Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Oncology
Orbital and ocular adnexa lymphomas are rare neoplasms confined to the orbital region. The prognosis is generally favorable, with a high proportion of localized disease, indolent clinical course, prolonged disease-free intervals, and low lymphoma-related mortality rate.
- orbital tumors
- lymphoma
- ocular oncology
- radiation oncology
1. Introduction
Orbital and ocular adnexa lymphomas (OOAL) are a rare localization of lymphomas confined to the orbital region, accounting for approximately 7–8% of all non-Hodgkin’s lymphomas (NHLs) [1,2]. These neoplasms develop from B-lymphocytes, T-lymphocytes, or NK lymphocytic cells [3,4]. It is recognizable by its morphological heterogeneous appearance with variable presence of germinal centers, plasma cells, and/or monocytic lymphocytes [4]. Within the NHLs, histological subtypes can be divided into indolent or low-grade lymphoma (i.e., extranodal marginal zone lymphoma (EMZL)) involving mucosa-associated lymphoid tissue (MALT), follicular lymphoma (FL) or lymphoplasmacytic lymphoma) and aggressive or high-grade lymphomas (e.g., diffuse large B-cell lymphoma (DLBCL) or mantle-cell lymphoma (MCL)) with different patterns of response to local and systemic treatment, local or distant recurrence [5,6]. An 80% of lymphomas involving ocular adnexa (conjunctiva, orbit, lacrimal gland, and eyelid) have mature B-cell origin [4] as a response to persistent antigenic stimulation in case of chronic inflammatory or autoimmune disorders [7]. Association with C. psittaci infection is also documented, especially in Eastern nations, even if there is no overall acceptance [8,9]. These types of lesions must be distinguished from intraocular lymphoma, a subtype of primary central nervous system lymphoma that represents a high-grade process with a distinct therapeutic strategy, but is not the subject of this review [10]. Lymphoma occurs predominantly in elder individuals [11] with an incidence peak amongst the fifth and seventh decade of life (median age ∼65 years), with a female predominance (male/female = 1:1.5/2) in the Western population. In contrast, a Korean study by Cho et al. revealed a significantly younger age at diagnosis (median age of 46 y/o), with a male predominance [11]. Ucgul et al. reported the rarity of this pathology in the pediatric population [12]. Treatment may include radiotherapy (RT), chemotherapy (CHT), immunomodulating therapy, primary antibiotic treatment, surgical excision, or combination therapy. The choice of treatment depends on a variety of factors: histopathologic type, systemic staging at the initial presentation, and patient comorbidities. When in the early stage, radiotherapy alone is the curative option in patients diagnosed with indolent lymphoma to achieve high response rates with manageable toxicity [13,14].
2. Treatment Options
Various strategies of treatment are available depending on the initial stage of the neoplasm: surgical excision, radiotherapy, chemotherapy, anti-chlamydial antibiotic (doxycycline and clarithromycin) [7,9], and immunomodulating therapy or combination therapy. Tailoring the treatment requires a multidisciplinary approach which should consider extensions, patient comorbidities, disease-related prognostic factors, short and long-term efficacy, and toxicities impact on a patient’s quality of life [7]. Radiotherapy alone is usually the treatment of choice, in early stage and indolent OOAL (stage I–IIE) [27]. Patients with stage III or IV or with aggressive OOAL’s histotypes need a systemic treatment chemotherapy/immunotherapy combined with local radiotherapy [28]. However, no prospective clinical trials have been conducted to evaluate these therapeutic options or define the optimal treatment approach for these patients. Radiotherapy and non-radiotherapy therapeutic options are summarized in detail in Figure 1.
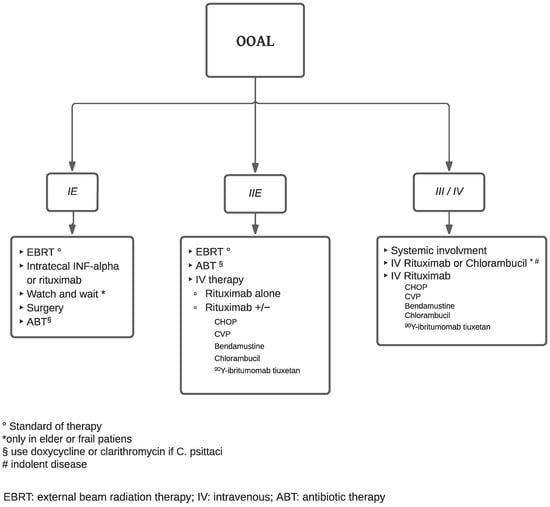
Figure 1. Flow chart of treatment.
2.1. Non-Radiotherapy Treatment Options
“Watch and wait” is not recommended due to the high incidence of local and systemic recurrence, but it can be taken under consideration in the setting of frail elderly patients with low-grade, asymptomatic, and unilateral disease with severe comorbidities that preclude other and more aggressive therapeutic approaches [29,30]. Surgical resection may be used to treat small or encapsulated tumors (e.g., conjunctival and lacrimal gland tumors). However, surgery alone showed a high risk of recurrence if not associated with adjuvant chemotherapy or radiotherapy [31]. In case of aggressive histological subtypes (i.e., MCL, DLBCL, T-cell lymphoma), bilateral disease, high-risk of local or distant relapse, chemotherapy regimen containing cyclophosphamide (CHOP (cyclophosphamide, adriamycin, vincristine, prednisone), COP/CVP (cyclophosphamide, vincristine, prednisone), C-MOPP (cyclophosphamide, vincristine, procarbazine, prednisone), and schemes containing Chlorambucil or Bendamustine can be taken under consideration with or without radiotherapy [32,33,34,35]. If infection with C. psittaci is detected, especially in Eastern countries, antibiotics, such as Doxycycline, can be used [7,8,9]. Interferon-alpha (INF-α) is an option for OOAL localized in the conjunctiva or the lacrimal glands. This glycoprotein has already been used in other neoplasm treatments, which possess antiviral, antiproliferative, and immunomodulatory functions (i.e., apoptosis, producing tumor suppressor gene p53, inhibition of tumoral neo angiogenesis). Cellini et al. and Holds et al. documented the successful use of intralesional INF-α in the treatment of conjunctival lymphoma [36,37]. Generally, 1 million IU of INF-α are administrated weekly, with optimal local control rate. INF-α showed low toxicity, and in general, no significant local side effects after injection. Rituximab is a monoclonal chimeric anti-CD20 antibody that targets the surface antigen CD20, overexpressed on CD20-positive NHL B cells. It can be administered intralesionally in case of recurrence and local relapse [38] or intravenously for bilateral or systemic involvement [39]. As previously mentioned, it can be used alone or in combination with other chemotherapy drugs. Monoclonal antibodies can be used to deliver radioisotopes to the site of OOAL [7], with the same or better outcome compared to rituximab. Esmaeli et al., in their study, promoted a protocol where Yttrium 90-ibritumomab tiuxetan (Zevalin®, IDEC Pharmaceuticals Corporation, San Diego, California), a radiolabeled anti-CD20 monoclonal antibody, is administrated after 2 weekly intravenous rituximab 250 mg/mq [40].
2.2. Radiotherapy Treatment Options
OOALs are characterized by high radiosensitivity [41,42]. External beam radiation therapy (EBRT) is the gold standard treatment in OOAL classified as Ann Arbor Stage IE-IIE thanks to high response rates and outstanding local control [16]. Radiotherapy can be administrated as a solo treatment, with adjuvant systemic therapy, or as salvage therapy after partial or incomplete response or in case of relapse [43]. Clinical exams to evaluate the extension of orbital disease is utilized for radiotherapy plans. A review of a CT scans, MRI and/or PET scans are utilized when available in order to create a deformable fusion. The gross tumor volume (GTV) includes the tumor extent, and the clinical target volume (CTV) includes the entire GTV plus an adequate margin to fully encompass the anatomical region involving the mass. The planning target volume (PTV) includes CTV with a 10 mm to 15 mm margin [42,44]. A bolus is positioned on the skin to facilitate the superficialization of the dose, especially when palpebral skin is involved. Different particles can be adapted to deliver the dose: electrons, photons, and protons. An electron beam can be used for superficial lymphomas of the eyelid and/or conjunctiva that do not infiltrate the ocular bulb. Electron energies typically cover the entire orbit. For patients with superficial disease limited to the eyelids or conjunctiva, treatment is generally delivered using electron beams (6–12 MeV) with or without bolus to provide optimal surface dose coverage. Deeper lesions are generally treated with higher energy electron beams (9–16 MeV) or photon beams (4–6 MV) [19,45]. The photon beam has been used widely for deeper lesions involving lacrimal glands, orbital soft tissue, muscles, or for bulky mass that extends beyond the globe equator. Proton beam therapy (PBT) is a valid option for the treatment of most ocular and periorbital malignancies (e.g., melanomas, lymphomas, squamous cell carcinomas, rhabdomyosarcoma hemangioma, metastases of solid tumors) with excellent control rates [45,46,47,48,49]. Compared with conventional photon radiotherapy, PBT uses heavier subatomic particles to deliver energy with higher accuracy, conformal treatment isodoses without dose fall-off and with less scattering to the healthy surrounding tissues. Proton beams are generated by a cyclotron or synchrotron and then accelerated to proper target energy [50,51]. The proton dose distribution that may be achieved is generally superior to the dose distribution of conventional photon radiotherapy. PBT may improve the survival rate of patients by improving the local tumor treatment rate, sparing adjacent tissues and lowering collateral damage. Cirrone et al. performed a study on 4 patients with orbital non-Hodgkin lymphoma ranging between 30 and 48 Gy [RBE], with 4 fractions on 4 consecutive days [47]. Nonetheless, due to the high treatment costs for facility building and maintenance, PBT is not very diffuse. Despite the consensus on the primary role of radiotherapy, there is no universally accepted optimal radiation dose and fractionation for patients with OOAL [27]. Historically, patients have received treatment with conventional doses of 24–36 Gy with local control rates >95% and a minimum dose required of 25 Gy [6,28,52,53] Le et al. found no differences in terms of distant progression-free survival (dPFS) or local recurrence (LR) after EBRT in pts with ≤34 Gy compared with higher doses; the only difference was the increase in local toxicities observed [53]. Bhatia et al. [54] and Letschert et al. [55] treated low-grade with a median dose of 30 Gy and intermediate to high-grade tumors with a median dose of 40 Gy.
3. Treatment Toxicity
Treatment-independent factors, especially in elderly patients, must be considered (i.e., diabetes, glaucoma, sicca syndrome, Sjögren syndrome) because they may influence cataract development. Most patients experienced mild acute toxicities, such as skin erythema in the periorbital area, conjunctival hyperemia, chemosis, swelling, and excessive tearing, during or immediately after the radiotherapy course, which were mainly self-limited or responded to a short course of lubricant gels or skin moisturizers. These symptoms generally resolve in a few months after completion of radiotherapy [19,43]. Long-term toxicities include: radiation-induced cataracts, persistent dry eyes, and iris neovascularization [56,57]. Serious toxicities such as corneal or skin ulceration, telangiectasia, neovascular glaucoma, and radiation retinopathy are extremely rare [58,59]. Radiation-related severe late side-effects incidence increases when patients are treated with RT doses ≥35 Gy, resulting in considerable late toxic effects, including keratitis, severe dry eye syndrome, glaucoma, retinopathy, and cataract formation [28,60,61]. Stafford et al. reported a 52% rate of acute complications with doses ranging from 19 to 48 Gy [60]. Retinal toxicity may result in visual impairment, which can significantly impact quality of life [62,63]. During treatment, shielding, such as a contact lens under the eyelid, can lower the dose for healthy and sensible organs [53,64].
This entry is adapted from the peer-reviewed paper 10.3390/cancers15245782
This entry is offline, you can click here to edit this entry!
