Axillary lymph node dissection (ALND) has traditionally been performed to assess nodal status, prevent axillary recurrence, and possibly improve survival. However, the procedure has been associated with postoperative morbidities, including arm lymphedema, shoulder dysfunction, and paresthesia. Sentinel lymph node (SLN) biopsy was introduced as an alternative approach to assess axillary nodal status and potentially eliminate the need for ALND in patients with clinically node-negative (cN0) breast cancer. Despite this progress, eliminating ALND for all breast cancer patients still seems premature at this time. Various forms of conservative axillary surgery have been developed to replace or supplement conventional ALND. Conservative axillary surgery may be promising in reducing the incidence of arm lymphedema without increasing the risk of axillary recurrence.
1. Conservative Axillary Surgery
In the era of effective multimodality therapy, various forms of conservative axillary surgery have been developed to decrease the incidence of arm lymphedema without increasing axillary recurrence [
29]. Conservative axillary surgery includes partial lower ALND, conservative axillary regional excision (CARE), conservative ALND with axillary reverse mapping (ARM), and tailored axillary surgery (TAS).
2. Partial Lower ALND for cN0 Patients
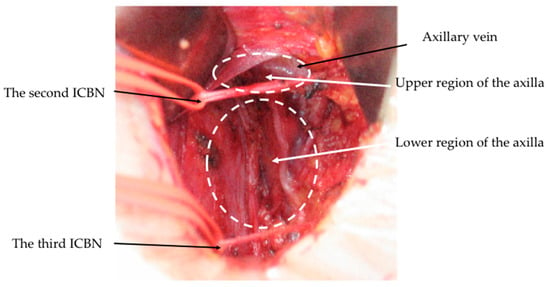
The axilla is anatomically divided into upper and lower parts, as separated by the second intercostobrachial nerve (ICBN) (
Figure 1) [
30,
31]. ALNs and lymphatics draining from the upper extremity are generally located in the upper area situated between the axillary vein and the second ICBN [
32], although lymph nodes lateral to the lateral thoracic vein are more specific to the lymphatic drainage of the upper extremity than to the drainage of the breast [
33]. In a preliminary study of Kodama et al. [
34], ALNs were excised separately from the upper and lower regions of the axilla in 100 cN0 breast cancer patients. On histological examination, nodal metastases were identified in the upper region in only 8% of patients. As a result, Kodama et al. subsequently developed a procedure known as partial lower ALND to preserve the ALNs and lymphatics located between the second ICBN and axillary vein. In this procedure, the level I axillary nodes caudal to the nerve were excised while retracting the second ICBN using tape. This is different from four-node sampling, where hard or enlarged axillary nodes were selectively removed from the axillary tissue. Such an approach was used in 1043 cN0 patients, with 248 (23.8%) patients undergoing total mastectomy and 795 (76.2%) patients undergoing BCS with breast radiation. A median of seven ALNs were removed per patient, and ALNs were involved in 21.3% of cases. Within a median follow-up period of 72 months, only six patients (0.6%) experienced axillary recurrence and no cases of lymphedema occurred. In their retrospective comparative study, the incidence of arm lymphedema was significantly lower in patients who underwent partial lower ALND compared with those who received conventional ALND (0% vs.11.8%:
p < 0.0001) (
Table 4).
Figure 1. Axillary anatomy after conventional ALND. Lateral thoracic artery and vein were removed; intercostobrachial nerves (ICBNs) were preserved.
Table 4. Partial lower ALND and CARE procedure.
| Patients/Methods |
No. of
Patients |
Systemic
Chemotherapy |
Radiotherapy |
Follow-Up
Period |
Axillary
Recurrence |
Arm
Lymphedema |
| (a) cN0 patients [34] |
|
|
|
|
|
|
| Partial lower ALND |
1043 |
100% |
Not reported |
72 months |
0.6% |
0.0% |
| Conventional ALND |
1084 |
100% |
Not reported |
120 months |
0.1% * |
11.8% # |
| (b) cN0 and cN+ patients [35] |
|
|
|
|
|
|
| CARE procedure |
587 |
49.3% |
25.9% |
5.1 years |
0.5% |
3.4% |
3. Conservative Axillary Regional Excision (CARE)
Another form of conservative axillary surgery that has emerged is conservative axillary regional excision (CARE). The procedure involves removing SLNs and other palpable suspicious nodes [
35]. Total mastectomy with CARE was performed in 587 patients, including not only 379 cN0 patients but also 208 cN+ patients. A median of eight ALNs were removed per patient. Of the patients, 289 (49.2%) patients received NAC or adjuvant systemic therapy and 152 (25.9%) received postoperative radiotherapy. Within a median follow-up period of 5.1 years, axillary recurrence only developed in three (0.5%) patients, while arm lymphedema occurred in twenty (3.4%) patients (
Table 4). These findings support the use of the CARE procedure in selected cN+ patients. However, it is worth noting that the CARE procedure is largely identical to SLN biopsy. The American Society of Clinical Oncology (ASCO) recommends that suspicious palpable nodes, irrespective of their dye or radioisotope uptake, be removed as a part of SLN biopsy [
36]. Nevertheless, the CARE procedure was performed not only in the cN0 patients but also in the cN+ patients. Previously, the researchers have found that SLN biopsy can be used to assess the axillary nodal status of both cN+ and cN0 breast cancer patients [
37].
4. Conservative ALND with Axillary Reverse Mapping (ARM)
ARM was developed as a surgical procedure to minimize the risk of arm lymphedema by delineating and preserving arm-draining nodes and lymphatics during ALND [
38,
39]. Since the procedure first emerged, multiple randomized trials have confirmed that ARM is effective in reducing arm lymphedema [
40,
41,
42,
43,
44,
45]. However, there have also been concerns about the oncological safety of ARM due to the not-infrequent involvement of ARM nodes. There are lymphatic interconnections between nodes draining from the upper extremity and nodes draining from the breast [
46]. Using the blue dye technique, a study of Boneti et al. [
47] observed that lymphatic drainage from the arm and breast rarely converged in SLN and that none of the receiving nodes contained metastases. As a result, it is concluded that preserving the ARM nodes may decrease the incidence of postoperative lymphedema (
Table 5).
Table 5. The surgical procedures with ARM and the outcome in cN0 patients.
Authors/
Surgical Procedures with ARM |
Identification
Rate of SLNs |
Identification Rate
of ARM Nodes
or Lymphatics |
Crossover Rate
between
SLN and ARM Nodes |
Involved Rate
of ARM Node |
Axillary
Recurrence |
Objective
Lymphedema |
| (a) Boneti et al. [47] |
|
|
|
|
|
|
| SLN biopsy (n = 220) |
97.2% (214/220) |
40.6% (87/214) |
2.8% (6/214) |
0% (0/15) |
/ |
|
| and/or ALND (n = 47) |
|
|
|
|
/ |
5.4% (2/51) |
| (b) Noguchi M, et al. [48] |
|
|
|
|
|
|
| SLN biopsy alone (n = 437) |
98% (499/507) |
63% (321/507) |
28% (140/499) |
|
0.9% (4/429) |
0.7% (3/429) |
| ALND after SLN biopsy (n = 70) |
|
93% (65/70) |
34% (24/70) |
5.7% (4/70) # |
2.9% (2/70) |
21% (15/70) * |
Although the ARM procedure is generally performed using blue dye, the fluorescent method, which uses indocyanine green (ICG), was developed as an alternative [
49]. The fluorescent imaging technique is highly sensitive in identifying ARM nodes. In a study by Noguchi et al. [
48], 507 patients with cN0 breast cancer underwent SLN biopsy with the ARM procedure using fluorescence dye. Although ARM nodes were involved in 18 of the 65 patients in which ARM nodes were identified, in 14 (78%) of these patients, the involved ARM nodes were identical to the SLNs identified. Since SLN–ARM nodes should be removed, ARM nodes were ultimately involved in only four (5.7%) patients after SLN biopsy. The authors concluded that, with the exception of positive SLN–ARM nodes, the involvement of ARM nodes in SLN-positive patients is infrequent (
Table 5). Nevertheless, indications for ARM in cN0 patients might be limited in light of results from the Z0011 and AMAROS trials [
44]. As mentioned above, ALND can be avoided in patients with one to two positive SLN(s) undergoing either BCS with whole breast irradiation [
6] or mastectomy with axillary radiation [
7]. On the other hand, ARM nodes are involved in a significant proportion of cN+ patients [
50]. Therefore, identified ARM nodes with suspected malignancy must be removed even in the ARM procedure. However, it is important to note that ARM lymphatics draining from the upper extremity should be spared as much as possible in order to minimize the risk of arm lymphedema.
A randomized clinical trial was conducted to compare conventional ALND and ARM-guided ALND [
45]. To identify the ARM nodes and lymphatics, methylene blue and radioisotope were injected into the upper extremity. A total of 265 patients including pN1-3 patients were randomized into two groups: 127 patients underwent conventional ALND and 138 patients underwent ARM-guided ALND with the aim of preserving ARM nodes and lymphatics. Nevertheless, in the ARM-guided ALND group, after examining identified ARM nodes using fine needle aspiration cytology, ARM nodes were determined to be involved and were subsequently removed in 11 patients (8.5%). In the median follow-up period of 20 months, arm lymphedema had developed in forty-two (33.1%) of the patients who underwent conventional ALND and in seven (5.9%) of the patients who underwent ARM-guided ALND (
p < 0.001). No patients in either group developed axillary recurrence. It is concluded that while ARM-guided ALND can reduce the incidence of lymphedema, this approach may not be suitable for advanced breast cancer (pN2-3) patients (
Table 6).
Table 6. ARM-guided ALND versus conventional ALND.
| Authors/Methods |
No. of
Patients |
Adjuvant
Chemotherapy |
Radiotherapy |
Follow-Up
Periods |
Axillary
Recurrence |
Arm
Swelling |
| (a) Yue et al. [45] |
|
|
|
|
|
|
| ARM-guided ALND |
138 |
None |
Not reported |
20 months |
0% |
5.9% |
| Conventional ALND |
127 |
None |
Not reported |
20 months |
0% * |
33.1% # |
| (b) Yuan et al. [40] |
|
|
|
|
|
|
| ARM-guided ALND |
543 & |
None |
56.5% |
37 months |
1.4% |
3.3% |
| Conventional ALND |
648 & |
None |
60.6% |
37 months |
1.2% * |
15.3% # |
The iDEntification and Preservation of ARm lymphaTic system (DEPART) is another form of conservative axillary surgery that has been developed [
40]. In the study that introduced this procedure, fluorescent dye (ICG) and methylene blue were injected into the upper extremity to identify ARM nodes and the subsequent-echelon nodes. All identified ARM nodes and lymphatics were preserved except SLNs and palpable suspicious nodes. Palpable suspicious ARM nodes (fluorescent or blue nodes) were histologically examined by partial frozen sections and removed if determined to be positive. In the randomized clinical trial, 874 cN+ patients and 480 SLN-positive patients were randomized to either undergo conventional ALND or the DEPART procedure. Postoperatively, both groups of patients received adjuvant chemotherapy, and high-risk patients underwent axillary radiotherapy. Within a median follow-up period of 37 months, arm lymphedema had developed in 18 (3.3%) patients who underwent the DEPART procedure and in 99 (15.3%) of patients who underwent conventional ALND (
p < 0.001); however, the incidence of axillary recurrence did not differ significantly between the two groups (1.4% vs. 1.2%) [
40] (
Table 6). Thus, palpable nodes with suspected malignancy should be removed even in ARM-guided ALND.
5. Tailored Axillary Surgery (TAS) for cN+ Patients
Another surgery that has been developed to decrease the incidence of arm lymphedema is TAS. This approach consists in removing all palpable suspicious lymph nodes together with the blue and radioactive SLNs, ideally performed with image-guided localization of the clipped node to achieve optimal results [
51,
52,
53]. This procedure is performed on cN+ patients, either after NAC or in the upfront surgical setting. Ultimately, TAS aims to turn cN+ patients into cN0 patients primarily through the selective removal of palpable suspicious nodes. Following TAS, axillary radiation is administered to treat any remaining nodal disease. Nodal radiotherapy is effective in achieving local control in patients with low-volume remaining nodal disease.
A randomized clinical trial known as the TAXIS trial is currently underway to investigate the oncological safety and improvement to quality-of-life associated with TAS and axillary radiotherapy in comparison with the use of conventional ALND in patients with cN+ breast cancer. The primary endpoint of this non-inferiority trial is disease-free survival, and secondary endpoints include morbidity and quality of life. Accrual completion is projected for 2025 and the primary endpoint analysis is expected to finish in 2029 [
53]. To date, the feasibility of TAS has been confirmed in a pre-planned sub-study involving 296 patients [
52]. Of these patients, 125 (42%) received NAC, and 71 (56.8%) of this cohort achieved nodal pCR. In this trial, TAS selectively removed positive lymph nodes and remained much less radical than ALND. In fact, for ALND performed after TAS, additional positive nodes were removed in 70% of patients [
52]. Although all of these patients received axillary radiation, the rate of incidence for additional positive nodes was significantly higher compared with corresponding rates from the Z0011 and AMAROS trials [
6,
7].
This entry is adapted from the peer-reviewed paper 10.3390/cancers15225353