Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Dermatology
Keloid is a disease in which fibroblasts abnormally proliferate and synthesize excessive amounts of extracellular matrix, including collagen and fibronectin, during the healing process of skin wounds, causing larger scars that exceed the boundaries of the original wound. Various phenolic compounds, terpenoids, alkaloids, and other plant-derived compounds could modulate different cell signaling pathways associated with the pathogenesis of keloids. For now, many studies are limited to in vitro experiments; additional research and development are needed to proceed to clinical trials.
- keloid
- plant-derived compounds
- phenolic compounds
- terpenoids
- alkaloids
1. Introduction
Keloid is a type of scarring that occurs due to abnormally high cell proliferation and the excessive accumulation of extracellular matrix (ECM) during the healing process of a skin injury [7,8]. Keloids are similar to hypertrophic scars in that they involve the proliferation of dermal fibroblasts and accumulation of ECM, but keloids differ in that they grow beyond the boundaries of the initial injury [9]. In hypertrophic scars, collagen or other ECM components show a wavy or spiral pattern arranged in a specific direction, but, in keloids, ECM does not show a consistent or regular pattern [10]. Additionally, hypertrophic scars gradually become smaller and lessen over time, but keloids are different in that they grow larger or persist [11,12]. Therefore, keloids are sometimes classified as benign fibroproliferative skin tumors [13].
Keloids and hypertrophic scars are both aesthetically disfiguring and functionally defective and can cause pruritus (itchiness), pressure, or pain depending on their shape, size, and location [11,14]. In treating keloids, surgical excision, cryotherapy, radiation, laser treatment, photodynamic therapy, pressure therapy, silicone gel sheeting, and pharmacotherapy are currently used alone or in combinations [15,16,17,18,19]. In pharmacotherapy, steroids, retinoids, interferons, imiquimod, etc. are administered by intralesional injection or topical application [15,16,17,18,19]. However, the outcomes are usually unsatisfactory, and further technical development is needed.
Studies have been conducted extensively to prevent and treat keloids by using various natural products in parallel with the application of various surgical, physical, and pharmacological therapies [15,18]. The following sections present experimental results from studies on the biological activities of plant-derived compounds in KFs at the cellular and molecular level. The compounds are described by classifying them into phenolic compounds, terpenoids, alkaloids, and others. The chemical structure of each compound is shown in Figure 1. The proposed therapeutic targets of plant-derived compounds are summarized in Table 1.
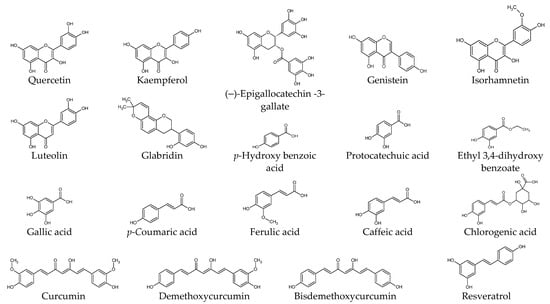
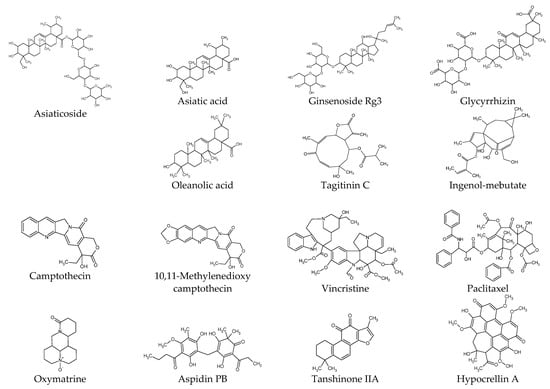
Figure 1. Chemical structures of natural products.
Table 1. Proposed therapeutic targets of plant-derived extracts and compounds. The targets modulated by each compound are indicated by check mark (√).
| Compounds | Proliferation/ Viability |
Migration/ Invasion |
Apoptosis | ECM Production |
TGF-β Level |
TGFβR Level |
SMAD Pathway |
AKT Pathway |
ERK Pathway |
Additional Targets |
Literature |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quercetin | √ | √ | √ | √ | √ | √ | √ | IGF1R | [87,108,109,110,111] | ||
| Kaempferol | √ | [111] | |||||||||
| (–)-Epigallocatechin -3-gallate |
√ | √ | √ | √ | STAT3 | [59,85,107] | |||||
| Genistein | CTGF | [112] | |||||||||
| Luteolin | √ | √ | FRAT1 | [113] | |||||||
| Glabridin | √ | √ | √ | √ | √ | [114] | |||||
| Isorhamnetin | √ | √ | √ | √ | S1PR1 | [74] | |||||
| Protocatechuic acid | √ | √ | [111] | ||||||||
| Gallic acid | √ | √ | [111] | ||||||||
| p-Coumaric acid | √ | [111] | |||||||||
| Ferulic acid | √ | [111] | |||||||||
| Chlorogenic acid | √ | √ | [111] | ||||||||
| Curcumin | √ | √ | √ | √ | [111,115] | ||||||
| Demethoxycurcumin | √ | √ | √ | [115] | |||||||
| Bisdemethoxycurcumin | √ | √ | √ | [115] | |||||||
| Resveratrol | √ | √ | √ | √ | √ | HSP47, α-SMA | [116] | ||||
| Asiaticoside | √ | √ | √ | √ | √ | √ | p38, GDF-9 | [117] | |||
| Asiatic acid | √ | √ | PAI-1, PPARγ | [82,118] | |||||||
| Ginsenoside Rg3 | √ | √ | √ | √ | √ | Angiogenesis | [119] | ||||
| Tagitinin C | √ | √ | [120] | ||||||||
| Ingenol-mebutate | √ | √ | miR-34a | [121] | |||||||
| Glycyrrhizin | √ | √ | √ | √ | √ | √ | √ | NF-κB, HMGB1, Autophagy | [70] | ||
| Oleanolic acid | √ | √ | √ | MMP1 | [122] | ||||||
| Camptothecin | √ | [123] | |||||||||
| 10,11-Methylenedioxy camptothecin |
√ | √ | √ | PAI-1 | [124] | ||||||
| Oxymatrine | √ | √ | [125] | ||||||||
| Vincristine | √ | [24] | |||||||||
| Paclitaxel | √ | √ | √ | √ | √ | [126] | |||||
| Aspidin PB | √ | √ | √ | CTGF | [127] | ||||||
| Tanshinone IIA | √ | √ | Survivin | [128] | |||||||
| Selenium- polysaccharide |
√ | √ | PARP | [129] | |||||||
| Photodynamic therapy with Hypocrellin A | √ | √ | √ | √ | √ | √ | √ | Autophagy, α-SMA |
[130] |
2. Phenolic Compounds
Quercetin attenuated KF proliferation (IC50, 25 μg mL−1) and lowered the expression levels of TGF-β1, TGFβR1/2, collagen 1/3, and fibronectin [87,108,109,110]. It lowered the expression levels of SMAD2/3/4 and reduced the phosphorylation of SMAD2/3, and the formation of the SMAD2/3/4 complex [110]. It lowered the expression levels of the insulin-like growth factor 1 receptor (IGF-1R) β subunit, insulin receptor substrate (IRS) 1, PI3K p85 subunit, c-Raf, and reduced the phosphorylation of c-Raf, MEK1/2, ERK1/2, ETS like protein (ELK) 1, and AKT1 in KFs [108].
(–)-Epigallocatechin-3-gallate (EGCG) attenuated the proliferation, migration, and collagen production of KFs and NFs, and reduced the phosphorylation of STAT3, but not that of SMAD2/3, in KFs [59]. Green tea extract and EGCG lowered the expression level of collagen 1 and reduced the phosphorylation of AKT, eukaryotic translation initiation factor 4E-binding protein (4E-BP), and p70S6K in KFs stimulated by human leukemic mast cell line HMC-1 [107].
CTGF protein levels were higher in KFs compared to NFs, and genistein reduced the CTGF protein levels in KFs [112]. Genistein, at different concentrations (37 or 370 μM), had variable effects on the mRNA expression levels of subunit proteins of AP-1, such as c-Jun, c-Fos, and FosB, in skin keratinocytes, NFs, and KFs [131].
Luteolin decreased the KF viability and the expression levels of cyclin D1, BCL-2, and FRAT1, and increased cell apoptosis, p21, and BAX expression [113]. The pro-apoptotic effects of luteolin were abolished by overexpressed FRAT1, a GSKβ3 inhibitor causing β-catenin activation in the Wnt signaling pathway, and siRNA-mediated FRAT1 depletion increased cell apoptosis [113].
Glabridin, a component of Glycyrrhiza glabra, reduced KF proliferation and collagen production and induced apoptosis by inhibiting the PI3K/AKT and TGF-β1/SMAD signaling pathways in vitro [114].
Isorhamnetin inhibited the proliferation, migration, invasion, and fibrogenesis of KFs [74]. It lowered the expression level of S1PR1 and reduced the phosphorylation of PI3K and AKT [74]. S1PR1 upregulation abolished the inhibitory effects of isorhamnetin on KF proliferation, migration, invasion, and fibrogenesis.
KF proliferation was inhibited by curcumin (2.5 and 5 μg mL−1), gallic acid (5 and 10 μg mL−1), quercetin (10 and 20 μg mL−1), kaempferol (20 μg mL−1), protocatechuic acid (100 and 200 μg mL−1), p-coumaric acid (400 μg mL−1), ferulic acid (400 μg mL−1), and chlorogenic acid (400 μg mL−1) [111]. p-Hydroxy benzoic acid had no effect, and caffeic acid was very toxic [111]. These effects were attributed to cell cycle arrest rather than apoptosis [111]. The cell proliferation was resumed after the removal of each phytochemical and relatively slow recovery was seen with quercetin, chlorogenic acid, or curcumin [111]. Quercetin, gallic acid, protocatechuic acid, and chlorogenic acid more effectively inhibited the collagen lattice contraction by NFs and hypertrophic scar-derived fibroblasts (HSFs) than other compounds [111]. The collagen lattice contraction resumed when each compound was removed, and the recovery was slowest with quercetin [111].
Curcuminoids (25–100 nM), consisting of curcumin, demethoxycurcumin, and bisdemethoxycurcumin, lowered the cellular levels of total soluble collagens, pro-collagen 1, fibronectin, and TGF-β1, and reduced the phosphorylation of SMAD2 in KFs stimulated with bleomycin [115]. Curcumin was the major form of curcuminoids that entered and accumulated inside cells [115].
Resveratrol attenuated cell proliferation, induced apoptosis, and lowered the expression levels of TGF-β1, collagen 1, α-SMA, and heat shock protein (HSP) 47, which is involved in collagen folding and remodeling [36,132], in KFs but not in NFs [116]. It also attenuated cell proliferation, induced apoptosis, and reduced the collagen synthesis of KFs under hypoxia by downregulating hypoxia-inducible factor (HIF)-1α.
3. Terpenoids
Asiaticoside, a component of Centella asiatica, attenuated KF proliferation and lowered the expression levels of collagen 1/3 and TGFβR1/2 [117]. Asiaticoside did not affect the expression levels or the phosphorylation of SMAD2/3/4 but increased the expression level of SMAD7, which acts as an intracellular antagonist of the TGF-β signaling pathway [117]. Asiaticoside attenuated KF proliferation, invasion, and the phosphorylation of ERK1/2, p38 MAPK, and SMAD2/3 (linker region) stimulated by GDF-9 [82].
Asiatic acid from Centella asiatica suppressed the TGF-β1-induced expression of collagen 1 and plasminogen activator inhibitor-1 (PAI-1) and the phosphorylation of SMAD2/3, while increasing SMAD7 expression [118]. These effects of asiatic acid on KFs were abrogated by PPAR-γ antagonist GW9662 or peroxisome proliferator-activated receptor gamma (PPAR γ) siRNA [118].
Ginsenoside Rg3 (50 or 100 µg mL−1) attenuated the proliferation, migration, invasion, angiogenesis, and collagen synthesis of KFs and inhibited the TGF-β/SMAD and ERK-mediated signaling pathways [119].
Tagitinin C reduced KF viability after 72 h (IC50, 0.122 μg mL−1), as potently as mitomycin C (IC50, 0.120 μg mL−1) [120]. Tagitinin C at IC50 decreased keloid collagen deposition to 53.1% of the control level, whereas mitomycin C IC50 decreased it to 60.4% [120]. Tagitinin C and mitomycin C were less toxic to NFs (IC50; 35.05 μg mL−1 and 16.21 μg mL−1, respectively) [120]. The selective cytotoxicity index of tagitinin C and mitomycin C on KFs versus NFs was calculated to be 287 and 135, respectively [120].
Treatment of KFs with ingenol-mebutate induced morphological alterations and DNA fragmentation, which were associated with reduced cell growth and increased apoptosis [121]. It induced the expression of miR-34a in a p53-dependent manner and upregulated proapoptotic genes, such as caspase-10, while downregulating antiapoptotic genes, such as BCL-2 [121].
Glycyrrhizin, a component of Glycyrrhiza glabra, lowered the expression level of HMGB1 in KFs and attenuated cell proliferation and autophagy while increasing apoptosis [70]. Glycyrrhizin inhibited the expressions of ERK1/2, AKT, and NF-κB induced by HMGB1 [70]. Glycyrrhizin lowered the expression levels of TGF-β1, SMAD2/3, ERK1/2, collagen 1/3, fibronectin, and elastin in KFs [70].
Oleanolic acid attenuated the proliferation of KFs [122]. It lowered the expression levels of intra- and extracellular fibronectin, procollagen 1, and α-SMA while increasing MMP1 [122]. It inhibited the phosphorylation of SMAD2 and SMAD3 and attenuated the increases in fibronectin, procollagen 1, and α-SMA and the decrease in MMP1 in KFs stimulated with TGF-β1.
4. Alkaloids
Camptothecin, originally isolated from Camptotheca acuminata, is a topoisomerase inhibitor that has been used in cancer therapy [133]. Camptothecin lowered the expression levels of collagen 1/3 in KFs without causing cellular toxicity [123]. Its effects on the collagen 3 level were relatively smaller, and consequently, the ratios of collagen 1 to collagen 3 were decreased by the camptothecin treatment [133].
10,11-Methylenedioxycamptothecin loaded in hyaluronic acid nanoemulsions were delivered percutaneously to the keloid lesion area in a mouse model [124]. Its internalization by KFs and delivery to the nucleus resulted in decreased cell proliferation [124]. It increased the expression levels of TGF-β1, SMAD3, and SMAD7, and downregulated PAI-1 in KFs, implicating an overall suppression of the TGF-β-mediated signaling pathway [124].
Oxymatrine, an alkaloid compound extracted from Sophora japonica, lowered the expression levels of collagen and SMAD3 in KFs in vitro without affecting the expression levels of TGF-β1, TGFβR1/2, SMAD4, and SMAD7 [125]. Oxymatrine inhibited the phosphorylation and nuclear translocation of SMAD3 induced by TGF-β1 [125]. Thus oxymatrine could attenuate collagen synthesis by inhibiting the TGF-β/SMAD signaling pathway.
Vincristine is one of the vinca alkaloids originally separated from Catharanthus roseus, and is used as an anticancer drug [134]. Vincristine inhibited cell proliferation by inducing cell cycle arrest in the G2/M phase and promoting apoptosis in SH-SY5Y human neuroblastoma cells [135]. Vincristine showed cytotoxicity to the primary KFs and NFs, with higher potency to the latter [24]. The resistance of KFs could be largely abrogated by verapamil (a calcium channel blocker) [24].
The treatment of KFs with paclitaxel or LY294002 (a PI3K inhibitor) lowered their expression levels of TNF-α, IL-6, TGF-β1, α-SMA, and collagen 1 [126]. Paclitaxel also blocked the AKT/GSK3β signaling pathway in KFs and keloid tissues [126]. Paclitaxel-cholesterol-loaded liposomes inhibited KF proliferation, migration, and invasion, and promoted apoptosis and cell cycle arrest in the G2/M phases more effectively than paclitaxel itself in vitro [126]. Paclitaxel-cholesterol-loaded liposomes had better performance in inhibiting keloid growth compared to paclitaxel in the keloid-bearing BALB/c nude mouse model [126].
5. Other Compounds
Aspidin PB inhibited the expression of collagen 1, CTGF, and α-SMA in KFs stimulated by TGF-β1 [127]. It inhibited both the SMAD2/3-mediated signaling pathway and the PI3K/AKT-mediated signaling pathway stimulated by TGF-β1 [127].
Tanshinone IIA attenuated the proliferation of KFs, whereas it did not affect the proliferation of NFs [128]. It increased the percentages of KF cells in the G0/G1 phases and the cells undergoing early apoptosis [128]. It also decreased the expression of survivin [128].
A selenium-containing polysaccharide from Ziyang green tea (Se-ZGTP) or short hairpin RNA (shRNA) for neuron-glia 2 inhibited the proliferation of KFs [129]. Se-ZGTP or NG2 shRNA induced apoptosis mediated by an increase in pro-apoptotic BAX expression, the activation of caspase-3, the subsequent cleavage and inactivation of poly (ADP-ribose) polymerase (PARP), and a decrease in the expression levels of anti-apoptotic BCL-2 [129]. Se-ZGTP or neuron-glia 2 shRNA reduced collagen 1 and protein expression in KFs following TGF-β1 stimulation [129].
As a photodynamic therapy, the combined treatment of hypocrellin A with a light-emitting diode (LED)’s red light irradiation increased ROS production [136] and decreased KF viability, proliferation, invasion, collagen production, and the expression of collagen 1/3, α-SMA, and fibronectin, while increasing cell apoptosis and the expression of BAX and caspase-3 [130]. The combined photodynamic therapy reduced autophagy, the protein expression of Beclin-1, and the conversion of LC3-I to LC3-II [130]. It inhibited the expression of TGF-β and the downstream signaling pathways mediated by ERK1/2 and SMD2/3 [130].
This entry is adapted from the peer-reviewed paper 10.3390/ijms25021235
This entry is offline, you can click here to edit this entry!
