Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Medicine, General & Internal
Cancer patients are at greater risk of developing venous thromboembolism compared to the general population, which can lead to a decreased quality of life, a worsened prognosis, and increased treatment costs. Many cancer patients will experience venous thromboembolism (VTE) at some stage, with the highest rate in the initial period following diagnosis. Novel cancer therapies may further enhance the risk. VTE in a cancer setting is associated with poor prognostic, a decreased quality of life, and high healthcare costs.
- venous thromboembolism risk
- ambulatory cancer
- risk assessment
1. Introduction
Cancer patients often present with a prothrombotic state due to the abnormalities in each component of Virchow’s triad, thus contributing to thrombosis. Researchers estimated that VTE would occur in 4–20% of cancer patients at some stage, with the highest risk immediately following cancer diagnosis [1]. In the last period, the VTE incidence in oncologic patients has increased in the context of the higher performance of imaging techniques and the development of new cancer treatments that improved survival [2]. After cancer diagnosis, the 12-month cumulative VTE incidence was 3%, a percentage nine times higher when compared to the general population [2].
However, despite improved cancer treatment, VTE in cancer patients is strongly associated with a poor prognosis. The cumulative mortality in VTE cancer patients was 27.7% after one month, 48.7% after three months, 68.2% at one year, and 84.1% after five years, which is much higher than the cumulative mortality in cancer patients without VTE (7.5%, 17%, 38.5%, and 84.1%, respectively) [3]. Pulmonary embolism (PE) was associated with a poorer prognosis than venous thrombosis [3]. The one-year mortality of the PE cancer patients was 73% in Sørensen et al.’s study, as compared to 39.3% in the non-cancer cohort [3].
Khorana et al. reported that 17.1% of the patients recently diagnosed with cancer and with VTE events would develop recurrent episodes of VTE during a nine-month follow-up period [4]. The total costs related to the healthcare of the patients with VTE recurrence were very high, suggesting the necessity of reducing VTE risk in cancer patients [4].
Thromboprophylaxis in hospitalized cancer patients and perioperative settings is widely accepted in clinical practice and supported by the guidelines. However, most cancer patients would develop VTE in the outpatient setting. Primary thromboprophylaxis is not routinely recommended, except for high-risk cancer patients. Selecting an ambulatory cancer patient who would benefit from thromboprophylaxis is still challenging because of the specific bleeding risk. The Khrorana score is mainly the recommended tool in this setting, but many limits of this old score have been reported. Novel approaches have been proposed. Clinical features, routine hematologic and coagulation lab testing, new biomarkers, and genetic data, separately or grouped, were introduced in the novel risk scores, nomograms, or machine learning algorithms to accurately assess the VTE risk in ambulatory cancer patients in general and specific tumors. This research aims to present the current relevant knowledge in this setting starting from the guideline recommendations and continuing with the specific risk assessment methods to help clinicians in their decision regarding primary thromboprophylaxis in ambulatory cancer patients (Figure 1). The future directions provided by the recent research papers are also presented.
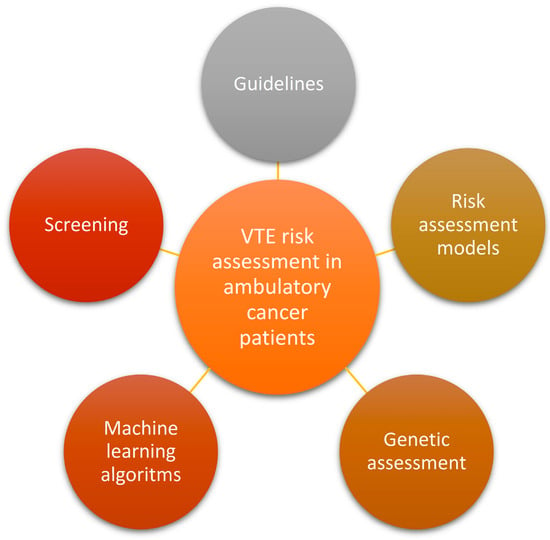
Figure 1. The current relevant knowledge in VTE risk assessment in ambulatory cancer patients. Abbreviations: VTE—venous thromboembolism.
2. VTE Screening in Ambulatory High-Risk Oncologic Patients
Cancer and thrombosis are strongly related. VTE can be the first clinical sign of undiagnosed cancer, especially when the event is unprovoked [13], while cancer represents a risk factor in VTE occurrence. In this last setting, guidelines issued recommendations for hospitalized and surgical cancer patients and high-risk outpatients. Gainsbury et al. found a 10.1% prevalence of preoperative deep venous thrombosis (DVT) in asymptomatic patients undergoing major oncologic surgery and suggested the preoperative screening with lower extremity venous duplex ultrasound (US) in this setting [14]. Increasing age, recent diagnosis of sepsis, and a history of prior VTE were significantly associated with preoperative DVT [14].
Detecting VTE high-risk outpatients with cancer is still challenging. VTE screening may be an answer in this setting. In total, 6.6% of venous thrombosis was found by Heidrich et al. in all tumor patients [15]. The same authors reported a much higher incidence of 33% when using an imaging prospective approach [15]. Loftus et al. researched the role of venous US screening in incidentally detecting VTE in high-risk patients with cancer in a multicenter trial. The studied 117 patients were asymptomatic, had a Khorana score ≥ 3, and were starting new systemic chemotherapy [16]. The lower-limb venous US and a contrast-enhanced CT baseline screening discovered 9% incidental VTE (6% DVT, 1% pulmonary embolism, 1% DVT and pulmonary embolism) [16]. The patients were screened further every four weeks for a 12-week period with venous US and at 12 weeks with contrast-enhanced CT [16]. Researchers proposed the lower-limb venous US screening in addition to the oncologic surveillance CT in high-risk ambulatory cancer patients setting with a Khorana score ≥ 3 [16].
This approach could help in early VTE detection in latent stages, preventing VTE progression and thus decreasing morbidity and costs [16]. Kourlaba et al. also reported US screening of high-risk cancer patients as a cost-effective strategy compared to clinical surveillance, even when all patients with a positive first US underwent a second US [17]. Kunapareddy et al. proposed an electronic alert to identify high-risk patients and suggest US screening for early detection [18]. Holmes et al. reported the success of a multidisciplinary program related to Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) [19]. The high-risk patients identified by Khorana and Protecht scores (≥3 points) were offered a hematology consultation to consider VTE prophylaxis, further referring the results of the consultation to the oncologist [19].
VTE risk was predicted by baseline D-dimer levels [20,21]. Niimi et al. recently reported the optimal D-dimer cut-off value of 4.0 μg/mL for predicting DVT in patients with malignancy [22]. Its association with risk assessment scores performed better in VTE prediction [21,22]. D-dimer was reported in another study as part of the thromboembolism risk assessment when added to fibrinogen level [23]. Oi et al. found that high D-dimer levels at VTE diagnosis were associated with an increased risk for short-term and long-term mortality and with long-term recurrent VTE, especially in patients with active cancer [24]. During a median follow-up of 30 months, D-dimer positively correlated with the reoccurrence of VTE (p = 0.0299) and mortality in cancer patients with VTE (p < 0.0001) and without VTE (p = 0.0008) [25]. D-dimer level positively correlated in Koch et al.’s study with VTE reoccurrence and mortality during a 30-month period [25]. The relationship with mortality was reported both in cancer patients who presented VTE and in cancer patients without VTE [25].
Another VTE risk factor is the soluble P-selectin (sP-selectin). A cut-off level of 53.1 ng/mL could predict VTE in cancer patients with no difference between tumor sites [26]. Zhang et al. recommended sP-selectin level for early identification of cancer-associated VTE and monitoring [27].
Khorana et al. recently studied the biomarkers distribution in patients with and without VTE diagnosed with cancer [28]. In the two groups, there were reported baseline lower levels of stromal cell-derived factor-1, thyroid-stimulating hormone, and monocyte chemotactic protein 4 and higher levels of growth hormone and interleukin-1 receptor type 1 [28]. ST2, IL-8, and C-reactive protein were significantly different between survivors and those who died [28].
Table 2 presents the relevant studies presenting modalities and importance of VTE screening among ambulatory cancer patients.
Table 2. The relevant studies presenting modalities and importance of VTE screening among ambulatory cancer patients.
| Screening Modality | Authors (Year) [Ref] | No. Patients | VTE Detected (%) | Type of Tumors | Main Findings |
|---|---|---|---|---|---|
| Lower limb venous duplex US | Gainsbury et al. (2018) [14] | 346 | 10.1 | Solid cancer | High-risk cancer patients may benefit from screening lower extremity venous duplex US before surgery. |
| Lower limb duplex US and/or venography | Heidrich et al. (2009) [15] | 97 | 33 | Various types | Regular screening for thrombosis is indicated even in asymptomatic tumor patients |
| Lower limb duplex US and contrast-enhanced chest CT | Loftus et al. (2022) [16] | 117 | 58 | Solid cancers | Suggested to add US screening to routine oncologic surveillance CT in high-risk ambulatory cancer patients (Khorana score ≥ 3) |
| Lower limb venous US | Kourlaba et al. (2017) [17] | 907 | - | various | Screening high-risk cancer patients via US to detect asymptomatic DVT is a cost-effective strategy over clinical surveillance |
| Automated alert Lower limb venous US |
Kunapareddy et al. (2019) [18] | 194 | 12.5 | various | An automated alert may help in early detection of DVT in high-risk cancer patients |
| VTEPACC model | Holmes et al. (2020) [19] | 918 | 23.2 | various | VTEPACC involves a multidisciplinary approach |
| D-dimer F 1 + 2 |
Ay et al. (2009) [20] | 821 | 7.6 | various | The cumulative probability of developing VTE after 6 months was highest in patients with both elevated D-dimer and elevated F 1 + 2 |
| Baseline D-dimer | Schorling et al. (2020) [21] | 100 | 11.2 | Solid cancers | VTE risk was well predicted by baseline D-dimer levels. |
| D-dimer | Niim et al. (2023 [22] | 208 | 28.4 | various | The optimal D-dimer cut-off value for the DVT diagnosis in cancer patients was 4.0 μg/mL. |
| D-dimer | Oi et al. (2020) [24] | 2852 | various | Elevated levels at diagnosis were associated with an increased risk for short-term and long-term mortality. | |
| D-dimer | Koch et al. (2023) [25] | 526 | 39.73 | various | Levels above the 10-fold upper reference limit contain diagnostic and prognostic information |
| sP-selectin | Ay et al. (2008) [26] | 687 | 6.4 | various | Higher levels independently predict VTE in cancer patients |
| sP-selectin | Zhang (2023) [27] | 1882 | 24.17 | various | Metaanalysis. Role in early identification and monitoring A higher level in Asian cancer patients |
| Various biomarkers | Khorana (2022) [28] | 124 | 50 | various | SDF-1 and TSH were the strongest predictors of VTE |
Abbreviations: CT, computed tomography; DVT, deep venous thrombosis; F 1 + 2, prothrombin fragment 1 + 2; SDF-1, stromal cell-derived factor1; VTE, venous thromboembolism; VTEPACC, Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic; TSH, thyroid-stimulating hormone; US, ultrasonography.
microRNAs (miRNAs) represent a promising class of biomarkers in VTE prediction in cancer, but until now, only a few small-sample-size studies, lacking external validation, have investigated their role in this setting [29]. The long non-coding RNAs (lncRNAs) may have a role as well in VTE pathogenesis [30]. Ten lncRNAs were implicated in VTE pathogenesis, but future research is needed in this setting [30].
Genetic assessment may help VTE risk stratify and prognostic in the cancer population. Thrombogenesis-related genetic polymorphisms are already studied in this setting and are integrated in specific risk scores alone, or together with clinical features. However, more prospective studies are required before clinical application.
This entry is adapted from the peer-reviewed paper 10.3390/cancers16020458
This entry is offline, you can click here to edit this entry!
