Mirizzi syndrome is a complication of gallstone disease caused by an impacted gallstone in the infundibulum of the gallbladder or within the cystic duct, causing chronic inflammation and extrinsic compression of the common hepatic duct or common bile duct. Eventually, mucosal ulceration occurs and progresses to cholecystobiliary fistulation. Numerous systems exist to classify Mirizzi syndrome, with the Csendes classification widely adopted. It describes five types of Mirizzi syndrome according to the presence of a cholecystobiliary fistula and its corresponding severity, and whether a cholecystoenteric fistula is present.
1. Introduction
Obtaining a diagnosis of Mirizzi syndrome is crucial in a preoperative setting as it has a major impact on management, morbidity, and mortality [
7,
8,
33,
41]. The incidence of bile duct injuries in patients operated on with undiagnosed Mirizzi syndrome can be as high as 17% [
8]. However, obtaining a preoperative diagnosis can be difficult and it can be made in only 8% to 62.5% of patients [
30,
31,
42]. This statistic was shown to increase to 85.9% [
21] when both magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) were used in combination. A combination of both MRCP and computed tomography (CT) yielded a sensitivity of 96%, specificity of 93.5%, and diagnostic accuracy of 94% [
43]. Hence, most surgeons prefer to use at least two diagnostic modalities in combination [
5,
21]. However, this practice has not been validated by evidence [
44].
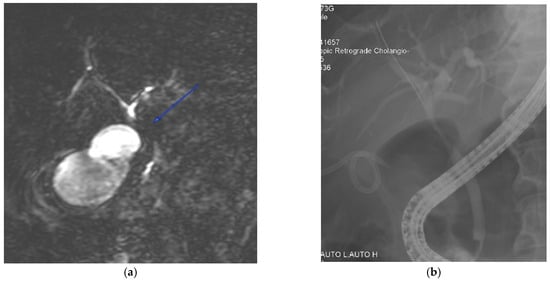
Figure 1 presents a case vignette with the aid of MRCP and ERCP images, illustrating the difficulty in differentiating Mirizzi syndrome from other pathologies such as biliary malignancy.
Figure 1. A 72-year-old male was admitted with a clinical presentation suggestive of acute cholangitis. (a) Magnetic resonance imaging demonstrates a hilar stricture (labelled) with suspicion of cholangiocarcinoma. In view of concomitant cholecystitis and the need to evaluate for suspected malignancy, percutaneous gallbladder drainage was performed. (b) A percutaneous cholecystostomy tube is visible, and an endoscopic cholangiogram shows a smooth biliary stricture with brushings that do not show malignant cells. The patient was managed with open cholecystectomy, choledochectomy, and hepaticojejunostomy. The final histology was a benign biliary structure with cholecystitis.
2. Ultrasonography
Findings on an ultrasound examination of the hepato-biliary system may include an atrophic gallbladder with thick or extremely thick walls, with one large or multiple small impacted gallstones in the infundibulum or cystic duct [
45]. Other findings include a dilated intrahepatic biliary tree and CHD above the level of obstruction, with a CBD of normal diameter [
8,
15,
21,
27,
45]. The sensitivity of ultrasound examination ranges from 8 to 57% [
7,
8,
9,
22,
46,
47], with a reported diagnostic accuracy of 29% [
30]. Regional inflammation and bowel gas may further limit the sensitivity of the study. Despite the low diagnostic accuracy of ultrasonography, it is often used as a cost-effective preliminary routine investigation, as Mirizzi syndrome is not always suspected even in patients with jaundice [
5,
21].
3. Computed Tomography (CT)
CT scans are useful to rule out hepatic or biliary malignancies in the porta hepatis, or other aetiologies of biliary obstruction [
8,
9,
21,
36]. It is a suitable modality for evaluating extraluminal causes of biliary compression. However, there are no specific CT findings for Mirizzi syndrome. CT is reported to have a 31–50% sensitivity [
7,
22,
46,
48]. A limitation of CT is that it often does not demonstrate biliary calculi [
49]. The presence of periductal inflammation can be misinterpreted as carcinoma of the gallbladder [
15]. Though CT scans are not optimal to detect stones, they adequately visualise inflammatory fat stranding, ductal dilatation, and gallbladder wall thickening. In addition, the scan provides an idea of the dimensions of the gallbladder with some perspective on the chronicity, fibrosis, and shrunken-ness of the gallbladdery. Aerobilia, if evident, without previous biliary instrumentation suggests cholecystobiliary or cholecystoenteric fistulation.
4. Magnetic Resonance Cholangiopancreatography (MRCP)
MRCP is the preferred imaging modality to assess biliary anatomy and the presence of biliary calculi. Although the reported diagnostic accuracy of MRCP is 50% [
30], it has a sensitivity of 77.8–100% in the diagnosis of Mirizzi syndrome [
8,
16,
27,
46,
50]. It is regarded as the preferred non-invasive imaging modality for the diagnosis of Mirizzi syndrome [
22]. MRCP findings in Mirizzi syndrome include dilatation of the intrahepatic bile ducts, narrowing of the CHD, and gallstone(s) in the cystic duct [
49]. MRCP can also rule out other causes of bile duct obstruction, such as choledocholithiasis, or be used to assess inflammation around the gallbladder [
9]. Though MRCP is a non-invasive modality, ERCP has increased accuracy to diagnose a cholecystobiliary fistula [
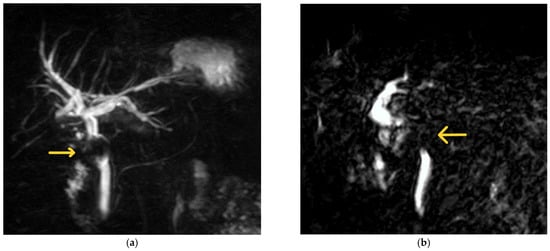
51]. MRCP images from patients with Mirizzi syndrome are shown in
Figure 2 for illustration.
Figure 2. Examples of MRCP findings in Mirizzi syndrome. (a) The first MRCP shows a filling defect (labelled) caudal to the confluence of the hepatic ducts with upstream biliary dilatation. The patient was a 67-year-old female with a background of Mirizzi syndrome treated with laparoscopic subtotal cholecystectomy at another hospital 10 months prior. She was subsequently diagnosed with a retained 19 mm cystic duct stone with a fistula in the CHD (Csendes Type III Mirizzi syndrome) and underwent laparoscopic CBD exploration with primary repair. (b) The second image illustrates an abrupt cut-off at the level of the CHD with a filling defect (labelled). This was taken from a 70-year-old man whose initial presentation of Mirizzi syndrome was that of acute pyogenic cholangitis. He subsequently underwent ERCP with biliary stenting, followed by laparoscopic CBD exploration, biliary stent removal, and primary closure of the CBD 8 weeks later.
5. Endoscopic Retrograde Cholangiopancreatography (ERCP)
Despite its invasive nature, ERCP is still the gold standard for the diagnosis of Mirizzi syndrome. ERCP has a sensitivity of 50–100% [
3,
30,
46,
50], with a diagnostic accuracy of 55–90% [
30,
42]. ERCP provides superior visualisation of the extrahepatic bile ducts, and can identify extrinsic biliary compression and the presence of a cholecystobiliary or cholecystoenteric fistula [
5,
36].
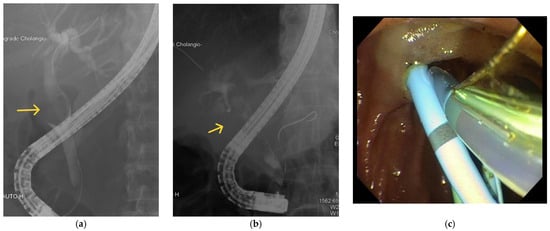
Figure 3 illustrates examples of images taken using ERCP. Biliary stenting or stone retrieval can also be offered to relieve obstruction, giving ERCP the advantage of being both a diagnostic and therapeutic procedure [
51]. An example of biliary and pancreatic stenting during ERCP is shown in
Figure 3c. The use of endoscopic ultrasound prior to ERCP to further evaluate the bile ducts and pancreas was demonstrated in a patient with Mirizzi type I by Rayapudi et al. [
52], while some studies have used intraductal ultrasonography during ERCP to delineate defects in the ductal mucosa to localise cholecystobiliary fistulas and to differentiate causes of biliary strictures [
53,
54].
Figure 3. Examples of ERCP findings in Mirizzi syndrome. (a) There is a filling defect (labelled) seen in the CBD. (b) There is a filling defect (labelled) in the CHD. (c) Biliary and pancreatic stenting during ERCP.
The main disadvantage of ERCP is the risk of major complications. These include pancreatitis (3.5%), haemorrhage (1.3%), cholangitis (1%), perforation (0.1–0.6%), and the associated cardiopulmonary complications of sedation [
55]. ERCP is best reserved as a therapeutic modality to clear biliary stone disease burden, decompress the biliary system in the presence of sepsis, and obtain biliary brushings or cytology in patients who have strictures which are suspected to be malignant.
6. Percutaneous Transhepatic Cholangiography (PTC)
PTC may be performed as a diagnostic investigation, usually in cases where ERCP failed [
5]. Percutaneous biliary drainage can be performed in the same setting. PTC can also be used in cases with previous bilioenteric anastomosis or intrahepatic dilation with a high obstruction [
56]. However, PTC is rarely used as a diagnostic tool.
This entry is adapted from the peer-reviewed paper 10.3390/medicina60010012