascular disease, chronic post-surgical pain, postherpetic neuralgia, orofacial pain, scleroderma |
Temporary pain, eyelid droopiness, fever, local blood aspiration, hematoma formation, spondylitis, and rare convulsions |
|
|
Trigeminal nerve block |
The ophthalmic (V1), maxillary (V2), and mandibular (V3) divisions and their corresponding nerves are blocked |
Trigeminal neuralgia, pre-emptive analgesia in maxillofacial surgery |
Difficulty chewing and swallowing and transient facial weakness and numbness |
This entry is adapted from the peer-reviewed paper 10.3390/neuroglia5010002
References
- Gawdi, R.; Shumway, K.R.; Emmady, P.D. Physiology, Blood Brain Barrier. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Obermeier, B.; Verma, A.; Ransohoff, R.M. The blood-brain barrier. Handb. Clin. Neurol. 2016, 133, 39–59.
- Cichorek, M.; Kowiański, P.; Lietzau, G.; Lasek, J.; Moryś, J. Neuroglia-development and role in physiological and pathophysiological processes. Folia Morphol. 2021, 80, 766–775.
- Cekanaviciute, E.; Buckwalter, M.S. Astrocytes: Integrative Regulators of Neuroinflammation in Stroke and Other Neurological Diseases. Neurother. J. Am. Soc. Exp. NeuroTherapeutics 2016, 13, 685–701.
- Wang, D.D.; Bordey, A. The astrocyte odyssey. Prog. Neurobiol. 2008, 86, 342–367.
- Daneman, R.; Prat, A. The blood-brain barrier. Cold Spring Harb. Perspect. Biol. 2015, 7, a020412.
- Abbott, N.J.; Patabendige, A.A.; Dolman, D.E.; Yusof, S.R.; Begley, D.J. Structure and function of the blood-brain barrier. Neurobiol. Dis. 2010, 37, 13–25.
- Cabezas, R.; Avila, M.; Gonzalez, J.; El-Bachá, R.S.; Báez, E.; García-Segura, L.M.; Jurado Coronel, J.C.; Capani, F.; Cardona-Gomez, G.P.; Barreto, G.E. Astrocytic modulation of blood brain barrier: Perspectives on Parkinson’s disease. Front. Cell. Neurosci. 2014, 8, 211.
- Rochfort, K.D.; Cummins, P.M. The blood-brain barrier endothelium: A target for pro-inflammatory cytokines. Biochem. Soc. Trans. 2015, 43, 702–706.
- Ronaldson, P.T.; Davis, T.P. Regulation of blood-brain barrier integrity by microglia in health and disease: A therapeutic opportunity. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2020, 40 (Suppl. S1), S6–S24.
- Gullotta, G.S.; Costantino, G.; Sortino, M.A.; Spampinato, S.F. Microglia and the Blood-Brain Barrier: An External Player in Acute and Chronic Neuroinflammatory Conditions. Int. J. Mol. Sci. 2023, 24, 9144.
- da Fonseca, A.C.; Matias, D.; Garcia, C.; Amaral, R.; Geraldo, L.H.; Freitas, C.; Lima, F.R. The impact of microglial activation on blood-brain barrier in brain diseases. Front. Cell. Neurosci. 2014, 8, 362.
- Simons, M.; Nave, K.A. Oligodendrocytes: Myelination and Axonal Support. Cold Spring Harb. Perspect. Biol. 2015, 8, a020479.
- Seo, J.H.; Maki, T.; Maeda, M.; Miyamoto, N.; Liang, A.C.; Hayakawa, K.; Pham, L.D.; Suwa, F.; Taguchi, A.; Matsuyama, T.; et al. Oligodendrocyte precursor cells support blood-brain barrier integrity via TGF-β signaling. PLoS ONE 2014, 9, e103174.
- Obermeier, B.; Daneman, R.; Ransohoff, R.M. Development, maintenance and disruption of the blood-brain barrier. Nat. Med. 2013, 19, 1584–1596.
- Attwell, D.; Mishra, A.; Hall, C.N.; O’Farrell, F.M.; Dalkara, T. What is a pericyte? J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2016, 36, 451–455.
- Jäkel, S.; Dimou, L. Glial Cells and Their Function in the Adult Brain: A Journey through the History of Their Ablation. Front. Cell. Neurosci. 2017, 11, 24.
- Stapor, P.C.; Sweat, R.S.; Dashti, D.C.; Betancourt, A.M.; Murfee, W.L. Pericyte dynamics during angiogenesis: New insights from new identities. J. Vasc. Res. 2014, 51, 163–174.
- Gaceb, A.; Özen, I.; Padel, T.; Barbariga, M.; Paul, G. Pericytes secrete pro-regenerative molecules in response to platelet-derived growth factor-BB. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2018, 38, 45–57.
- Brown, L.S.; Foster, C.G.; Courtney, J.M.; King, N.E.; Howells, D.W.; Sutherland, B.A. Pericytes and Neurovascular Function in the Healthy and Diseased Brain. Front. Cell. Neurosci. 2019, 13, 282.
- Sonar, S.A.; Lal, G. Blood-brain barrier and its function during inflammation and autoimmunity. J. Leukoc. Biol. 2018, 103, 839–853.
- De Ridder, D.; Adhia, D.; Vanneste, S. The anatomy of pain and suffering in the brain and its clinical implications. Neurosci. Biobehav. Rev. 2021, 130, 125–146.
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097.
- Thanh, N.X.; Tanguay, R.L.; Manhas, K.J.P.; Kania-Richmond, A.; Kashuba, S.; Geyer, T.; Pereira, J.X.; Wasylak, T. Economic burden of chronic pain in Alberta, Canada. PLoS ONE 2022, 17, e0272638.
- Yong, R.J.; Mullins, P.M.; Bhattacharyya, N. Prevalence of chronic pain among adults in the United States. Pain 2022, 163, e328–e332.
- Maniadakis, N.; Gray, A. The economic burden of back pain in the UK. Pain 2000, 84, 95–103.
- Dubin, A.E.; Patapoutian, A. Nociceptors: The sensors of the pain pathway. J. Clin. Investig. 2010, 120, 3760–3772.
- Lacroix-Fralish, M.L.; Mogil, J.S. Progress in genetic studies of pain and analgesia. Annu. Rev. Pharmacol. Toxicol. 2009, 49, 97–121.
- Stewart, J.W.; Dickson, D.; Van Hal, M.; Aryeetey, L.; Sunna, M.; Schulz, C.; Alexander, J.C.; Gasanova, I.; Joshi, G.P. Ultrasound-guided erector spinae plane blocks for pain management after open lumbar laminectomy. Eur. Spine J. 2023. Correction in Eur. Spine J. 2023.
- Mehlmann, F.M.G.; Ferraro, L.H.C.; Sousa, P.C.C.B.D.; Cunha, G.P.; Bergamaschi, E.C.Q.A.; Takeda, A. Ultrasound-guided selective nerve blocks for trigger finger surgeries to maintain flexion/extension of fingers-Case series. Braz. J. Anesthesiol. 2019, 69, 104–108.
- Curatolo, M.; Bogduk, N. Diagnostic blocks for chronic pain. Scand. J. Pain. 2010, 1, 186–192.
- Piraccini, E.; Munakomi, S.; Chang, K.V. Stellate Ganglion Blocks. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK507798/ (accessed on 24 December 2023).
- Bogduk, N. On diagnostic blocks for lumbar zygapophysial joint pain. F1000 Med. Rep. 2010, 2, 57.
- Gupta, R.; Madanat, L.; Jindal, V.; Gaikazian, S. Celiac Plexus Block Complications: A Case Report and Review of the Literature. J. Palliat. Med. 2021, 24, 1409–1412.
- Erdine, S. Complications of Splanchnic and Celiac Plexus Block. In Complications of Pain-Relieving Procedures; Erdine, S., Staats, P.S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2022.
- John, R.S.; Dixon, B.; Shienbaum, R. Celiac Plexus Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK531469/ (accessed on 24 December 2023).
- Avila Hernandez, A.N.; Singh, P. Epidural Anesthesia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK542219/ (accessed on 24 December 2023).
- Kompoliti, K.; Horn, S.S. Chapter 55—Drug-Induced and Iatrogenic Neurological Disorders. In Textbook of Clinical Neurology, 3rd ed.; Goetz, C.G., Ed.; W.B. Saunders: Philadelphia, PA, USA, 2007; pp. 1285–1318.
- Bhattaram, S.; Shinde, V.S. Novel use of motor-sparing genicular nerve blocks for knee injuries in the emergency department. Am. J. Emerg. Med. 2024, 75, 196.e1–196.e4.
- Dass, R.M.; Kim, E.; Kim, H.K.; Lee, J.Y.; Lee, H.J.; Rhee, S.J. Alcohol neurolysis of genicular nerve for chronic knee pain. Korean J. Pain. 2019, 32, 223–227.
- Kim, D.H.; Choi, S.S.; Yoon, S.H.; So-Hee, L.; Seo, D.K.; Lee, I.G.; Woo-Jong, C.; Jin-Woo, S. Ultrasound-Guided Genicular Nerve Block for Knee Osteoarthritis: A Double-Blind, Randomized Controlled Trial of Local Anesthetic Alone or in Combination with Corticosteroid. Pain Physician 2018, 21, 41–52.
- Baxter, C.S.; Singh, A.; Ajib, F.A.; Fitzgerald, B.M. Intercostal Nerve Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK482273/ (accessed on 24 December 2023).
- Guerra-Londono, C.E.; Privorotskiy, A.; Cozowicz, C.; Hicklen, R.S.; Memtsoudis, S.G.; Mariano, E.R.; Cata, J.P. Assessment of Intercostal Nerve Block Analgesia for Thoracic Surgery: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2133394.
- Alexander, C.E.; De Jesus, O.; Varacallo, M. Lumbar Sympathetic Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK431107/ (accessed on 24 December 2023).
- Carroll, I.; Clark, J.D.; Mackey, S. Sympathetic block with botulinum toxin to treat complex regional pain syndrome. Ann. Neurol. 2009, 65, 348–351.
- Barreto Junior, E.P.S.; Nascimento, J.D.S.; Castro, A.P.C.R. Neurolytic block of the lumbar sympathetic chain improves chronic pain in a patient with critical lower limb ischemia. Braz. J. Anesthesiol. 2018, 68, 100–103.
- Austin, M.; Hinson, M.R. Occipital Nerve Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK580523/ (accessed on 24 December 2023).
- Castillo-Álvarez, F.; Hernando de la Bárcena, I.; Marzo-Sola, M.E. Greater occipital nerve block in the treatment of headaches. Review of evidence. Med. Clín. (Engl. Ed.) 2023, 161, 113–118.
- Ghanavatian, S.; Leslie, S.W.; Derian, A. Pudendal Nerve Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK551518/ (accessed on 24 December 2023).
- Cok, O.Y.; Eker, H.E.; Cok, T.; Akin, S.; Aribogan, A.; Arslan, G. Transsacral S2-S4 Nerve Block For Vaginal Pain Due To Pudendal Neuralgia. J. Minim. Invasive Gynecol. 2011, 18, 401–404.
- Goel, V.; Patwardhan, A.M.; Ibrahim, M.; Howe, C.L.; Schultz, D.M.; Shankar, H. Complications associated with stellate ganglion nerve block: A systematic review. Reg. Anesth. Pain Med. 2019.
- Jeon, Y. Therapeutic potential of stellate ganglion block in orofacial pain: A mini-review. J. Dent. Anesth. Pain Med. 2016, 16, 159–163.
- Jacques, N.; Karoutsos, S.; Marais, L.; Nathan-Denizot, N. Quality of life after trigeminal nerve block in refractory trigeminal neuralgia: A retrospective cohort study and literature review. J. Int. Med. Res. 2022, 50, 3000605221132027.
- Kumar, A.; Sinha, C.; Kumar, A.; Kumari, P.; Mukul, S.K. Ultrasound-guided trigeminal nerve block and its comparison with conventional analgesics in patients undergoing faciomaxillary surgery: Randomised control trial. Indian J. Anaesth. 2018, 62, 871–875.
