Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Obstetrics & Gynaecology
Childbirth is a remarkable, life-changing process and is frequently regarded as an excruciating, physically and emotionally demanding experience that women endure. Labor pain management poses a significant challenge for obstetricians and expectant mothers.
- non-pharmacological pain management
- pregnancy
- mothers
- labor
- obstetrician efficacy
1. Introduction
Historically, labor pain has been recognized as an inherent part of childbirth, although approaches to its management have varied across cultures and time periods [1]. With the advent of modern medicine, the focus shifted toward pharmacological interventions. By the late 19th century, interventions such as chloroform and ether were used for labor pain, followed by the introduction of “twilight sleep” in the early 20th century—a combination of morphine and scopolamine that induced a state of semi-consciousness [2,3].
In the latter half of the 20th century, advances in anesthesia led to the widespread use of regional analgesics, such as epidurals and spinal blocks, for labor pain [4]. These methods became the gold standard in many high-income countries due to their effectiveness in reducing pain [5]. In recent decades, the use of opioids such as fentanyl and morphine has also become common [6]. Although they do not eliminate pain, they can help to make it more manageable. However, pharmacological pain management methods (PPM) have been associated with various side effects and risks despite their effectiveness. For example, epidurals can lead to a drop in blood pressure, fever, and a raised need for assisted delivery [7]. Moreover, they lengthen the labor’s duration. Opioids induce nausea and affect the neonate (breathing and heart tracing) if admitted too soon [8,9]. Pain is the norm of childbirth; reducing pain via drugs makes laboring women lose essential feedback, potentially leading to more prolonged labor or increased intervention. Some forms of PPM reduce a woman’s motility or the ability to take different positions to alleviate discomfort; this lack of control over pain is distressing to women [10]. Over the past few decades, a growing interest has been expressed in revisiting non-pharmacological pain management techniques (NPPM) to reduce labor pain [11,12]. This shift is driven by a confluence of factors, including increasing evidence of pharmacological interventions’ side effects and risks. Additionally, there has been a broader societal shift towards more patient-centered and holistic healthcare, emphasizing personal autonomy, shared decision-making, and natural and complementary therapies [13]. These trends have led to an increased interest in NPPM, which relieves pain and empowers women to actively engage in the birth experience. NPPMs have demonstrated encouraging outcomes in diminishing pain intensity and enhancing satisfaction and are commonly regarded as safe, with minimal adverse effects compared to pharmacological interventions [3,5,8].
2. Understanding Pain in Labor
The nature of pain experienced during labor undergoes modifications as the process progresses. During the first stage of labor, the primary source of pain is visceral in nature, originating mostly from the cervix, uterus, and adnexa. This pain is mediated by sympathetic fibers that transmit signals to the ganglia of the posterior nerve roots located at the T10-L1 spinal levels [5]. During the late first stage and early second stage of labor, pain arises from the distention and traction of the pelvic organs. The pudendal nerve is responsible for transmitting pain signals to the ganglia of the posterior nerve roots located at spinal levels S2 to S4. During the second stage of labor, the sensation of pain is elicited by the stretching of the perineal structures as the fetus descends [5,11]. Comprehending the complexities of labor pain goes beyond the physiological aspects; it necessitates an understanding of psychological and socio-cultural elements. It is crucial to grasp the multifaceted nature of labor pain to assess NPPM better. From a physiological standpoint, uterine contractions and cervical dilation are the main causes of labor pain, because they activate pain receptors (nociceptors) and send signals to the brain [11]. The intensity of labor pain can vary greatly among women, between different labors in the same woman, and it is affected by various factors such as the baby’s position, size, and the speed of labor [12]. On a psychological level, labor pain is influenced by a woman’s emotions, expectations, and previous experiences [13,14]. Fear and anxiety can heighten pain perception by increasing tension and resistance. As confidence, relaxation, the feeling of control in their labor, and continuous support are all less likely to result in severe pain, the women are more likely to cope and have a positive birth experience [15,16,17,18]. Psychological preparation for childbirth can reduce the need for analgesia and increase satisfaction with pain management [19,20]. Socio-cultural factors, cultural beliefs, and societal attitudes toward childbirth can influence a woman’s expectations and coping strategies. In some cultures, labor pain is viewed as a natural and empowering part of childbirth, while in others, it is seen as something to be avoided or feared [21,22]. Furthermore, social support is crucial during labor. Having a supportive companion can significantly improve a woman’s experience of pain and reduce her need for pharmacological analgesia [23,24].
3. Categorization of Non-Pharmacological Methods for Pain Relief in Labor
These can be categorized based on the mechanisms of action into physical, psychological, and complementary techniques.
3.1. Physical Modalities
There are several physical methods listed under NPPM during labor. These methods include massage, pressure on precise anatomical locations, Transcutaneous Electrical Nerve Stimulation (TENS), water immersion, heat and cold therapy, breathing techniques, positioning, and movement [28,29]. The sub-types of each method, mechanism of action, perceived benefits, and supporting references are all summarized in Table 1.
Table 1. Non-pharmacological pain management in labor: An in-depth analysis of physical modalities concerning the mechanism of action, perceived benefit, and the supporting references.
| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Massage |
|
|
|
Pawale et al. [30]; 2020 Silva Gallo et al. [31]: 2013 Eskandari F et al. [32]; 2022 |
| Pressure on precise anatomical locations |
|
|
|
Smith et al. [33]; 2020 Schlaeger et al. [34]; 2017 Eshraghi et al. [35]; 2021 |
| Transcutaneous Electrical Nerve Stimulation (TENS) |
|
|
|
Thuvarakan et al. [36]; 2020 Gibson et al. [37]; 2019 Daniel et al. [38]; 2021 |
| Water immersion |
|
|
|
Cluett et al. [39]; 2018 Carlsson et al. [40]; 2020 Cooper et al. [41]; 2022 |
| Heat therapy |
|
|
|
Goswami et al. [42]; 2022 Akbarzadeh et al. [43]; 2018 Akbarzadeh et al. [44]; 2016 Dastjerd et al. [45]; 2023 |
| Cold therapy |
|
|
|
Shirvani et al. [46]; 2014 Emine et al. [47]; 2022 Serap et al. [48]; 2022 |
| Breathing techniques |
|
|
|
Baljon et al. [49]; 2022 Issac et al. [50]; 2023 Yuksel H et al. [51]; 2017 Boaviagem et al. [52]; 2017 |
| Positioning and Movement |
|
|
|
Huang et al. [53]; 2019 Ondeck et al. [54]; 2019 Borges et al. [55]; 2021 Ali SA et al. [56]; 2018 |
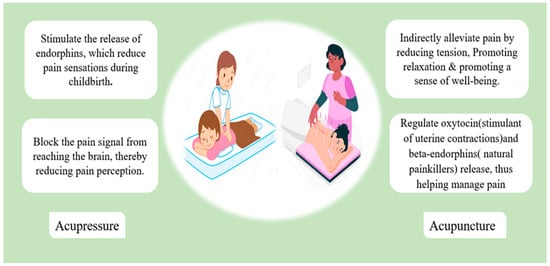
Figure 2. The mechanisms that underlie acupressure’s positive effect in reducing labor pain.
3.2. Psychological Techniques
Cognitive Behavioral Therapy (CBT) aims to identify and modify maladaptive thoughts, emotions, and behaviors. Moreover, CBT assists individuals in cultivating a perception of control in managing pain, fostering the acquisition of pain-coping strategies, and enhancing self-esteem [57]. CBT was used to manage labor pain; there was inconsistency in the reported literature; some discussed reduced psychological aspects of pain and improved satisfaction [58]. However, pain medication was still needed.
Others have discussed how CBT techniques significantly reduced pain intensity and labor duration [57].
Cognitive behavioral therapy helps individuals have a sense of control in coping with pain, develop pain-coping behaviors, and increase self-respect [57,59]. The main methods of CBT include:
-
Relaxation techniques;
-
Virtual reality (VR);
-
Music;
-
Distraction technique.
The main mechanism and benefits of each are summarized in Table 2.
Table 2. Summary of non-pharmacological pain management in labor: An in-depth analysis of psychological modalities, concerning the mechanism of action, perceived benefit, and the supporting references.
| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Relaxation technique |
|
Progressive muscle relaxation, guided imagery, and visualization have been found to be effective in mitigating anxiety and fostering tranquility throughout labor. |
|
Smith et al. [15]; 2018 Zhang et al. [60] Jahdi et al. [61]; 2017 |
| Virtual reality (VR) |
|
|
|
Massov et al. [62]; 2021 Musters et al. [63]; 2023 Baradwan et al. [64]; 2022Xu et al. [65]; 2022 |
| Music | -- |
|
|
Timmerman et al. [66]; 2023 Estrella-Juarez et al. [67]; 2023 Chehreh et al. [68]; 2023 García González et al. [69]; 2018 |
| Distraction |
|
|
|
Ireland et al. [70]; 2016 Amiri et al. [71]; 2019 Melillo et al. [72]; 2022 |
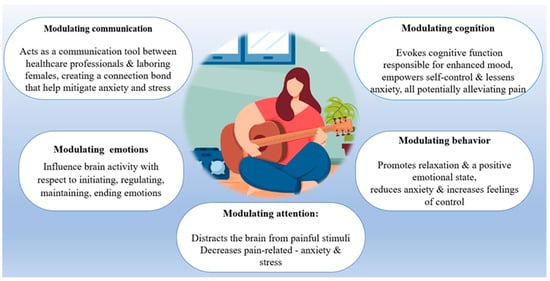
Figure 3. The main pathways by which music conducts its beneficial effect in alleviating labor pain.
3.3. Complementary and Alternative Approaches
Over the past decade, there has been a growing scholarly focus on literature examining the role of Complementary and Alternative Approaches (CAA) in mitigating pain during childbirth [73]. CAA exhibits a higher prevalence among women within the reproductive age range [74]. The utilization of this intervention during childbirth is quite prevalent, as indicated by a survey conducted in Australia, with a reported rate of 75% [75]. Complementary and Alternative Medicine is a term employed by the U.S. National Center for Complementary and Integrative Health to denote a range of practices that can be utilized in conjunction with conventional and established medical care (complementary) or as a substitute for it (alternative) [76]. An in-depth analysis of complementary and alternative approaches concerning the mechanism of action, perceived benefit, and the supporting references [77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92] are summarized in Table 3.
Table 3. Summary of non-pharmacological pain management in labor: An in-depth analysis of complementary and alternative approaches concerning the mechanism of action, perceived benefit, and the supporting references.
| Methods | Methods Sub-Types | Proposed Mechanism of Action | Perceived Benefit | Authors’ Name; Publication Year |
|---|---|---|---|---|
| Hypnosis |
|
|
|
Madden et al. [77]; 2016 Cyna et al. [78]; 2013 Downe et al. [79]; 2015 |
| Integration of religion/health and well-being |
|
|
|
McLaren H et al. [80]; 2021 Desmawati et al. [81]; 2019 Kocak et al. [82]; 2022 |
| Dancing | -- |
|
|
Abdolahian et al. [83]; 2014 Akin et al. [84]; 2020 |
| Aromatherapy | Essential oils may be given as:
|
|
|
Tabatabaeichehr et al. [85]; 2020 Sirkeci et al. [86]; 2023 Hamdamian et al. [87]; 2018 |
| Photomodulation | -- | Irradiation induces.
|
|
Traverzim et al. [88]: 2021 Traverzim et al. [89]; 2018 |
| Support therapy |
|
|
|
Akbas et al. [90]; 2022 Bohren et al. [91]; 2017 Ip et al. [92]; 2009 |
This entry is adapted from the peer-reviewed paper 10.3390/jcm12237203
This entry is offline, you can click here to edit this entry!
