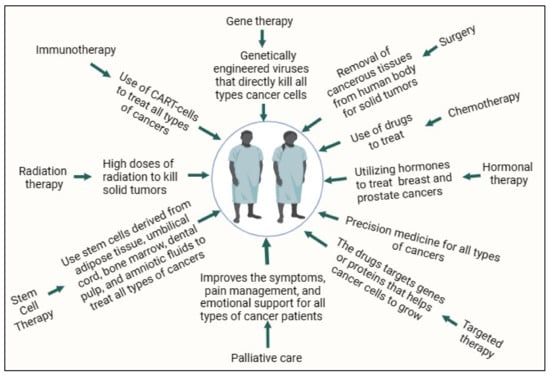
Moreover, early identification of cancer frequently results in improved treatment outcomes. The treatment options for cancer differ, according to the nature and stage of the disease. Stem cell transplantation, radiation therapy, chemotherapy, targeted therapy, immunotherapy, and hormone therapy are the most common therapeutic techniques [
11]. Possible treatment modalities include a combination of these methods. Prolonged investigations pertaining to the etiology, prevention, and therapeutic aspects of cancer have recently yielded noteworthy progress. These include the advancement of precision medical strategies, targeted medicines, and immunotherapies [
12]. The prognosis of many cancer patients has substantially improved as a result of ongoing research and advancements in medical therapies, despite the fact that cancer continues to be a major worldwide health concern. Advancements in cancer therapy, early detection, and prevention are critical components of the ongoing battle against this disease. Oncology therapy, or cancer therapy, encompasses a range of medical procedures and therapies implemented to control and eradicate cancer [
13]. Cancer type and stage, in addition to the patient’s general health and treatment objectives, influence treatment selection. Cancer therapy can be classified into several primary categories, on a large scale. Surgical techniques to remove malignant tumors and surrounding tissues comprise the first category [
14]. Surgery is often the primary treatment for solid tumors such as breast cancer, lung cancer, and colon cancer. It can also be used for diagnostic purposes, staging, and alleviation of symptoms and complications [
14,
15]. The second type is radiation therapy, or radiotherapy, which uses high-energy beams of radiation to target and kill cancer cells [
16,
17]. It can be used as a monotherapy or in combination with other therapies. Radiation therapy is often employed for localized tumors, and may be administered before or after surgery. The third category is chemotherapy, which involves the use of drugs to destroy cancerous cells or inhibit their growth [
18], which can be administered either orally or parentally. Chemotherapy is often used for systemic or metastatic cancers, but can also be part of adjuvant therapy following surgery. The fourth category is immunotherapy, or biological therapy, which harnesses the body’s immune system to recognize and attack cancer cells [
19]. These include monoclonal antibodies, checkpoint inhibitors, cytokines, and cancer vaccines. Immunotherapy has shown remarkable improvement in treating various cancer types, including melanoma, lung cancer, and some types of leukemia. The fifth category is targeted therapy, which uses drugs that specifically target cancer cells by interfering with the molecules or pathways that drive their growth and spread [
20]. These drugs are often more precise and have fewer side effects than traditional chemotherapies. Targeted therapies are used to treat tumors with specific genetic mutations or other targetable characteristics. The sixth type is associated with the use of hormones, which are primarily used for hormone-sensitive cancers, including breast and prostate cancer [
21]. This involves medications that block the effects of hormones or reduce their production, as hormones can fuel the growth of certain cancers. The seventh category is known as stem cell transplantation (bone marrow transplantation), which is used to replace damaged or cancerous bone marrow with healthy stem cells [
22]. It is often used in the treatment of blood-related cancers, including leukemia and lymphoma. The eighth type is precision medicine, which involves tailoring cancer treatment to an individual’s specific genetic and molecular profiles [
23]. This approach aims to maximize the effectiveness of the therapy while minimizing side effects. The ninth type is palliative care, which is an indispensable component of cancer therapy that emphasizes improving the quality of life of patients with advanced or terminal cancer [
24]. It addresses symptoms, pain management, and emotional support, and may be combined with curative treatments. Cancer therapy is also known as multimodal therapy, often administered as a combination of these treatments, which are summarized in
Figure 1.
2. Historical Perspective
Since ancient times, natural drugs have been central to medicinal practices and have served as primary healthcare solutions across various cultures. These drugs, encompassing plant-based, animal-based, and mineral-based medicines, have been particularly prominent in India and China, which are often considered mother nations for the utilization of natural-product drugs [
32]. Approximately 80% of the world’s population relies on traditional medicinal systems, and plant-derived drugs have significant therapeutic value [
33]. Medicinal plants, the key components of these systems, have been used for their healing properties for centuries.
According to Ashok and Devasagayam (2007), nearly 70% of Indians rely on natural medications, a figure that increases to 90% in Africa. Herbal drugs, a critical component of natural drugs, play a significant role in Ayurveda, yoga, Unani, Siddha, homeopathy, and naturopathy [
34]. Particularly in the realm of cancer, the convergence of ethnobotany and traditional knowledge is crucial to the development and use of natural medicines. Ethnobotanical investigations, which focus on the utilization of plants and other natural compounds by many civilizations, have yielded vital knowledge regarding their potential therapeutic attributes. Scientists and researchers have frequently been influenced by this conventional approach when attempting to identify plants that may possess anticancer properties. The utilization of periwinkle in traditional medicine, for instance, has resulted in the identification of vinca alkaloids, which are essential chemotherapeutic agents. The persistent integration of conventional wisdom and contemporary scientific investigation remains a pivotal catalyst in the ongoing pursuit of novel anticancer substances [
35,
36,
37].
In the realm of anticancer drug discovery, natural products are pivotal because they offer a diverse array of therapeutic possibilities. This historical overview traces the journey from traditional medicine to modern cancer therapy. Initially, plant- and animal-derived compounds were used in traditional medicine, laying the foundation for understanding their therapeutic potential [
38,
39]. The 20th century saw a significant shift in the systematic isolation and characterization of active compounds from natural sources, leading to breakthroughs such as Vinca alkaloids, which had a substantial impact on treating challenging cancer types [
39,
40,
41].
Progression in extraction and separation methodologies has facilitated the transformation of natural substances from conventional applications to contemporary medicinal agents. Previously, techniques employed to extract therapeutic chemicals from plants and other natural sources were frequently primitive, and lacked efficiency. However, since the introduction of modern technologies and chemistry, these techniques have progressed considerably. The use of methodologies such as ultrasonic, microwave-assisted, and supercritical fluid extraction has facilitated the selective and effective separation of active chemicals [
42,
43]. In addition to increasing the yield and purity of natural products, these developments have enabled the identification of novel molecules with anticancer effects. The capacity to extract and analyze the distinct constituents of conventional treatments has proven crucial in comprehending their mechanisms of action and formulating standardized pharmacological drugs [
44,
45].
The development of Taxol, or paclitaxel, from the Pacific yew tree epitomizes this evolution, balancing ecological sustainability with therapeutic advancement. Discovered as part of the National Cancer Institute program in the 1960s, Taxol’s journey highlights the integration of emerging technologies such as high-throughput screening and computational modelling in drug discovery [
38,
46,
47]. Despite challenges such as supply issues and ecological impacts, innovations in synthetic and semi-synthetic methodologies have paved the way for the next generation of anticancer drugs [
48,
49].
Taxol’s mechanism of action, promoting tubulin assembly into microtubules and stabilizing them against disassembly, is distinct from other treatments of its time, making it a unique and effective anticancer agent [
50]. However, the development of Taxol faced challenges, owing to the low abundance of the compound in its natural source and the ecological implications of harvesting yew trees. Advances in semi-synthesis from more abundant yew species eventually led to FDA approval of ovarian cancer treatment in the early 1990s [
49,
51]. Taxol’s success story not only underlines the importance of natural products in drug discovery, but also emphasizes the need for sustainable sourcing and interdisciplinary collaboration in pharmaceutical development.
The incorporation of natural substances into contemporary pharmacopeia signifies a meaningful advancement in pharmaceutical exploration. Although the utilization of natural chemicals was first inspired by traditional medicine, their integration into conventional healthcare has necessitated stringent scientific verification and standardization. Extensive pharmacological and toxicological testing was conducted as part of this procedure, to guarantee safety and effectiveness in strict adherence to rigorous standards of regulatory bodies [
40]. The incorporation of natural compounds, such as Taxol, into pharmacopeia represents a transition from anecdotal and empirical use to evidence-based medicine. Furthermore, it emphasized the potential of natural products as an abundant reservoir of innovative therapeutic agents with the capacity to tackle a multitude of complex health ailments, such as diverse forms of cancer [
52,
53].
3. The Importance and Potential of Natural Products in Drug Discovery
Promising and novel cancer therapies have been explored and studied in natural compounds and their structural analogs, and show exceptional variation in chemicals. In addition, the distinct molecular characteristics of natural products enable them to offer greater safety and effectiveness [
47]. Chemotherapy drugs like doxorubicin and cisplatin, as well as radiotherapy, are commonly employed in cancer treatment, but are associated with severe adverse reactions and toxic side effects. Radiotherapy, in particular, can lead to cognitive dysfunction and a decline in brain function [
54]. Additionally, chemotherapy may result in secondary tumors and damage to normal tissues, presenting challenges for cancer survivors. Common issues during chemotherapy include bone marrow suppression, causing immunosuppression, and various toxicities such as liver, kidney, and heart toxicity [
55]. For instance, cisplatin can induce nausea, vomiting, acute kidney injury, neurotoxicity, and ototoxicity. Some chemotherapy drugs may not effectively target less-active cancer cells, influencing overall survival and prognosis, negatively [
56].
In recent times, natural compounds have gained importance in cancer prevention and treatment. These compounds, including phenols (such as curcumin, quercetin, resveratrol, and capsaicin), flavonoids (quercetin, tanshensin IIa, and icariin), terpenoids (andrographolide, artesunate, and atractylodes), alkaloids (matrine, berberine, and piperine), and others, play a crucial role. They exhibit anti-inflammatory properties, promote cell apoptosis, inhibit invasion and metastasis, and enhance immune responses. These natural compounds have demonstrated efficacy against various cancers like lung cancer, breast cancer, and ovarian cancer [
57].
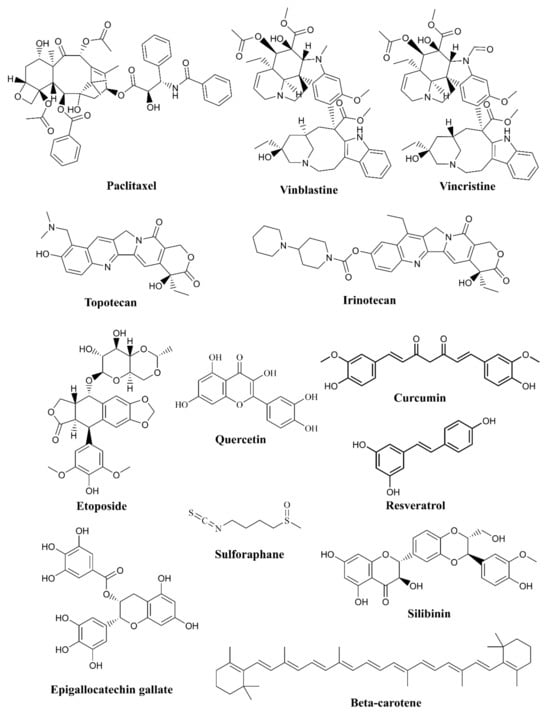
Compounds generated from bacteria, plants, and marine organisms are considered to be natural products. Throughout history, natural products have been crucial for the advancement in cancer treatments. Research on anti-cancer medication employs natural products because of their extensive chemical diversity, distinctive structural characteristics, and biological activity, which has less toxicity. As some of these substances have undergone evolutionary adaptations to protect species from illnesses, including cancer, they are promising candidates for anticancer drugs. Screening the anti-cancer activity of natural-product extracts is a customary initial step taken by researchers. Subsequently, promising extracts are isolated and purified to determine their precise active components. It is frequently possible to enhance the quality of natural products by chemical modification, as in the case of improving their bioavailability or targeting particular types of cancer cells. By synthesizing analogs or derivatives, medicinal chemists can augment the drug-like characteristics of substances.
About fifty percent of drugs originated from natural substances. These could be compounds that are either semi-synthetic or obtained from flora [
58]. Examples of natural products used in anti-cancer drug development include the following (
Figure 2 and
Table 1).
Figure 2. Natural compounds from various sources exhibit anti-cancer activity.
-
Paclitaxel: derived from the Pacific yew tree, and is used to treat various cancers, including breast, ovarian, and lung cancers [
59].
-
Vinblastine and Vincristine: these alkaloids are derived from the
Madagascar periwinkle plant and are used in the treatment of leukemia and lymphoma [
60].
-
Camptothecin: originally isolated from the Chinese tree
Camptotheca acuminata, derivatives of this compound, such as Topotecan and Irinotecan, are used in the treatment of ovarian and colorectal cancers [
61,
62].
-
Etoposide: derived from the mayapple plant, etoposide is used to treat lung and testicular cancer [
63].
Natural products have several advantages in drug discovery, including structural diversity, potential for multi-target effects, and the presence of compounds that can overcome drug resistance. However, the challenges in sourcing and standardizing natural products, as well as issues related to patent protection, can complicate their development as anticancer drugs. Nevertheless, ongoing research in this field continues to yield promising results for novel cancer treatments. These compounds can interact with various molecular pathways and cellular processes associated with cancer development and progression (
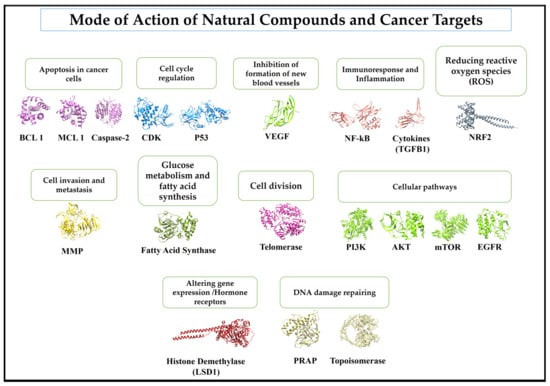
Figure 3). The common mode of action for some cancer targets are like the following:
Bcl-2,
Bcl-xL, and
Mcl-1, and the activation of caspases enzymes to induce apoptosis in cancer cells [
64]; inhibiting the cell cycle regulating enzymes/proteins such as cyclin-dependent kinases (CDKs) and p53 [
65]; inhibiting the formation of new blood vessels in tumor cells by inhibiting enzyme-like vascular endothelial growth factor (VEGF) [
66], by targeting proteins associated with immunoresponse and inflammation such as nuclear factor-κB (NF-κB) and cytokines [
67]; reducing reactive oxygen species (ROS) and increasing the anti-oxidation defense against cancer-spreading cells [
68]; inhibiting cancer cell invasion and metastasis by inhibiting group of enzymes known as matrix metalloproteinases (MMPs) and increasing the activity of Tissue Inhibitors of Metalloproteinases (TIMPs), which counter the effects of MMPs [
69]; inhibition of DNA-damage-repairing enzyme such as poly(ADP-ribose) polymerase (PARP) [
70]; altering gene expression in cancer cells by modifying DNA methylation and histone acetylation involved in epigenetics [
71], in breast- and prostate-cancer natural-product target hormone receptors like estrogen and androgen receptors [
72]; by interfering in cellular pathways such as PI3K/Akt/mTOR and the EGFR (Epidermal Growth Factor Receptor) pathway [
73,
74,
75]; by inhibiting telomerase, an enzyme which helps to divide tumor cells indefinitely [
76]; by inhibiting glucose metabolism and fatty acid synthesis [
77,
78]; and by inhibiting the topoisomerase group of enzymes to maintain damaged-DNA repair and replication [
79,
80].
Table 1. Various natural compounds used as anti-cancer treatments in treating various cancers via different pathways.
Figure 3. Mode of action and molecular targets of natural compounds involved in cancer development. The molecular targets are BCL-1, MCL-1, Caspase-2, CDK, p53, VEGF (Vesicular Endothelial Growth Factor), NF-kB, TGFB1, NRF2, MMP, Fatty Acid Synthase, Tellomarase, P13, AKT, mTOR, EGFR, Histone Demthylase, PRAP, and Topoisomease.
4. Present Status of Natural Compounds
Many natural compounds are under investigation in preclinical and clinical trials for their potential use in various medical applications, including cancer treatment, anti-inflammatory agents, and antioxidants (
Figure 2). These compounds are derived from plants, marine organisms, and other microorganisms. Some examples of natural compounds that have undergone, or are currently undergoing, pre-clinical and clinical trials are Curcumin, which was tested for anti-inflammatory, antioxidant, and potential anti-cancer properties [
104]; Resveratrol, which has been tested in both preclinical and clinical trials for cardioprotective and anti-aging effects [
105]; Epigallocatechin Gallate (EGCG), which is being investigated for the treatment of various diseases, including cancer, neurodegenerative disorders, and metabolic syndrome [
106]; Paclitaxel, which is an established chemotherapy drug for various cancers, including breast, ovarian, and lung cancer [
107]; Quercetin, which has shown promising results in pre-clinical as well as clinical trials as an anti-inflammatory, antioxidant, and potential anti-cancer agent [
108]; and Camptothecin and its derivatives, such as Topotecan and Irinotecan, which are used in the treatment of ovarian and colorectal cancer [
109]. Clinical trials of Beta-carotene have explored its potential benefits, such as reducing the risk of certain cancers and eye conditions [
110]. Sulforaphane is under study in pre-clinical and clinical trials for its potential anti-cancer and antioxidant effects [
111]. Silibinin has shown potential in preclinical and early-stage clinical trials for various cancers and liver diseases, including hepatitis and cirrhosis [
112]. These natural compounds are just a few examples of substances from nature that are being investigated in pre-clinical and clinical trials.
The use of natural chemicals in conventional treatments represents a substantial advancement in modern health care. Several natural medicines previously confined to traditional applications are undergoing rigorous effectiveness testing for a variety of medical diseases, as research progresses. This demonstrates a trend toward more holistic and integrative therapeutic methods [
40,
113]. A meticulous equilibrium between scientific validation and traditional knowledge is necessary for this shift. The clinical efficacy of natural chemicals, such as paclitaxel, highlights the capacity of these substances to supplement, or even improve, traditional medicinal interventions. Nevertheless, the inclusion of these substances in conventional treatment plans is contingent upon stringent clinical validation to ascertain their efficacy and safety when utilized in conjunction with, or in lieu of, synthetic medications. Although natural substances frequently possess low toxicity and tolerance, it is important to perform thorough scientific studies to ascertain their safety and effectiveness in treating a wide range of medical diseases. Clinical trials are vital for identifying the possible advantages and limitations of these natural substances as medical therapies. The continuous process of integrating and conducting comprehensive evaluations indicates an expanding acknowledgment and acceptance of the benefits offered by natural chemicals in contemporary medicine [
114,
115].
5. Computational Approaches in Drug Discovery
Computational methodologies have brought about a paradigm shift in the domain of pharmaceutical discovery, providing indispensable instruments across the entire drug development life cycle. These techniques substantially lower expenses and increase the effectiveness of processes involved in identifying and producing new medications. Prominent computational techniques include docking, virtual high-throughput screening, and protein structure prediction. These methods enable the expeditious evaluation of extensive compound libraries and the detection of potential binders via sophisticated modeling, simulation, and visualization methodologies [
116,
117]. Various computational drug discovery methods such as molecular docking, pharmacophore modeling and mapping, de novo design, molecular similarity calculations, and sequence-based virtual screening have undergone significant refinement in recent decades. Consequently, the screening and design of drug candidates have become considerably more precise and efficient [
118]. The integration of computational techniques into the drug-design and discovery processes has become an essential element of this development, enabling researchers to conserve significant time and money [
119]. Furthermore, several computational methods, such as the NMR structure–activity connection, are sophisticated iterations of conventional procedures, illustrating how technology may augment and optimize the process of drug development [
116]. As mentioned earlier, developments highlight the pivotal significance of computational approaches in contemporary pharmaceutical research, signifying a substantial paradigm change in the approach to drug discovery and development.
Computational methodologies have become indispensable adjuncts to conventional experimental processes in the realm of cancer drug discovery, substantially bolstering efficacy and diminishing the financial outlay associated with the development of novel therapeutics [
117]. The exponential expansion of computational techniques used in the field of drug discovery, particularly those targeted at anticancer medicines, has significantly influenced the design of anticancer drugs. These technologies have yielded significant knowledge on cancer therapy, presenting new opportunities for the discovery and exploration of innovative pharmaceutical candidates [
120].
Computational in silico techniques have witnessed significant progress in recent years, particularly in the modeling of biological processes for the identification of novel disease-relevant targets. Significantly contributing to these achievements, machine learning and deep-learning techniques have enabled the identification of novel drug–phenotype and drug–target relationships [
121]. The utilization of computational techniques in the development of prospective anticancer medications has yielded significant advancements in the realm of cancer treatment, throughout the years [
122]. The development of omics data during the past decade has also enabled computer prediction of anti-cancer therapies, thereby enhancing the efficacy of drug research. For instance, merging high-throughput transcriptome data with drug-response data has been extensively utilized in biomarker identification and medication prediction [
123].
Computer-aided drug discovery (CADD) is a promising technology for drug development. This increases the efficiency, effectiveness, and speed of the drug design process, thus tackling the problem of lowering research expenses and accelerating the creation of novel medications. In particular, the influence of CADD in the field of anticancer medicine has revolutionized the design of anticancer drugs and offers essential insights into cancer treatment [
120]. In essence, the incorporation of computational methodologies into the realm of cancer drug discovery signifies a fundamental change, presenting novel solutions to conventional obstacles and facilitating the development of cancer therapies that are both more productive and streamlined.
The advent of computational methods for drug discovery has opened new horizons in personalized medicine, particularly in the field of cancer treatment. Computational approaches are increasingly being used to tailor cancer therapies to individual patients, considering their unique genetic makeup and disease characteristics [
124]. Through the utilization of computational methods such as genetic data analysis and patient-specific simulation models, scientists can forecast the distinct responses of individual patients to a variety of anticancer medications. Particularly crucial in oncology, where the genetic diversity of malignancies can substantially impact therapeutic results, is an individualized approach. By enabling the identification of particular biomarkers that direct the selection of the most efficacious treatment for each patient, computational approaches eliminate the trial-and-error approach, which is frequently associated with cancer therapy. The transition towards personalized medicine holds the potential to enhance treatment effectiveness and patient outcomes, while concurrently reducing adverse effects and elevating the overall quality of life for patients with cancer. Cancer therapy is being revolutionized by the use of computational technologies in personalized medicine, resulting in enhanced precision, efficacy, and patient-centeredness [
125,
126].
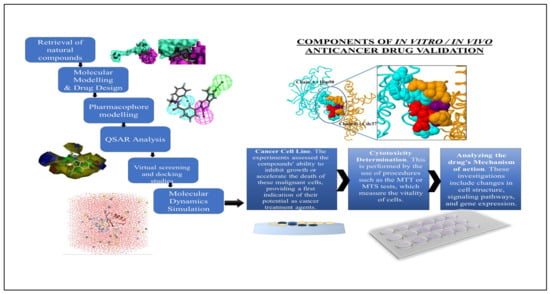
5.1. Molecular Modelling and Drug Design
Through the implementation of molecular modeling, computational methods have substantially transformed drug development procedures. This method is implemented by producing, modifying, or expressing three-dimensional structures of molecules and evaluating the physicochemical attributes associated with them. Chemical modeling enables medicinal chemists to predict the molecular and biological characteristics of therapeutic molecules, which is a significant asset in drug design [
127,
128]. Predicting molecular interactions is an essential component of molecular modeling. This requires modeling the potential interaction between a pharmacological molecule and its target, which may be an enzyme or protein within the body. Medicinal chemists can discern prospective binding sites and predict the characteristics and potency of these interactions through this process. This stage is critical for evaluating the safety and effectiveness of a potential medicine prior to its synthesis and laboratory testing [
129,
130]. The concept of drug designing via a computational method is illustrated in
Figure 4.
Figure 4. The discovery of natural compounds undergoes various stages, which include computational methods and the validation. The computational methods follow sequential steps that involve retrieval of natural compounds, molecular modelling, pharmacophore modelling, QSAR analysis, virtual screening and molecular dynamic simulation. Based on the binding scores, the top natural compounds against the molecular target will be further validated under the in vitro and in vivo cancer model.
Another noteworthy attribute of computational approaches in the realm of drug creation is their capacity to screen extensive collections of molecules rapidly. Complementary to high-throughput screening (HTS) methodologies, computer methods provide rapid evaluation of thousands of molecules. This technique considerably expedites the initial phases of drug discovery, by identifying promising candidates that warrant further research [
130]. In addition, computational techniques play an important role in the enhancement of potential pharmaceuticals. By modifying the structure of a molecule using structure–activity relationship (SAR) analysis, chemists are able to augment its medicinal qualities, including, but not limited to, greater potency, decreased toxicity, and enhanced pharmacokinetic profiles. This optimization is essential for the development of safe and efficacious pharmaceutical products [
130].
Furthermore, there is a growing trend to employ molecular modeling and computational techniques to predict the pharmacokinetics and pharmacodynamics of potential drugs. These predictions facilitate the comprehension of the physiological actions of medication throughout the human body, encompassing its distribution, excretion, and metabolism. Such data are crucial for determining whether a medicine will be successful in clinical trials [
129]. The value and efficacy of molecular modeling in drug development cannot be overstated. This increases the probability of identifying effective and safe medications, provides a more comprehensive understanding of molecular interactions at the atomic level, and decreases the time and expense associated with conventional drug development techniques. Furthermore, with the progress of technology, these computational techniques persistently enhance complexity, facilitating more precise prognostication and streamlined medication-creation procedures [
131,
132].
An exemplary illustration of its utilization is in the development and refinement of innovative curcumin analogs that hold promise as anticancer medicines. Curcumin, an antioxidant, anticancer, and natural polyphenol derived from the rhizome of Curcuma longa, is well known for its properties. However, its chemical instability and low absorption impede its practical use. To address these obstacles, medicinal chemists have resorted to using molecular modeling methodologies to develop and refine curcumin analogs [
128,
133].
Molecular modeling methodologies, such as molecular dynamics simulations and docking studies, are crucial for forecasting the binding mechanism and affinity of curcumin analogs towards their respective target proteins. The enhanced binding ability of these improved curcumin analogs for targeting proteins increases their potential as medicines against cancer [
133].
Research conducted by Cao et al. exemplifies this methodology. An assortment of innovative mono-carbonyl curcumin derivatives was formulated and manufactured, and their efficacy against hepatocellular carcinoma was assessed via in vitro and in vivo investigations [
127]. In anti-proliferation experiments, G2 emerged as the most powerful derivative, relative to curcumin. Additional research employing molecular docking, wound healing, transwell, JC-1 staining, and Western blotting techniques revealed that G2 possesses the ability to impede apoptosis and cell migration by manipulating the expression of apoptosis-related proteins and impeding the phosphorylation of AKT [
127]. Additionally, the effectiveness of G2 was verified in a xenograft model using HepG2 cells; H&E staining confirmed that it inhibited tumor development more effectively than curcumin [
127].
In summary, molecular modeling is indispensable in the field of drug design. This facilitates the accurate prediction of the chemical and biological characteristics of drug compounds by medicinal chemists. By creating and optimizing new curcumin analogs as possible anticancer medicines, the application of molecular modeling tools demonstrates how this methodology may result in the creation of more powerful medications by improving their binding to target proteins.