infection might be involved one of the many factors in the complex pathogenesis of MAFLD.
infection can impact the composition and function of the gut microbiota, insulin resistance, and systemic inflammation. [
infection can affect its composition and diversity, potentially influencing the development of MAFLD. However, the precise mechanisms underlying this relationship are not yet fully understood. Moreover, the systemic inflammatory state that contributes to the pathogenesis of MAFLD is associated with an
infection, during which the concentration of pro-inflammatory markers increases, potentially influencing the development of MAFLD in a yet-unclear manner [
].
Antibiotics can eliminate unfavorable microbiota, and their efficacy has been confirmed in several liver diseases [
165]. For treating cirrhosis and encephalopathy, as well as spontaneous bacterial peritonitis, fluoroquinolones (norfloxacin and ciprofloxacin), third-generation cephalosporins (ceftriaxone and cefotaxime), and trimethoprim–sulfamethoxazole are recommended; and neomycin, metronidazole, polymyxin B, and rifaximin have been used. β-Lactam/β-lactamase inhibitor combinations (BLBLIs) and carbapenems are recommended as the first choice in empirical treatments. Rifaximin, as a eubiotic, has a potential effect on the liver by modulating the bowels’ microbiota. Gangarapu et al. [
166] found that the short-term administration of antibiotics improved clinical symptoms in NAFLD/MASH patients by lowering circulating endotoxin and IL-10 levels (0.9 ± 0.34 vs. 0.8 ± 0.13 EU/mL,
p = 0.03 and 4.08 ± 0.9 vs. 3.73 ± 0.7 pg/mL,
p = 0.006, respectively) as well as LFTs (AST: 50.4 ± 39 vs. 33 ± 14 IU/L,
p = 0.01; ALT: 72 ± 48 vs. 45.2 ± 26.3 IU/L,
p = 0.0001, GGT: 52 ± 33 vs. 41.2 ± 21.1 IU/L,
p = 0.02). Similarly, a study by Abdal-Razik et al. [
167] demonstrated a significant decrease in transaminases and transferase activity [ALT: 64.6 ± 34.2 vs. 38.2 ± 29.2 IU/L,
p = 0.017; AST: 66.5 ± 42.5 vs. 40.1 ± 20.1 IU/L,
p = 0.042; GGT: 56.7 ± 31.6 vs. 34.8 ± 28.6 IU/L,
p = 0.046]; endotoxins; and IL-10, TNF-alpha, and IL-6 levels [0.82 ± 0.22 vs. 0.7 ± 0.09 EU/mL,
p = 0.001; 40.6 ± 18.78 vs. 58 ± 23.16 pg/mL,
p = 0.009; 19.18 ± 9.29 vs. 13.34 ± 8.31 pg/mL,
p = 0.045; 8.34 ± 1.8 vs. 6.67 ± 1.1 pg/mL,
p = 0.004, respectively]; and the NAFLD Liver Fat Score [from (−0.6) to (−0.2) vs. from (−0.7) to (−0.4) (
p = 0.034)], following the administration of rifaximin for 6 months but not after 1 month of therapy.
7. Antioxidants
Vitamin E (Alpha-Tocopherol)
Current international guidelines for the management of liver diseases (e.g., AASLD, AACE, the European Association for the Study of Diabetes (EASD), and the European Association for the Study of Obesity (EASO)) indicate the use of vitamin E (alpha-tocopherol) in the therapy of MASH in patients without diabetes [
7]. Lipid accumulation in hepatocytes leads to lipotoxicity and increases the level of oxidative stress, which results in liver injury and inflammation [
170]. As a redox scavenger, vitamin E may prevent the damage caused by excessive oxidative stress [
171]. The off-label use of vitamin E is connected with improvements in LFTs [
172]. The current recommendations on the use of vitamin E in NAFLD treatment are based on the results presented in RCTs concerning patients suffering from MASH with or without type 2 diabetes mellitus (DMT2). In the PIVENS trial, the antioxidative properties of vitamin E appeared to have a positive effect on the liver histology both in reducing the NAFLD activity score (NAS) and resolving MASH [
72,
173].
8. Interactions between the Endocrine System and NAFLD
8.1. Thyroid Hormones
As mentioned earlier, hypothyroidism is an important risk factor for MAFLD [
179]. The use of thyroid hormones to induce fat loss in the liver might be a promising therapeutic option, but the burden of side effects precludes their use in native form. However, it might be feasible to use specific agonists of thyroid receptor beta (TRb), which selectively affect liver metabolism while omitting most cardiac effects (e.g., tachycardia) resulting from TRa activation. Currently, there are several compounds under evaluation in the treatment of NAFLD. Resmetirom halved liver fat content, as assessed using MRI-PDFF, in patients with MASH during 36 weeks of treatment with an 80 mg daily dose of the drug [
180]. This was accompanied by a significant reduction in ALT [11.0 ± 6.8 vs. (−15.4) ± 4.7 IU/L;
p = 0.0019] and AST [3.6 ± 2.8 vs. (−7.4) ± 1.9 IU/L;
p = 0.0016] activities at week 36. The 72-week open-label extension trial also showed resmetirom’s efficacy and sufficient tolerability.
8.2. Testosterone
Low testosterone levels (<346 ng/dL) in males have been linked with noninvasive markers of liver steatosis [
183]. Long-term observations strongly suggest improvements in liver steatosis in hypogonadal men during testosterone replacement therapy. A 12-year follow-up showed that maintaining the optimal testosterone level with testosterone undecanoate resulted in a significant improvement in the Fatty Liver Index (from 83.6 ± 12.08 to 66.91 ± 19.38;
p < 0.0001) and GGT (from 39.31 ± 11.62 to 28.95 ± 7.57 IU/L;
p < 0.0005) but without a significant change in the ALT or AST activity [
184]. Therefore, testosterone-replacement therapy is improving the metabolic status of males with hypogonadism. Conversely, testosterone or anabolic androgenic steroids may lead to liver damage in men with normal testosterone levels [
185].
8.3. Estradiol
Estrogens play an important role in the metabolism of lipids [
186]. Estradiol deficiency, which occurs after menopause, coincides with an increased propensity to develop NAFLD [
187]. The loss of the protective effects of estrogens is also reflected by a reduction in the sex-hormone binding protein (SHBG), which leads to a relative “excess” in androgen levels [
188]. Estradiol therapy might be beneficial for the course of MAFLD after menopause, but it is generally used with progestins, which may alleviate the benefits [
189].
8.4. Growth Hormone
Growth hormone (GH) has a multidimensional influence on the human metabolism, including that of the liver. Both deficiency and excess may lead to several pathologies [
192]. GH deficiency is commonly associated with liver steatosis, and the risk of NAFLD development in such patients is nearly two-fold OR = 1.85; 95% CI: [(1.05–3.28);
p = 0.03] [
193]. Patients with NAFLD tend to have a reduced peak GH secretory response (9.2 ± 6.4 vs. 15.4 ± 11.2 ng/mL;
p = 0.001), and higher IGF-1 (Insulin-like Growth Factor-1) levels are associated with less-advanced FIB-4 scores [
194].
9. Other Therapies
9.1. Xanthine Oxidase Inhibitors
A positive correlation between hyperuricemia and the incidence of MAFLD underlies the research concerning the probably beneficial effects of therapy with xanthine oxidase inhibitors (allopurinol and febuxostat) on liver functions [
196].
In the mouse model of MASH, both xanthine oxidase inhibitors appeared to alleviate hepatic steatosis and fibrosis [
197,
198]. In a pilot interventional study with febuxostat in patients with MAFLD, serum levels of ALT [before: 73.0 (69.8–117.8); after: 70.5 (57.5–94.5) IU/L,
p = 0.040] and AST [before: 50.5 (40.8–69.8); after: 44.5 (34.8–60.8) IU/L,
p = 0.018] were significantly decreased, and hepatic steatosis, as confirmed by conducting a histopathological examination, was improved [
197]. The results of an ongoing interventional randomized clinical trial comparing the influences of allopurinol and febuxostat on MAFLD (NCT05474560) may clarify the potential use of xanthine oxidase inhibitors for the therapy of liver diseases in the future [
199].
9.2. Lubiprostone
A gut–liver axis dysfunction turned out to be one of the pathological mechanisms responsible for the progression of MAFLD. Thus, disturbances in the intestinal permeability and dysbiosis have become potential targets in the management of MAFLD [
200].
Lubiprostone, an oral metabolite of prostaglandin E
1, which increases intestinal fluid secretions by promoting the intraluminal chloride-anion efflux, was originally implemented for the therapy of idiopathic constipation and irritable bowel syndrome with constipation [
201].
9.3. Pentoxifylline
Considering the multifactorial pathogenesis of MAFLD, which includes inflammation, drugs with potential anti-inflammatory effects, such as pentoxifylline, were evaluated for use in the aforementioned liver dysfunction. As a nonspecific phosphodiesterase 4 (PDE-4) inhibitor with the ability to decrease the transcription of TNFa, which is considered as one of the main proinflammatory agents responsible for the degradation of hepatocytes, the effects of therapy with pentoxifylline were examined both in rodents and humans [
205,
206].
9.4. Other Drugs
The data from selected meta-analyses might suggest that several drugs commonly used in patients with cardiovascular diseases with concomitant MAFLD (e.g., losartan and acetylsalicylic acid) have positive impacts on hepatic enzyme levels or protect against progression to advanced fibrosis [
210,
211]. Nevertheless, currently, the level of evidence is underwhelming.
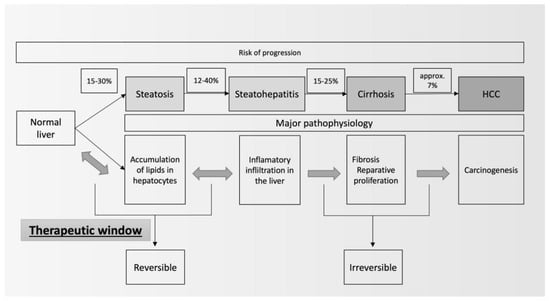
10. Summary
The pathogenesis of MAFLD is multifactorial, and the pathogenic drivers of MAFLD can serve as therapeutic targets. Those can include: the modulation of food intake, increase in energy expenditure, improvement in adipocyte insulin sensitivity, inhibition of de novo lipogenesis, tapering of oxidative stress, and reduction in inflammation. MAFLD might be considered as a part of the clinical presentation of the metabolic syndrome. For several decades, there have been major improvements in the therapies of diabetes, hyperlipidemia, and hypertension. It seems that drugs affecting incretin receptors, PPAR, and TRb have significant impacts on the surrogate markers of liver steatosis. Based on the available research findings and recommendations from liver disease societies, it appears that some of the most significant factors are the achievement of a normal body weight and the effective treatment of metabolic disorders. Still, there is a lack of a sufficient number of studies indicating which of the cardiometabolic risk factors, included in the definition of MAFLD, most significantly lead(s) to disease progression. Thus, the need for further studies on therapies that will significantly and independently mitigate both the consequences and severity of liver steatosis seems essential. Therefore, alongside the established roles of pioglitazone and vitamin E in MASH treatment, it seems that drugs for weight reduction (including incretin-based medications that also have a glycemic-normalizing effect) and other drugs that affect the cardiometabolic risk will gradually gain importance; hence, the incessant necessity for exploring pathophysiological pathways that would allow a common mechanism of action to be found for steatosis resolution regardless of the type of factor that led to it.