Wounds have plagued patients for millennia, imposing a substantial burden on their carers, thus earning its designation as the ‘silent epidemic’ [
1]. Approximately 4 million cutaneous wounds have been documented to occur annually in affluent countries, with the number in developing nations in ascendance [
2]. Skin injury compromises the integrity of the skin’s framework, leading to a wound healing process that is characterized by a well-coordinated series of cellular and molecular reactions that aim to recuperate or replace the injured tissue [
3]. Wounds distinguished by synergistic and ordered processes, which lead to uninterrupted wound regeneration, are commonly referred to as ‘acute wounds’. Although minor cutaneous injuries can recuperate, several variables frequently impact wound rehabilitation. These include severe oxidative stress, infection, and underlying medical conditions that result in the development of “chronic or inert wounds” [
4]. Chronic wounds exhibit distinctive attributes, which include recurrent infections, a heightened inflammatory phase, and impaired responsiveness of epidermal cells to reparative signals [
5].
Hydrogels can be described as intricate three-dimensional structures composed of hydrophilic polymer chains and exhibit a quick swelling response upon contact with water, forming a partially solid material [
7]. More than 90% of the hydrogel framework is composed of water, thereby rendering it possible to sustain a moist environment adjacent to the wound’s surface, facilitating tissue repair [
4]. Hydrogels possess numerous properties that make them ideal for use as wound dressings. These include firm adhesion, shape adaptability, and mechanical protection, which enable sufficient coverage and safeguarding of the wound [
8]. Hydrogel-based dressings possess the advantage of being readily tuneable, allowing for the incorporation of antibacterial and antimicrobial agents, cells, biomolecules, and growth factors [
9]. This augmentation aims to expedite the processes of wound contraction and healing. A hydrogel can be constructed using any hydrophilic polymer through a tailored cross-linking technique. These water-soluble polymers can be natural or synthetic. Synthetic materials provide unique features pertaining to their highly modifiable physical attributes and adhesive characteristics. Natural polymers exhibit enhanced biocompatibility and biodegradability compared to synthetic polymers [
10]. There has been notable progress in combining natural and synthetic polymers to formulate blended hydrogels. Additionally, integrating nanomaterials in situ has led to the formation of “smart” nanogels that possess a customized functionality, facilitating the application of hydrogels in treating deep or irregular wounds due to in situ induction [
11].
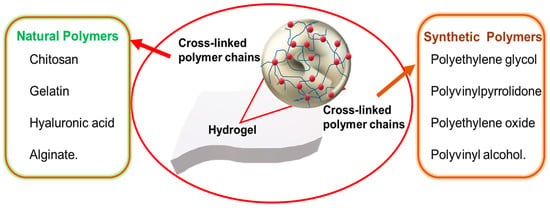
Hydrogel wound dressings are developed using diverse natural and synthetic polymers (Figure 1). Natural polymers include chitosan, gelatin, hyaluronic acid, and alginate. Synthetic polymers include polyethylene glycol, polyvinyl pyrrolidone, polyethylene oxide, and polyvinyl alcohol. Hydrogels can be highly elastic, and this reduces mechanical power; therefore, multipolymeric hydrogels have been introduced for improved mechanical power and absorption. Combining a naturally occurring polymer with a synthetic polymer promises to be a viable approach for generating materials with the desired thermal and mechanical attributes. Advancements in the field have been achieved by harnessing the inherent features of polymers, leading to the development of novel technologies such as sprayable hydrogels, “smart hydrogels”, nanogels, aerogels, and cryogels.
Figure 1. Natural and synthetic polymers being used in hydrogel dressings.
2. Natural Hydrogels
Natural hydrogels primarily comprise proteins and ECM constituents, rendering them intrinsically biocompatible, bioactive, and potentially well suited for various biomedical applications due to their ability to enhance numerous cellular activities [
53]. The makeup and attributes of these materials resemble the inherent characteristics of tissue layers. Nevertheless, they are subject to some restrictions, primarily from the challenges associated with their manipulation arising from variations observed between different batches. Hydrogel variants exhibit unique properties that render them more appropriate for their proposed purpose. We shall briefly discuss the various natural hydrogels.
2.1. Chitosan
Chitin is the primary building block of arthropod exoskeletons. It is partially deacetylated to make chitosan, a linear polysaccharide of beta (1-4)-linked D-glucosamine and N-acetyl-D-glucosamine groups. Chitosan exhibits a structural resemblance to glycosaminoglycans inside the ECM. The molecular weight and level of deacetylation of chitosan have a direct relationship with its physical and mechanical characteristics [
54]. Chitosan possesses a cationic charge and exhibits specific antimicrobial activity through electrostatic interactions [
55]. Its positive charge has made it a polymer of choice for coating nanoparticles for enhanced stability [
56,
57]. The potential advantages of chitosan-based hydrogels in wound healing applications include the creation of a hydrated wound environment, protection from infections, promotion of leukocyte activity for wound exudate disposal, regulation of degradation through a change in the level of deacetylation, and a reduction in scar tissue [
58]. These properties highlight the significant promise of chitosan in wound healing. The susceptibility of the hydrogel to external factors, such as pH and temperature, can be attributed to the presence of hydroxyl and amino groups. One of the drawbacks associated with this material is its suboptimal mechanical strength and challenges in manufacturing fibrous wound dressings [
53]. Nevertheless, this issue can be effectively addressed by implementing cross-linking techniques. The most prominent cross-linking technique is the utilization of glutaraldehyde or genipine cross-linkers, which will typically embed themselves between chitosan polymer chains by cross-linking with the amino groups of chitosan. Another method often utilized is the cross-linking of chitosan with tripolyphosphate (TPP). The phosphates present in TPP ionically bind to the amine groups of the chitosan through a process known as ionic gelation [
59].
An injectable chitosan-based hydrogel for repairing wounds has been reported. This hydrogel exhibited antimicrobial activity against bacterial strains
Pseudomonas aeruginosa and
Staphylococcus aureus, with a terminating efficiency of 96.4% and 95.0%, respectively. Hydrogel-treated wounds showed 99.8% sealing after two weeks. Evaluation of the hydrogel’s hemostatic properties demonstrated prompt attachment to the adjacent tissue of the bleeding region, thereby establishing a protective covering that mitigated hemorrhaging [
60]. Hence, hydrogels derived from chitosan can promote the healing of wounds as well as the prevention of infection. Recently, an injectable carboxymethyl chitosan (CMCS) hydrogel to modulate cellular responses and facilitate the complete recovery of diabetic wounds was developed. CMCS was synthesized by modifying chitosan to improve its solubility in water. The CMCS hydrogel exhibited a significant swelling rate of 132% at 37 °C. This property enabled it to efficiently soak up a substantial quantity of tissue exudate and regulate the moisture levels at the lesion. The hydrogel was administered intradermally into the wounds of mice with diabetes. The hydrogel promptly attached to the location of the wound, effectively halting hemorrhaging and establishing a favorable environment for the healing process, which took 14 days for 99% wound healing [
61]. Hence, it can be concluded that hydrogels constructed from carboxymethyl chitosan exhibit properties that closely resemble the conditions of the ECM, demonstrating their efficacy in wound healing.
2.2. Gelatin
Gelatin is a renowned, naturally occurring, inexpensive vascular polymer with beneficial features for tissue development, including low immunogenicity and significant degradability. Gelatin is derived by disrupting the triple helical structure of collagen, resulting in the development of the sequence of amino acids known as RGD (Arg/Gly/Asp). This sequence can facilitate the adhesion of cells and create a favorable environment for cell proliferation. This material’s fibroblast adhesion, proliferative features, and low antigenicity render it highly promising for clinical use [
62]. Nevertheless, its suboptimal strength and susceptibility to breakage constrain its utility as a hydrogel treatment. Therefore, this hydrophilic protein requires cross-linking [
63]. Gelatin has also been employed as an adhesive for coating to enhance cell adhesion, serving as a method for facilitating the regrowth of vascular tissues. The absorption of wound exudates and moisture maintenance by porous gelatin matrices contribute to the facilitation of wound recovery. Despite its potential as a biopolymer for wound healing applications, gelatin lacks antibacterial properties that could effectively avoid infections. Therefore, it is typically combined with antibacterial agents or hybrid polymers [
64]. Gelatin is often cross-linked with aldehydes, such as glutaraldehyde and formaldehyde, similar to chitosan, due to the presence of amino groups. An alternative method is to use cross-linkers such as 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide hydrochloride (EDC), that are not incorporated into the gelatin matrix. EDC activates the carboxyl groups present in gelatin, which then undergoes a direct reaction, forming bonds with the adjacent amino groups [
65].
Wang and coworkers (2023) developed a bilayer gelatin hydrogel with photothermal properties to eradicate biofilms and provide extensive therapy for chronic wounds. To enhance the attachment and growth of fibroblasts, gelatin methacryloyl (GelMA) with favorable rigidity was synthesized via optical cross-linking on the outermost layer of the hydrogel. In the interim, epidermal growth factor (EGF) was introduced into GelMA to enhance tissue repair and re-establish the wound’s epithelial layer. Scanning electron microscopy (SEM) revealed a significant reduction in the biofilm layer within the lesion after photothermal therapy. Following a 12-day treatment period, the
Escherichia coli-afflicted wound exhibited a reduction to a mere 7.9% of its initial area [
66].
2.3. Hyaluronic Acid
Hyaluronic acid (HA) is a glycosaminoglycan lacking sulfonate groups and is a naturally occurring anionic polysaccharide. It comprises a series of disaccharides, specifically β-D-glucuronic acid and N-acetyl-D-glucosamine, interlinked by alternate β-1, 3, and β-1, 4-glucosidic linkages. HA is found within the vitreous humor of humans, umbilical cords, and connective tissues and is synthesized via fermentation by microbes [
67]. HA does not undergo hydrogel formation through conventional physical cross-linking methods. However, it is worth noting that this polymer can undergo chemical modifications in its hydroxyl and carboxyl moieties. As a result, it is widely used in the construction of hydrogels, making it one of the most commonly employed polymers. The hydrophilicity of hyaluronic acid can be attributed to the presence of these functional groups, and this characteristic allows it to soak up exudate and enhance cell adhesion efficiently [
68]. A widely used cross-linking method for HA is through the formation of thiol-modified HA hydrogels. This cross-linking system entails the conjunction of oxidised glutathione with an HA-based hydrogel through a thiol-disulfide exchange reaction. The thioether–sulfone bond is highly stable and not susceptible to hydrolysis, making it suitable for hydrogel formation [
69]. Hydrogel wound dressings based on HA exhibit notable features that make them a good option for addressing all four phases of wound healing. These characteristics encompass a reduction in inflammation, an amplification of angiogenesis, and the promotion of endothelial cell growth [
70].
Li et al. (2022) developed a hydrogel that used HA as its primary constituent. HA was cross-linked using benzaldehyde-functionalized PEG co-polyglycerol caprate (PEGSB) to form a hydrogel with both elasticity and regeneration abilities. The aldehyde group of PEGSB can undergo a chemical reaction with those found in the wounds, thereby facilitating adequate adhesion. A three-minute exposure to near-infrared (NIR) irradiation at 808 nm effectively eradicated
Escherichia coli and methicillin-resistant
Staphylococcus aureus (MRSA). After a 14-day therapy regimen targeting hip wounds in mice, a near-complete healing of the lesion was observed. The hydrogel showed promise for practical use in the treatment of infections in wounds due to its excellent biocompatibility [
71].
2.4. Alginate
Alginate is a polymer found in brown algae cell walls and certain bacteria capsules. Its structure is built from blocks of two distinct monomers, D-manuronate (M) and L-glucuronate (G). Alginate’s substantial G block concentration may produce stiff hydrogels when bound to divalent cations like Ca
2+. This is referred to as the “egg-box model”. Alginate with an elevated M block concentration demonstrates reduced adhesiveness and immunostimulatory properties [
72]. The calcium ions in an alginate-containing dressing exchange with sodium ions as they come into contact with the exudate from the wound. The alginate fibres undergo expansion, partial dissolution, and solidification, forming a protective coating that facilitates wound repair [
73]. A direct method of cross-linking is typically utilized, where alginate is directly treated with calcium chloride, calcium sulphate, or calcium carbonate. Internal gelation occurs upon mixing as the cations penetrate the alginate gel through diffusion. Divalent ionic bonding with zinc oxide has also been a notable cross-linking method, as it provides antibacterial properties [
74]. Alginate can activate macrophages and promote the production of interleukin-6 (IL-6) and tumor necrosis factor α (TNF-α) by monocytes, thereby accelerating chronic wound healing. Dry alginate dressings can soak up wound fluids, resulting in the formation of gels. These gels subsequently release water, which can benefit the hydration of dry wounds. The gelation property of alginate facilitates the painless and safe removal of dressings [
75]. Multiple commercial hydrogels have alginate as the primary component (
Table 1).
Table 1. Some commercially available hydrogels for wound healing [
5].
| Product |
Company |
Constituent |
Use |
| DermaSyn® |
DermaRite
Industries (NJ, USA) |
Primary wound dressing with vitamin E |
Partial and full-thickness
chronic wounds |
Neoheal®
Hydrogel |
Kikgel |
Polyethylene glycol,
polyvinylpyrrolidone, Agar,
and 90% water |
Low-exuding scabs, a
abrasions, dry scabs, first, second-and third-degree burns, and ulcers |
Restore
Hydrogel |
Hollister Inc.
(IL, USA) |
Gauze pad, Hyaluronic acid |
Partial and full-thickness
chronic wounds |
| ActivHeal® |
Advanced Medical
Solutions Ltd.
(Oxon, UK) |
Primary wound dressing
with 85% water |
Cavity wounds, pressure ulcers,
diabetic foot ulcers, and leg
ulcers |
| NU-GEL™ |
Systagenix |
Sodium alginate primary
wound dressing |
Diabetic foot ulcers, leg ulcers,
venous ulcers |
| Purilon® |
Coloplast |
Calcium alginate, sodium
carboxymethyl cellulose |
Pressure ulcers, first and second
degree burns, non-infected
diabetic foot ulcers, leg ulcers |
Simpurity™
Hydrogel |
Safe n’ Simple |
Acrylate, polyvinyl alcohol,
polyethylene oxide,
polyurethane |
First and second-degree partial-
thickness burns, low-exuding
chronic wounds |
To improve the repair of wounds, a dual-network hydrogel using platelet-rich plasma (PRP) and sodium alginate (SA) was synthesized using a thrombin activation method. The presence of epidermal growth factor (EGF) and vascular endothelial growth factor (VEGF) was observed in a hydrogel maintained in phosphate-buffered saline (PBS), suggesting the potential for cellular growth and the redevelopment of blood vessels. The hydrogel showed efficacy in promoting wound closure when administered directly to the cutaneous wounds of rats [
76]. Using alginate hydrogels presents a viable strategy for addressing the limitations associated with traditional wound dressings.
3. Synthetic Hydrogels
Synthetic polymers have demonstrated considerable efficacy in biomedical applications due to their mechanical properties, capacity for facile shaping into various configurations, and manufacturing cost-effectiveness [
77]. These polymers exhibit stability and ease of use but are inhibited by limited biocompatibility. In contrast to their naturally occurring equivalents, synthetic polymers possess the advantage of being conveniently manufacturable on an industrial level. Furthermore, their inherent adaptability enables them to be employed in various forms that promote the ideal development of tissues. The ability to precisely manipulate both the hydrophilic and hydrophobic regions of synthetic polymers additionally permits the fabrication of more homogenous frameworks and an improved capacity for the retention of water [
78]. Hybrid polymers (blended), which exhibit favorable physicochemical characteristics, can be achieved through their combination with biopolymers. The positive attributes of blended hydrogels fabricated from synthetic polymers are further improved using bioactive substances derived from naturally occurring substances. Blended hydrogels serve as a solution for future wound treatment by combining their favorable characteristics. Some synthetic polymers include polyvinyl alcohol, polyethylene glycol, and polyvinylpyrrolidone.
3.1. Polyethylene Glycol (PEG)
Polyethylene glycol (PEG) is a polymer that possesses hydrophilic properties, resulting in it being capable of interacting favorably with water. PEG is characterized by its flexibility and is composed of ether-based units.
The use of PEG-based hydrogels in constructing biological systems has been motivated by their remarkable biocompatibility and ability to thwart protein attachment. The addition of functional groups may generate PEG derivatives like PEG dimethacrylate (PEGDM) and PEG diacrylate (PEGDA), which can then be chemically cross-linked to create long-lasting matrices that permit the connecting or integrating of biomolecules to support tissue repair [
78]. Polymethacrylic acid (PMA) and polyacrylic acid (PAA) can combine with PEG to create complexes by hydrogen bonding between the carboxyl groups of PMA and the oxygen of PEG. This facilitates the absorption of liquids by the complex, causing it to expand at low pH, forming a gel. PEG may also be used as a cross-linker due to its rigidity, water solubility, and low immunogenicity [
79]. Growth factors, such as epidermal growth factor (EGF) and PEG macromers, have a favorable attraction and can form chemical bonds with each other. These can be specifically directed to the site of injury. PEG’s mechanical, thermal, and crystallinity attributes can be enhanced by including chitosan in the polymer blends [
80]. PEG-based hydrogels have been used for the treatment of lesions in individuals with diabetes. These hydrogels facilitate wound repair by stimulating the multiplication and development of skin cells. The application of such dressings has been observed to decrease scar development.
A wound closure study using PEG-based hydrogels on 1.5 cm long incisions in Sprague Dawley rats was conducted by Chen et al. (2018). Applying the PEG-based hydrogels stopped the hemorrhaging from the cuts and the incision apertures closure of the incision within minutes [
81]. Hence, the use of PEG-based hydrogels can exhibit a positive impact on the wound healing process.
3.2. Polyvinyl Alcohol (PVA)
Polyvinyl alcohol (PVA) is a hydrophilic polymer featuring properties that have garnered considerable attention from the biomedical industry. It is biocompatible, biodegradable, and semi-crystalline.
PVA can undergo physical cross-linking using several freeze–thaw cycles, called cryogelation. Additionally, PVA can be chemically cross-linked by employing glutaraldehyde or epichlorohydrin. Both methods of production produce PVA hydrogels that are remarkably hydrophilic and chemically stable [
82]. PVA can be altered with glycidyl methacrylate or acryloyl chloride to produce reactive acrylate groups via the pendant hydroxyl groups. These can then be cross-linked and polymerized to create hydrogels [
79]. PVA hydrogels serve as effective wound dressings by protecting them from external environmental stimuli and mechanical forces, reducing the risk of secondary injuries. Furthermore, PVA hydrogels exhibit favorable characteristics such as excellent water and oxygen permeability and an elevated moisture level [
83]. These attributes are particularly advantageous in wound healing, as they facilitate maintaining a moist environment, promoting the formation of new tissue, and improving the overall wound healing process. However, PVA hydrogels lack inherent antibacterial activity, necessitating the augmentation of their antibacterial efficacy when employed as a therapeutic [
84].
Through the coupling of chitosan/Fe
3+ and carboxylated polyvinyl alcohol, a double-cross-linked hydrogel was synthesized that exhibited exceptional features, including enhanced rigidity (78 kPa) and adherence traits, as well as a reduced duration for self-healing (5 min). These changes were observed to align with the dynamic nature of lesions. The hydrogel demonstrated antibacterial efficacy and enhanced hemostatic ability throughout the wound recovery phase. Furthermore, it was proposed that the hydrogel could reduce skin repair duration to 14 days [
85].
3.3. Polyvinylpyrrolidone (PVP)
Polyvinylpyrrolidone (PVP) is a crystalline polymer soluble in water and polar solutions. PVP is a highly appealing polymer for the manufacture of hydrogels due to its diversified qualities, including its non-toxic nature, ability to form films, and adequate adhesion. A promising technique for the cross-linking of PVP is the use of radiation. PVP is often mixed with PEG and agar to form a reaction mixture that undergoes cross-linking through irradiation under a linear electron accelerator. Radiation cross-linking removes the need for an initiator and cross-linking agent and allows for easy manipulation of the hydrogel properties [
86]. PVP can absorb water up to a magnitude of one hundred times its mass, which facilitates the preservation of moisture [
87]. The semi-permeable nature of PVP enables the selective permeation of oxygen while effectively impeding the ingress of bacteria and other contaminants. The utilization of PVP is beneficial in the debridement process, as it effectively absorbs exudate and necrotic tissue. PVP can potentially protect wounds from further injury or the onset of infection [
88].
Hydrogel fibre mats using PVP with ferulic and p-coumaric acid have been synthesized. The biocompatibility studies conducted on erythrocytes from humans, A549 cells, and HaCaT cells demonstrated the absence of any adverse impacts. The ex vivo experiments on human skin revealed evidence of skin regrowth and effective regulation of inflammation, as seen by the presence of minimal quantities of pro-inflammatory cytokines, specifically IL-6 and IL-8. Hence, the results obtained from the study suggest that PVP-based fibre hydrogels have the potential for application in wound treatment [
89].