Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
A holistic view should be taken towards patient’s treatment, care and counselling in order to provide patient-centric, ethically and legally informed care for pregnant cancer patients. It is essential to consider individual circumstances of each pregnant cancer patient where each patient is seen as a person embedded in the realities of their lives and the changes that a cancer diagnosis brings to themselves and their pregnancy care.
- cancer during pregnancy
- ethics
- guidelines
- patient centricity
- patient engagement
1. Introduction
Providing care to pregnant cancer patients is complex as they present healthcare needs and decisional dilemmas that encompass distinct and often overlapping dimensions [1]. Looking after these patients raises not only clinical challenges, such as choosing the most suitable treatment regiment, time of delivery and breastfeeding support following the birth of an infant, but also many concerns and decisional challenges for the patients [2] and ethical challenges for the clinical teams [3].
Treatment choices are challenging as the evidence derived from prospective clinical trials is scarce due to study design and participant recruitment difficulties in this setting. Even though it is known that pregnancy does not impair the clinical outcomes of patients who have undergone curative treatment for some cancers [4,5], less data are available regarding its impact on those with advanced cancers which require multimodal treatment protocols [1,6]. Moreover, some cancers might be more difficult to manage during pregnancy and some treatments may be not feasible during pregnancy. For example, uterine cancer poses the challenge that the organ affected by cancer is also the one bearing the pregnancy [7,8] and chemotherapy given during the first trimester may be associated with a higher rate of foetal malformations and pregnancy complications [9]. Therefore, treatment decisions always need to be informed by the gestational age of the foetus as well as the site, stage and biological features of the tumour (Table 1). Recent recommendations suggest that radiotherapy is technically feasible during pregnancy, specifically for tumours that are remote to the foetus, such as breast and head and neck cancer [10]. Immunotherapies and targeted agents are usually contraindicated in pregnancy with some reports of congenital hypothyroidism [11] or severe immune-mediated enteritis [12] following in utero exposure to anti-PD1. On the contrary, other reports present positive maternal outcomes after immunotherapy exposure [13,14,15]. Further reviews also suggest that targeted therapies (e.g., trastuzumab) in the first trimester are less likely to lead to complications [16], and their use during pregnancy might be possible under close monitoring [17], but the risk of pregnancy and foetal complications remains high [18]. Thus, standard treatments cannot be always given to pregnant cancer patients, reinforcing the difficulty of managing such patients.
Table 1. Considerations for treating cancer during pregnancy.
| Type of Malignancy | Modes of Treatment | Considerations for Pregnant Patients | Considerations for the Foetus |
|---|---|---|---|
| Breast cancer [19,20] | Surgery (safe throughout pregnancy), radiotherapy (contraindicated in pregnancy), chemotherapy (second and third trimester), hormonal/endocrine therapy (contraindicated), immunotherapy (contraindicated, PD-1/PD-L1 pathway could result in immune response against the foetus), targeted therapy (contraindicated with exception of trastuzumab, which may be used in the first trimester under close monitoring). | Physiological breast changes should be considered, delaying reconstruction surgery after delivery. Higher risk of pregnancy complication cannot be excluded. |
Increased risks of stillbirths, small gestational weight, preterm delivery, neonatal mortality. No significant impairment after exposure to chemotherapy. Prematurity correlated with worse cognitive outcome irrespective of cancer treatment. |
| Thyroid cancer [21,22] | Surgery (second trimester or after delivery), endocrine therapy (LT4 therapy should start immediately after surgery), radioactive iodine (contraindicated in pregnancy and breastfeeding), immunotherapy with tyrosine kinase inhibitors (TKIs) is not well studied. | Calcium and vitamin D supplementation, hypothyroidism should be avoided by correct supplementation of thyroxine. No evidence to support pregnancy termination. |
Thyroid hormone deficiency can cause severe neurological disorders. |
| Cervical cancer [7,23,24] | Hysterectomy (in advanced cases, can be combined with a caesarean delivery or performed post-partum, otherwise not compatible with pregnancy), cold knife conization (risk of premature birth), radical trachelectomy/cervicectomy (risk of premature birth), chemotherapy (second and third trimester), radiotherapy (contraindicated). | Caesarean section is preferred delivery method, especially in advanced cases. Fertility preservation in advanced cases might not be possible. Chemotherapy is not recommended beyond 35 weeks of gestation to allow maternal and foetal bone marrow recovery before delivery. |
Chemotherapy can affect foetal eyes, genitals, hematopoietic system, nervous system, foetal growth. Single cases of bilateral hearing loss and rhabdomyosarcoma have been reported. |
| Other gynaecological cancers (vulvar, vaginal, endometrial, ovarian cancer, ovarian masses with low malignant potential) [7] | Laparoscopic surgery (feasible throughout pregnancy, not longer than 90–120 min), surgery (decided upon individual cases), chemotherapy (second and third trimester), radiotherapy (contraindicated), systemic therapies not well studied. | Caesarean section is a preferred delivery method, especially in advanced cases. In cases of advanced epithelial ovarian cancer, pregnancy termination should be considered in the first half of pregnancy. Chemotherapy is not recommended beyond 35 weeks of gestation to allow maternal and foetal bone marrow recovery before delivery. |
If possible, delivery should not be induced before 37 weeks to allow foetal maturity. Breastfeeding should be avoided with ongoing chemotherapeutic, endocrine and targeted treatment. |
| Lymphomas (Hodgkin lymphoma and non-Hodgkin lymphoma) [25,26] | Chemotherapy (second and third trimester), radiotherapy (conflicting data), immunotherapy (limited data) | Deferring therapy until after delivery does not always affect maternal outcomes and can be considered. Pregnancy termination can be considered in the first trimester. Patients receiving antenatal therapy have more obstetric complications (preterm contractions and preterm rupture of membranes). |
No gross foetal malformations or anomalies have been reported. Low gestational age and admissions to NICU did not differ between neonates exposed and not exposed to chemotherapy. Those exposed to chemotherapy had lower birth weight. |
| Melanoma [27,28] | Excisions (throughout pregnancy—safe and necessary), targeted therapies (BRAF inhibitors) and checkpoint inhibitors (anti-PD1 and anti-CTLA4) may be teratogenic. | Relationship between pregnancy and melanoma should not be ruled out. Some reports suggest poorer prognosis for pregnant patients, but evidence is inconclusive. | No evidence that melanoma diagnosis will have adverse effected on the foetus. Melanoma accounts for 30% of metastatic spread to the placenta. This does not mean that the foetus will be affected. |
| Brain tumours [29,30] | Surgery, chemotherapy, radiotherapy—only limited data available due to rarity of the condition. | Delivery recommended after 34 weeks of gestation to allow foetal maturity. Caesarean delivery recommended. |
No known foetal complications. Steroids for foetal lung maturation might be needed if early delivery is needed due to deteriorating maternal condition. |
| Lung cancer [31,32] | Chemotherapy (second and third trimester), targeted therapies—only limited data available due to rarity of the condition | Increased risk of lung infections. Case reports suggest that lung cancer is diagnosed at advanced stages in pregnancy and prognosis is poor. | No adverse outcomes data reported. Due to advanced stage of maternal cancer, there might be a metastatic spread to the placenta. This does not mean that the foetus will be affected. |
The decision-making process in this setting is also challenging for patients and often raises ethical dilemmas. Patients might need support with attending hospital appointments and enduring treatment procedures, while at the same time preparing for the arrival of the new family member and taking care of an infant. An extra layer of complexity stems from the idiosyncratic nature of this condition, as the patient herself is not the only player involved or affected (Figure 1). Ethical questions raised by the healthcare team, patients and/or their families are not always the same and might be conflicting, such as when one party does not feel comfortable with care decisions that are either taken or desired by another party involved [33,34]. For these reasons, taking care of pregnant cancer patients requires a multidisciplinary clinical team that should also include decisional counsellors [35,36], psychologists and ethicists [37], in addition to the oncological core medical team [1,38,39,40].
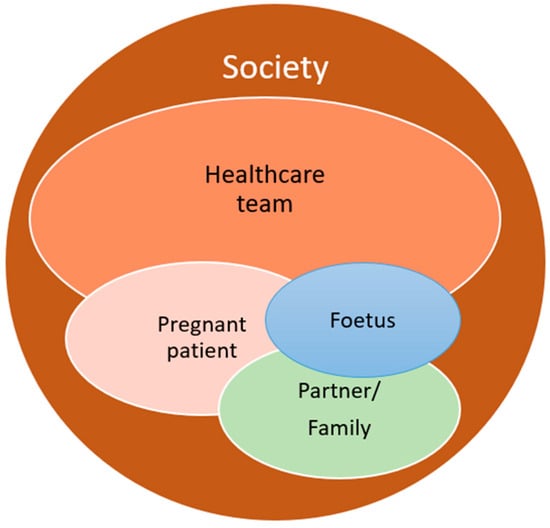
Figure 1. Conflicting interests in cancer during pregnancy care. The bubble sizes and colours in the above figure are not intended to rank the importance of the affected stakeholders.
To provide patient-centric, ethically and legally informed care for pregnant cancer patients, a holistic view should be taken towards patient’s treatment, care and counselling. It is essential to consider individual circumstances of each pregnant cancer patient where each patient is seen as a person embedded in the realities of their lives and the changes that a cancer diagnosis brings to themselves and their pregnancy care. Currently, only limited ethical guidance is available for clinicians with very few resources presented in a structured and consistent manner [39,41], lacking guidelines dedicated to identifying, addressing and managing ethical issues and concerns in cancer during pregnancy care. Available resources integrate information from the guidelines focused on clinical aspects of treating different cancer types during pregnancy and are supplemented by some clinical and bioethics experts’ input. This guidance is also mostly based on references to the biomedical ethics principles, which is a significant limitation of ethical guidance available in this field.
2. Ethical Models Applicable to Cancer Care during Pregnancy
There are many ethical guidance models that can be applied to cancer care during pregnancy. However, none of them appear to adequately address all ethical issues arising in these circumstances. Four biomedical ethics principles developed by Beauchamp and Childress [42] and the European principles in bioethics and biolaw [43,44] were used as a starting point (Table 2).
Since caring for pregnant cancer patients also requires consideration of the patient’s relationships—including the patient’s perceived relationship with the foetus, partner, other children (if present), parents, relatives, friends and wider community, as well as ethno-socio-cultural and political environment [34]—elements of ethics of care [45,46], relational ethics [47,48] and medical maternalism [49,50] were also considered. These relational, patient-focused approaches were used as adjuncts to specify the principles-based guidance and to illustrate how the proposed theoretical framework (Figure 2) and subsequent ethics checklist (Table 3) can work in already existing healthcare structures by supplementing rather than challenging already established patient care processes and services.
Table 2. Foundational models for ethical, patient-centric care of pregnant cancer patients.
| Ethical Models Used to Develop the Guidance | Model Description and Specification | Key References | |
|---|---|---|---|
| Principle-based approaches | Four principles for biomedical ethics (Georgetown principles) by Beauchamp and Childress | Respect to patient’s autonomy, including relational aspects Nonmaleficence: avoiding harm before doing good Beneficence: maximising the benefit for the pregnant patient and developing foetus Justice: considering a big picture and a broader context |
[42] |
| European principles of bioethics and biolaw presented by Rendtorff | Autonomy: individual freedom to make choices Dignity: moral responsibility to human life Integrity: right to bodily integrity, right to refuse treatment Vulnerability (respect to vulnerability): recognising human vulnerabilities, protecting vulnerable groups |
[43,44] | |
| Relational, patient-focused approaches | Relational ethics | Trusted relationship building with the patient Patient-centric approach to patient care Interdependency and freedom Emotions and reason |
[47,48] |
| Care ethics (ethics of care) | Compassion to patient’s suffering Presence in patient’s unique situation, active listening Empathy to patient’s feelings and circumstances Recognition of a patient as fellow human being |
[45,46] | |
| Medical maternalism | Shared decision making Accessible evidence-based information Conversation and understanding of patient’s circumstances and best interest Patient guidance through clinical advice and reason |
[49,50] |
2.1. Principle-Based Approaches
Classical biomedical ethics principles (respect for patient’s autonomy, nonmaleficence, beneficence and justice) developed by Beauchamp and Childress [51], also known as the Georgetown principles, are both directly and indirectly referenced by clinical practice guidelines for cancer treatment during pregnancy [39]. The European approach to biomedical ethics offers autonomy, dignity, integrity and vulnerably as core guiding principles, which are to be considered in the broader context where a patient is seen as being part of a wider human ecosystem [44]. Therefore, respect for patients’ autonomy, which requires due attention to be given to the individual patient’s views and wishes (as well as their participation in decision making) is not limited to the patient alone. Beauchamp and Childress recognise that following the respect for autonomy principle without considering the context is problematic because patients do not live in isolation and out of context. Their treatment choices might affect other people in their lives, and the patient’s choices can also be influenced or even directed by people that pregnant cancer patient considers significant [42].
Therefore, in addition to autonomy, it is suggested that in the European context, dignity should further support the moral responsibility to human life [44], which is perceived broadly. It is not intended to escalate disagreements on how and whether the life of the unborn should be protected. Dignity, together with bodily integrity, overarch classical nonmaleficence and beneficence principles proposed by Beauchamp and Childress. Moreover, vulnerability (or respect for vulnerability) has been emerging as a wider recognised principle in biomedical ethics [52,53], which could be distinguished either as a requirement to protect vulnerable groups [54] or as merging with other principles, such as the principles of nonmaleficence, autonomy, dignity and bodily integrity [55]. Some authors also mention “vulnerability to co-creation”, especially in contexts surrounding the reproductive decisions, parental roles and dependent status of women [56], where their personal identity is mirrored through their relationships with others [57,58].
Principles on their own, however, can be too rational and too rigid for addressing ethical issues in everyday clinical practice [59] as—for example—is the doctrine/rule of double effect referenced by Beauchamp and Childress in regards to maternal–foetal conflict [42]. Maternal–foetal conflict is sometimes presented as deliberate harm to the developing foetus caused by its mother’s ignorance or unwillingness to adhere to standard pregnancy care [60], which is not necessarily the case when cancer is diagnosed during pregnancy. Principles can also fall in a conflict with each other, especially respect for patients’ autonomy and clinicians’ beneficence obligations [51]. Moreover, the principled approach has been shown to be less culturally neutral than it might initially appear, especially in a non-Judeo–Christian context [61]. Therefore, principle-based models need to be supplemented with other ethical models in order to address the ethical and patient-centred care needs. Some attempts have been made to blend principle-based approaches with casuistry when resolving clinical cases [62], which has been shown to be a valuable addition to technological decisional support tools aimed at patient-centred healthcare [63].
2.2. Relational, Patient-Focused Approaches
Shared decision making and care of pregnant cancer patients can be a very intense, emotional and psychologically demanding task for the healthcare team. It might challenge clinical teams’ attitudes towards the patient, their circumstances and even relationship with the patient. Indeed, the pregnant cancer patient’s relationship with the clinical team is of pivotal importance, requiring recognition of the patient’s unique situation; understanding of their individual circumstances; and empathy with their clinical, moral and practical concerns. Relational ethics can support clinicians with a patient-centred approach to patients by guiding the relationships toward empathy, attempting to understand patients’ emotions and reasoning [47].
The ethics of care further specify that compassion, presence, empathy and recognition of a patient as a fellow human being play a significant role in building trusted relationships between healthcare professionals and their patients [64], which is regarded with high importance in midwifery [46].
Medical maternalism is one more patient-focused approach emerging in contemporary bioethics [50]. It considers patients’ autonomy in a relational context and encourages patient support by the clinical team, where patients are provided correct, up-to-date and easy to understand information in order to guide them through the decision-making process with their best interests in mind.
Caring for pregnant cancer patients can have further relational and care obligation complexities. Some healthcare professionals might feel an obligation to protect the developing foetus and might consider it a separate patient [65,66]. Such protection, however, can only be achieved if pregnant patients perceive foetal interests the same way as the clinical team does and are willing to collaborate with the clinicians. Some jurisdictions might have legal frameworks governing pregnancy care and restricting pregnancy termination. A recent example from the United States in the Dobbs vs. Jackson case shows that cancer treatment options might be restricted for pregnant patients [38,67], despite the historic trend denying foetuses a legal entity status until they are born [68].
Relational, patient-focused approaches to patient care can fall short of being universally applicable as they mostly describe the practice of providing care [69]. Such approaches are based on forming trusted relationships with the patient, but they do not offer a clear set of rules to follow which could be applied in different patient care scenarios. Furthermore, some suggest that care ethics and relational approaches to patient care are solely based on Western perceptions of patient care and lack cultural representativeness and inclusiveness [70].
Figure 2. A visual summarising the framework for ethical, patient-centric care of pregnant cancer patients
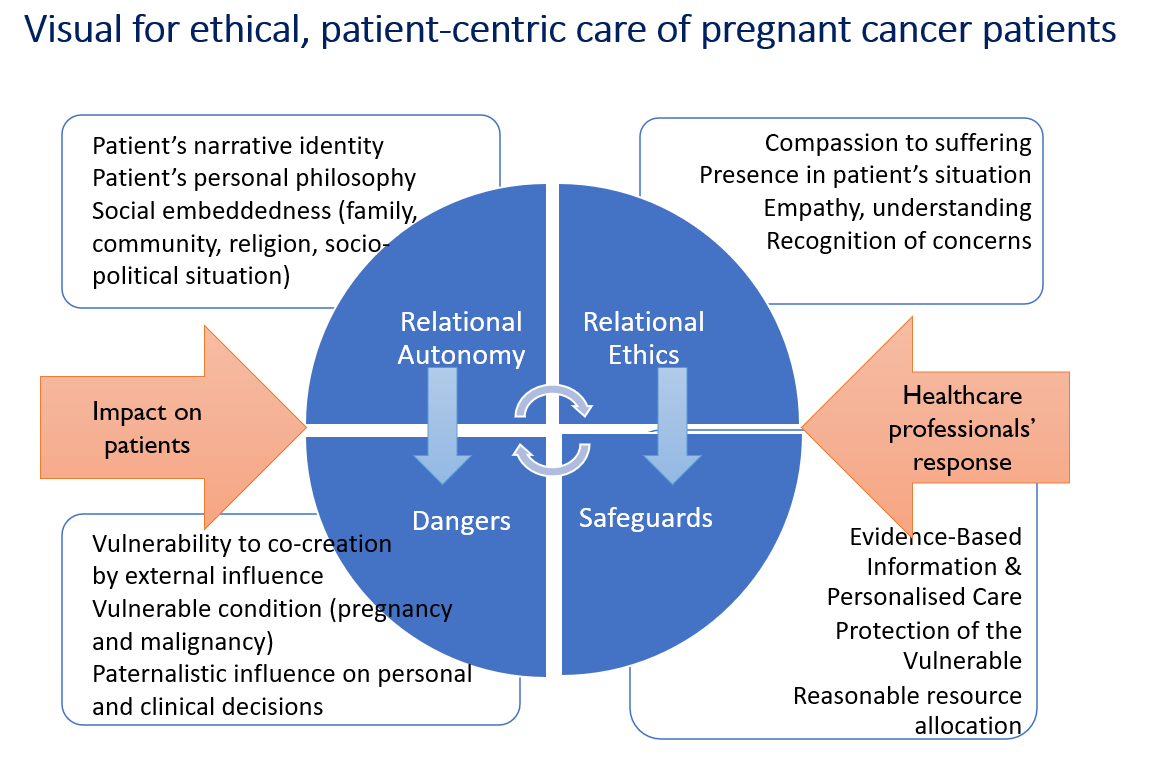
Table 3. Foundational m
This entry is adapted from the peer-reviewed paper 10.3390/cancers16020455
This entry is offline, you can click here to edit this entry!
