You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Recently, in the treatment of advanced esophageal cancer, evidence for combined-modality therapy has been obtained, and the usefulness of neoadjuvant therapy and conversion surgery has been reported. Neoadjuvant therapy is known to improve the results of surgery for advanced esophageal cancer. In particular, neoadjuvant chemoradiotherapy (NACRT) showed a better prognosis than chemotherapy. When a histologically effective response is obtained, the presence of a good response has been shown to significantly affect the resection rate and the long-term prognosis; thus, precise evaluation has become more important for determining the treatment strategy.
- esophageal cancer
- neoadjuvant therapy
- perfusion-CT
- diffusion-MRI
- FDG-PET
1. Introduction
Recently, in the treatment of advanced esophageal cancer, evidence for combined-modality therapy has been obtained, and the usefulness of neoadjuvant therapy [1,2] and conversion surgery has been reported [3,4]. Neoadjuvant therapy is known to improve the results of surgery for advanced esophageal cancer. In particular, neoadjuvant chemoradiotherapy (NACRT) showed a better prognosis than chemotherapy [5,6,7,8]. When a histologically effective response is obtained, the presence of a good response has been shown to significantly affect the resection rate [9] and the long-term prognosis [10,11]; thus, precise evaluation has become more important for determining the treatment strategy.
2. Response Prediction before Neoadjuvant Therapy
A highly detailed prediction of treatment outcome requires evaluation of the physiological or biochemical characteristics of the tumor, which must be considered when selecting the drug delivery system or irradiation conditions. Tumors show angiogenesis with increased VEGF, which can be seen through evaluation of perfusion status, or stromal changes, which can be seen through evaluation of diffusion status [15]. Therefore, qualitative imaging modalities such as perfusion-CT or diffusion-MRI can show the dynamics of blood flow or diffusion of the tumor and surrounding tissue, which are considered useful for the prediction [16,17].
Perfusion analysis: It was thought that the high blood flow presented advantages with respect to pharmacokinetics or oxygenation to obtain a good pathological response. Perfusion-CT is a method that shows tumor tissue hemodynamics [18,19] (Figure 1). The tumor blood flow after CRT and the ◿blood flow could be evaluated using this modality. And the predictive ability of this method has also been reported. The quantity of tumor blood flow before treatment reflects the degree of response. Hayano et al. [20], Makari [21], and Li [22] reported that higher tumor blood flow could be the index for predicting responders. On the other hand, DCE-MRI also provides perfusion images. In the analysis of DCE-MRI, the Ktrans value is used as an index that reflects tissue permeability and blood flow. Lei et al. [23] and Ye et al. [24] reported that the pre-treatment Ktrans value was significantly higher in complete responders and could be a response predictor [25].
Diffusion analysis: Tumors are considered to show trends in their diffusion status due to their microvessels and stromal characteristics [14]. Diffusion-MRI is a method to calculate the diffusion dynamics of tissue through imaging (Figure 2). According to the treatment effect, the apparent diffusion coefficient (ADC) is a quantitative measure of the state of diffusion. ADC value was reported to be inversely correlated to the tissue VEGF expression [14,26] or tumor stromal density [14]. Therefore, it could reflect the drug delivery or radiation circumstance and was expected to be a predictive marker of treatment response [26]. It has been reported in several articles that the diffusion of the tumor before treatment correlates with the degree of response to CRT [24,26,27,28]. Aoyagi et al. [27] described that the susceptibility to treatment could be predicted using this method, with ADC > 1.1 identifying responders, but no consensus was reached regarding the concept and index value for the prediction of response. Li et al. [29] speculated that tumors with high necrosis might have higher ADC values and that they would be associated with poor therapy outcomes. Hirata et al. reported that a high ADC value was related to a lower response [30].
3. Response Evaluation Reflecting the Degree of Pathological Regression after Treatment
In neoadjuvant therapy, when a histologically effective response was obtained, the prognosis after surgery was significantly better [31,32]. Therefore, it becomes essential to assess the degree of response after treatment accurately to determine whether to proceed with surgical resection. Tumor perfusion, diffusion, glucose metabolism, and tissue heterogeneity and their relationships have been found to change according to the histologic response to therapy.
Perfusion analysis: It has been reported that, on perfusion CT, the tumor part shows a significant blood flow decrease with treatment, and the images reflect the histologic response. Significant tumor blood flow decreases were seen in responders to neoadjuvant chemoradiotherapy compared with non-responders (Figure 1), and responders were diagnosed using this index of tumor blood flow decrease. Hayano et al. [33] reported an index of a 15% decrease in tumor blood flow after treatment, which reflected histological response, and Stefanovic et al. reported [34] a post-CRT blood flow < 30 (mL/min/100 g) as a response.
Diffusion analysis: A consensus was seen in several reports that tumor diffusion had been shown to have a tendency to increase after treatment according to the degree of the histologic response (Figure 3), and ◿ADC (pre–post) was a good marker which reflected histologic response [17,35,36,37,38]. In our results obtained via diffusion-weighted imaging with 1.5T-MRI for advanced esophageal cancer during the treatment of CRT, the responder group showed a significant earlier increase in the ADC value at the irradiation dose of 20 Gy than the non-responder group (Figure 3), and it seemed that an evaluation of the early treatment effect would be possible. Moreover, the possibility of its evaluation in the early treatment course was also recommended in several articles [35,37,39]. Imanishi et al. [35] reported that responders to CRT showed an ADC increase of 15% at 20 Gy and 40% at 40 Gy. Guo et al. [28], Vollenbrock et al. [40], and Borggreve [39] reported that the optimal timing for early prediction of the effect was 2 weeks after the beginning of treatment. Vollenbrock et al. [40] described that the ADC increase with treatment effect was due to the early effect of radiotherapy on the tumor microenvironment inducing tumor necrosis with a loss of cell membrane, resulting in an increase in the ADC.
Glucose metabolism analysis: FDG-PET is a technique for imaging the state of glucose metabolism, which reflects tumor proliferative activity, and the degree of glucose integration is assessed with the standardized uptake value (SUV) calculated from an image [41]. Evaluations of the mean uptake of the tumor and of total uptake are possible, and the histologic responses have been reported to correlate with the mean uptake [42,43]. As indices to identify responders, Higuchi et al. [44] reported post-treatment SUV < 2.5, and Swisher et al. [42] reported SUV < 3.1. Furthermore, through evaluation in the early treatment period, a prediction of the final effect was also considered possible. Otto et al. [45] assumed that a 35% decrease in accumulation two weeks after the start of chemotherapy for esophageal adenocarcinoma was a predictor of response. This occurred before the morphologic decrease in the tumor, which was thought to be due to decreased glucose metabolism prior to its morphologic decrease. In addition, the prognostic value of metastatic lymph node uptake after treatment, as well as the main tumor, was reported [46], and Yasuda et al. reported the prognostic value of residual lymph node uptake after treatment [47,48].
Heterogeneity analysis: Tumor heterogeneity has been reported to reflect malignancy or prognosis, and it has been studied through texture analysis using CT. It was reported that tumor texture showed a tendency to homogenize, decrease entropy, and increase uniformity after treatment [49,50,51,52]. When planning for conversion surgery, an evaluation of the heterogeneity of the effect on the tumor is needed to diagnose downstaging. If T4 status could be diagnosed as resolved, conversion surgery with R0 resection could be possible. For such a diagnostic aim, tissue-selective reconstruction of enhanced CT was applied to show the fibrous changes in the tumor due to treatment. In our study, contrast-enhanced CT (100 mL/body/30 s of contrast medium) was performed using multi-detector CT, and a depiction of the layer of connective tissue or adipose tissue between a tumor and adjacent organs was enabled through the contrast-enhanced CT image reconstruction method, which emphasizes the CT values of the tissue (Figure 4). It was found to be useful for the diagnosis of T4 cases. Furthermore, after treatment, the decrease in the CT level of the tumor has been found to correspond to the histologic response. In T4-diagnosed cases before treatment, the presence of a fibrotic change in the tumor and the emergence of a fibrous layer between the tumor and the adjacent organs after treatment have been reported to be evidence of downstaging that would permit conversion surgery with R0 resection [53].
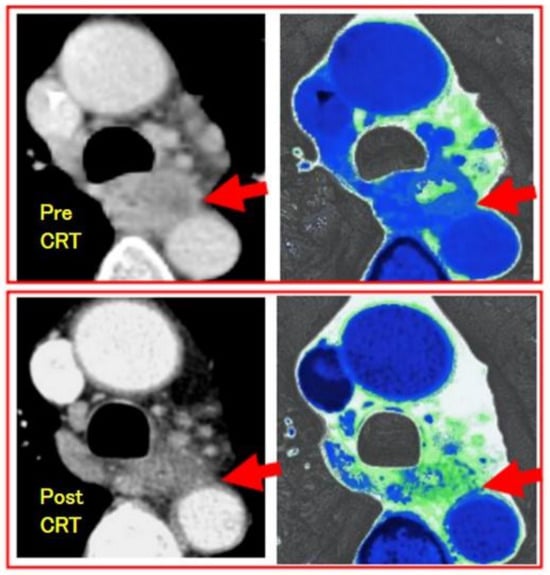
Figure 4. Downstaging evaluation using fibrous-tissue-enhanced CT reconstruction image of the case of esophageal squamous cell carcinoma after CRT. Contrast-enhanced CT was performed using multi-detector CT (GE light speed ultra). Arrows show the tumor. The upper is pre-CRT T4 image, which shows no interstitial plane between the tumor and aorta. The lower is post-CRT image, which shows fibrous plane as green and the case was diagnosed as downstaging and curatively resected with surgery.
This entry is adapted from the peer-reviewed paper 10.3390/jcm13020632
This entry is offline, you can click here to edit this entry!
