Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Neurosciences
ADHD is strongly associated with psychiatric comorbidities; it is reported that roughly 80% of adults with ADHD have at least one coexisting psychiatric disorder, with rates of comorbid bipolar disorder (BD) between 5 and 47%, rates of depression between 9 and 16%, and anxiety rates approaching 50% in the adult ADHD population. There is also a notable increased risk of developing psychiatric comorbidities in individuals who have ADHD, including anxiety disorders, substance use disorders, depression, and bipolar disorder.
- ADHD
- borderline personality disorder
- bipolar disorder
- management
1. Introduction
Throughout history and now into modern practice, ADHD has been regarded as a neurodevelopmental disorder in children—often slated to self-resolve during adolescence and young adulthood [1]. In recent years, however, ADHD has evolved to become more intricately understood, and it has been determined that roughly 65% of cases involve the persistence of symptoms into adulthood [2]. While there have been changes in the DSM-IV and DSM-V to reflect the persistence and presentations of ADHD in adulthood, adult patients with this disorder continue to face barriers to getting sufficient support [3]. ADHD is strongly associated with psychiatric comorbidities; it is reported that roughly 80% of adults with ADHD have at least one coexisting psychiatric disorder, with rates of comorbid bipolar disorder (BD) between 5 and 47%, rates of depression between 9 and 16%, and anxiety rates approaching 50% in the adult ADHD population [4]. There is also a notable increased risk of developing psychiatric comorbidities in individuals who have ADHD, including anxiety disorders, substance use disorders, depression, and bipolar disorder [5]. The most common comorbidities in ADHD include anxiety disorders, substance use disorder (SUD), and personality disorders, with SUD being twice as common in the ADHD population than the general population—with a predilection towards nicotine, cannabis, and cocaine [4]. Personality disorders are also found in roughly half of the adult ADHD population, and researchers identified cluster B and C disorders to be among the most common [4]. This same pattern is also observed in patients with bipolar disorder [6]. The presence of comorbidities may result in delayed recognition and treatment of ADHD.
While comorbidities vary across the psychodiagnostic spectrum, literature gaps present themselves when identifying the relationship of ADHD to personality disorders and bipolar disorder in particular—two very different but burdensome disorders that are often observed in patients with ADHD. Reports suggest that personality disorders are present in more than 50% of adults with ADHD—with particular attention focused on cluster B disorders like borderline personality disorder (BPD) [7]. This is an important concept for the management of both issues because their concurrence with one another is linked to more severe impairment and poorer response to ADHD pharmacotherapy [4].
Both bipolar I disorder and bipolar II disorder are found at higher rates among adult patients with ADHD [8]. A recent meta-analysis demonstrated that roughly 1 in 13 adults with ADHD has an additional diagnosis of bipolar disorder, while 1 in 6 bipolar patients are also living with ADHD; interestingly, it appears that there is no disparity between the rates of bipolar I disorder vs. bipolar II disorder in the adult ADHD population [9]. There are clinical characteristics that overlap in patients presenting with either bipolar disorder or ADHD, so it can pose a unique challenge to clinicians who may struggle with the identification of certain psychopathologies. Studies suggest that comorbid ADHD and bipolar disorder are linked to worsened course of illness and more frequent episodes of mania and depression [4].
2. Management Implications
2.1. Bipolar Disorder
The management of patients with comorbid ADHD and bipolar disorder is an under-researched topic; however, there have been some findings established as effective and worthy of consideration. The clinical impact in patients with ADHD and bipolar disorder is arguably increased because of the impairment in functioning that they experience because of their ADHD, in between the cycling episodes of depression and mania that are characteristic of bipolar disorder. Many studies have identified additional risks that patients with BD are subject to in the presence of a comorbid ADHD diagnosis, including:
-
earlier age of onset of BD
-
increased frequency of mood episodes (especially depressive episodes)
-
increased risk and number of suicide attempts
-
increased likelihood of substance use disorder
-
poor response to mood-stabilizing medications [16].
The treatment goals in bipolar disorder typically revolve around achieving and maintaining mood stability, as well as preventing recurrent episodes of mania, hypomania, and depression [41]. This will often entail the short-term management of mood episodes when they occur and long-term maintenance of treatment plans to minimize recurrence. Medications remain the cornerstone of BD treatment, with the most commonly used medications being mood stabilizers and antipsychotics, used in conjunction with psychotherapy and lifestyle modifications when available [42]. Treatment for bipolar disorder, however, can be an arduous process as clinicians grapple with optimizing mood stabilization and minimizing adverse effects. Additional complicating factors include treatment non-adherence, challenging social circumstances, and unavoidable triggers for mood episodes [41]. It is crucial that physicians and other care providers who treat patients with BD use a patient- and family-centered approach and that they enlist multidisciplinary professionals when appropriate.
When BD and ADHD co-occur, among the first steps in developing a treatment plan is determining which condition and which symptoms are most severe and disabling. Typically, mood stabilization is a priority because untreated mood episodes in BD can have more devastating consequences, including hospitalization [12]. Once mood stabilization is achieved, the ADHD symptoms can begin to be addressed; another challenge arises here because it is known that some medications used to treat ADHD, particularly stimulants, can pose a risk for mood destabilization in individuals with BD [43]. A great deal of caution must be exercised when trying to treat BD and ADHD using monotherapy, and there is little data to support comprehensive treatment for both conditions using one drug. While some approaches will be discussed, it is important to be vigilant about the risk of manic and hypomanic induction when using stimulants and other medications in this patient population [44].
One 6-week prospective trial in 36 patients with diagnoses of ADHD and bipolar disorder showed that sustained-release bupropion was linked to a 55% reduction in ADHD symptoms and a 58% reduction in mood episodes associated with depressed mood in bipolar disorder patients, with little evidence of hypomania induction [45]. In this study, the patients were experiencing mild symptoms only on the Young Mania Rating Scale (YMRS) and Clinical Global Impression (CGI) scales, and there was a clinically significant reduction in mood symptoms at the end of the trial [45]. The positive response observed with bupropion helped to establish this medication as an effective treatment for ADHD-BD in the Canadian Network for Mood and Anxiety Treatments (CANMAT), with level 4 evidence [16]. The rate of medication-induced hypomania was low in this sample size [45].
Bipolar disorder, when not appropriately treated, may manifest itself in ways that may make it challenging for clinicians to discern between its symptoms and those of ADHD—thus, the first goal of treatment when approaching the management of these patients is to ensure that BD symptoms are adequately controlled, typically using mood-stabilizing treatments like lithium, lamotrigine, or divalproex sodium [12]. Methylphenidate (MPH) is a central nervous system (CNS) stimulant that has proven to be effective and tolerable for the treatment of ADHD in both children and adults [46]. While previous concerns surrounding treatment-emergent mania have been brought forward, a registry of over 2000 patients in Sweden demonstrated that this medication is a safer and more effective option in the treatment of ADHD in patients with BD who were receiving concomitant mood stabilizing therapy [44]. It is important to note that stimulants should not be used in patients who are experiencing active mania or psychosis and that those who are well-controlled should receive frequent monitoring [47]. This helps to further emphasize the importance of achieving euthymia before initiating stimulant therapy for comorbid ADHD in patients with bipolar disorder.
Other medications, such as modafinil and armodafinil, were significantly superior to placebo in some studies. One small study of 85 patients with BD demonstrated that modafinil use was associated with improved depressive symptoms in the study population [48]. Similarly, another trial using armodafinil demonstrated improved depressive symptoms in patients with type I bipolar disorder, and that it appears to be safer in terms of not increasing suicidality or manic symptoms; however, the rates of clinical response using armodafinil did not differ from placebo [48].
Atomoxetine is another commonly prescribed medication for the treatment of ADHD, which is a selective norepinephrine reuptake inhibitor—the first of the non-stimulant pharmacotherapy options [49]. While it has been investigated somewhat extensively as an option for pediatric and adolescent patients with ADHD-BD, the data are limited for the adult population. It is well-established that atomoxetine is associated with a statistically significant reduction in ADHD symptoms compared to placebo, but there have also been case reports of treatment-induced hypomania with this medication [43]. Atomoxetine can be considered as a potential option for patients whose bipolar symptoms are effectively managed, with close monitoring for the risk of hypomanic induction. The other ADHD pharmacotherapy to be considered for co-management is amphetamine salts, which are categorized as CNS stimulants. Recent research suggested that amphetamine-based products may carry double the risk than methylphenidate-based stimulants in inducing mania and psychosis [50].
Evidence has shown that there are noted interactions specifically between methylphenidate and anti-seizure medications, some of which may be used as mood stabilizers in the treatment of bipolar disorder [47]. The anti-seizure medications that are of special concern when used adjunctively with methylphenidate are phenytoin and carbamazepine; there are also a small number of case reports that describe a dyskinetic reaction when MPH is used alongside valproic acid [51]. The literature that is available for the treatment of comorbid ADHD and BD is limited; however, there are evidently various options in the realm of ADHD pharmacotherapy that have been associated with potential improvement in bipolar disorder symptomatology.
It is best to think of the management of ADHD-BD using a hierarchical approach, with frequent assessment of treatment response, as seen in Figure 1.
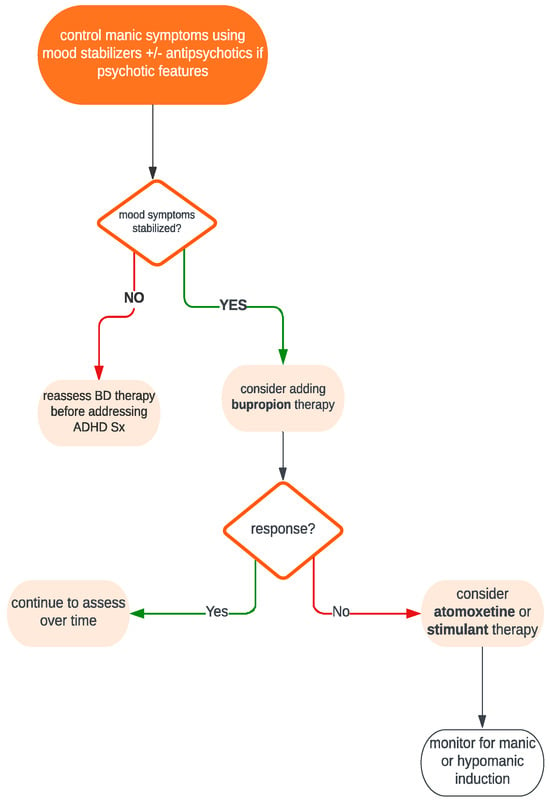
Figure 1. Simplified treatment algorithm for the pharmacological management of patients with comorbid ADHD and bipolar disorder.
While bupropion has shown some benefit in this population, it is important to consider the therapeutic advantages of using various mood stabilizers as well. Lithium, for example, which is well-established as effective BD pharmacotherapy, has demonstrated efficacy in reducing addictive and impulsive behaviors associated with ADHD and, therefore, may help to reduce complications [52]. One double-blind study found lithium to be comparable in effectiveness to methylphenidate in a predominantly male sample of ADHD patients [52].
There is limited data for using other mood stabilizers such as valproate and lamotrigine in the ADHD population; however, valproate is known to help alleviate symptoms such as emotional dysregulation and impulsivity, thereby warranting consideration for ADHD + BD co-occurrence [53]. Similarly, lamotrigine may have a positive impact on ADHD symptoms, especially when there is a depressive component to the clinical picture—this medication may be considered to help alleviate mood symptoms that contribute to impaired attention and concentration difficulties [54] (Hashimoto et al., 2021). The data for other mood stabilizers, including carbamazepine, are scant; studies of its use in BD have demonstrated a positive effect on the prevention of impulsivity, so it can be considered while further research is awaited [55].
The Canadian Network for Mood and Anxiety Treatments (CANMAT) has guidelines specifically for the treatment of bipolar disorder when it co-occurs with ADHD. Again, the stabilization of mood symptoms in BD using pharmacotherapy is identified as the priority before addressing ADHD symptoms [41]. ADHD pharmacotherapies were all tested for the management of ADHD symptoms in the adult BD population, and the evidence was varied. The medications atomoxetine, bupropion, and lisdexamfetamine are supported by level 4 evidence, while methylphenidate and mixed amphetamine salts are supported by level 3 evidence [41].
While atomoxetine, bupropion, and lisdexamfetamine are all supported by evidence of similar quality, because of limited data to support atomoxetine in the adult population as well as the risk of hypomanic induction, bupropion remains the preferred first-line agent for managing ADHD symptoms in the BD population. This is supported by recent literature that has demonstrated the clinically significant improvement in disease severity that bupropion has in patients with bipolar disorder, in addition to its dopaminergic properties that render it an effective choice for ADHD treatment [56]. There was a 2017 Cochrane review of a small number of studies that generally concluded that bupropion may lead to a small improvement in ADHD and may decrease ADHD symptoms [57]. Of importance, it is also considered not to pose a greater risk for phase switching (induction of hypomania or mania) when compared to any of the other antidepressants studied, including other SNRIs and SSRIs [56].
Key Points:
-
Adequate mood stabilization in patients with ADHD-BD should be achieved using mood stabilizers prior to initiation of ADHD pharmacotherapy.
-
There are some case reports of atomoxetine-associated hypomanic induction, while methylphenidate and amphetamine salts are considered to be low-risk medications in patients receiving appropriate mood stabilization therapy, but amphetamine salts carry double the risk than methylphenidate.
-
Monitor for drug–drug interactions, particularly between methylphenidate and anti-seizure medications that are being used for mood stabilization.
2.2. Borderline Personality Disorder
Much like bipolar disorder, the management of ADHD is challenging for providers of psychiatric care. The diagnostic features of ADHD and borderline personality disorder (BPD) share overlapping characteristics, including impulsivity, emotional dysregulation, and issues with attention and concentration. There is also evidence of greater treatment resistance in patients with comorbid ADHD and BPD when compared to those with either disorder in isolation [23].
There have been case reports published detailing the successful use of methylphenidate for the treatment of comorbid ADHD and BPD, demonstrating that methylphenidate monotherapy is effective not only for ADHD symptom management but also for aggression and self-injurious behavior seen in BPD [22]. There are many features of BPD and ADHD that overlap, and it is estimated that up to 1/3 of patients with BPD have a comorbid diagnosis of ADHD [58]. Because of the similarities in symptoms, including impulsivity, emotionality, and cognitive dysfunction, the well-known ADHD treatment methylphenidate was investigated in patients with a dual BPD diagnosis. One study demonstrated that participants in the methylphenidate treatment group had performed significantly better on tasks of decision-making, which was attributed to the changes in dopaminergic transmission mediated by the drug [59]. It was also shown that methylphenidate treatment in patients with ADHD-BPD resulted in fewer mood episodes and decreased likelihood of expressing anger, the latter of which is a known feature of emotional lability in BPD [60]. In one study with ADHD patients, the non-stimulant ADHD medication atomoxetine was superior to placebo for the management of emotional symptoms such as irritability and emotional volatility; the fact that these are also features of BPD indicates that atomoxetine therapy may be a potential therapeutic choice for patients who suffer from comorbid ADHD and BPD [61].
Similar investigations have identified that mood stabilization should be achieved before initiating ADHD treatment and that methylphenidate and amphetamine salts should both be avoided in patients with pervasive cluster B personality disorders that have malingering features [43]. According to the American Psychiatric Association guidelines, mood stabilization can be achieved using both psychotherapeutic and pharmacologic modalities [62]. Medication selection depends largely on the presenting phenotype of the patient; patients with high levels of impulsivity or agitation may benefit from a second-generation antipsychotic such as aripiprazole or olanzapine [63]. Certain anticonvulsants like topiramate and lamotrigine have some limited or mixed evidence for mood stabilization in BPD patients with features of anxiety and anger [63].
When available, psychotherapeutic modalities should be engaged with these patients to maximize treatment outcomes and allow patients to benefit from a multi-pronged approach to care. Dialectical behavior therapy (DBT) is a psychotherapeutic method adapted from the traditional cognitive-behavioral therapy (CBT) that focuses on skill building for patients with some function-impairing features of BPD, including an unstable sense of self, relationship instability, emotional lability, and impulsivity that may manifest as self-destruction. It is currently the first-line and most evidence-based treatment for BPD [64]. It is administered by a trained professional and can be performed in either the individual or group setting. DBT is well-known to be effective in managing BPD; however, one study in predominantly female patients with ADHD-BPD demonstrated that its efficacy in enhancing mindfulness skills and reducing feelings of depression and hopelessness are also appropriate and useful in the management of ADHD symptoms [60]. While DBT and other psychotherapy modalities are helpful, there are several factors that need to be considered when incorporating these approaches into the treatment plans—including patient preference, the therapeutic relationship between patient and therapist, and the availability of high-quality services in the community [39]. It has also been identified that effective pharmacological management of ADHD in the BPD setting will help to produce enhanced functioning, decreased distress and inner tension, greater control over behavior, and potentially stronger engagement in psychotherapy in patients with both diagnoses [10].
Aside from DBT, there are other therapeutic options that may be available to patients if there are trained clinicians with the ability to provide these specialized services. Mentalization-based therapy and transference-focused therapy are examples of alternative psychotherapeutic modalities that have been proven to be helpful in the outpatient management of BPD, although they have not yet been studied in the ADHD-BPD population. Mentalization-based therapy can also be administered as either individual or group therapy, and it helps patients work through their impulses and develop strategies to think before reacting [65]. Because of its ability to aid in the control of impulsive behaviors, it has been theorized that its principles may be applied to patients with ADHD of the hyperactive-impulsive subtype. Transference-focused therapy is a psychoanalytic technique that has also proven to be effective as a therapeutic modality for patients with BPD; while it requires extensive training and is not commonly practiced, it may be another consideration for patients with BPD and comorbidities in areas where it is available [66].
Many off-label medications have been trialed for the management of ADHD when comorbid with BPD. Some of the symptoms of BPD, including feelings of emptiness, fear of abandonment, and identity disturbance, have been proven to be resistant to treatment with various agents, including olanzapine and quetiapine [10]. Clonidine, an alpha-2 receptor agonist, is known to be an effective adjunct treatment for ADHD; its efficacy is poorly understood but hypothesized to be helpful in the setting of ADHD management because of its actions on neurotransmitters like norepinephrine [67]. This medication has been shown to reduce inner tension and the urge to engage in self-harm behaviors, characteristics often observed in BPD. Thus, it can be considered a management strategy for patients who present with diagnoses of both ADHD and BPD [10].
Clinicians should also consider the risks and management difficulties that may accompany the treatment of a patient with ADHD-BPD. It is well-documented that patients with BPD have a propensity to use substances due in part to the symptoms of impulsivity that they experience and the experiences of inner tension and suicidality that often provoke the use of alcohol and drugs as a coping mechanism [68]. It is estimated that up to 78% of patients with BPD have a comorbid substance use disorder, so clinicians should take caution when prescribing psychoactive medications like stimulants, which have the potential for abuse, to patients with BPD [69].
It is evident that research into the management implications of ADHD-BPD is limited and that further investigations should be performed to better understand the unique needs of this patient population.
Key Points:
Methylphenidate treatment can be helpful not just in the management of ADHD symptoms but also in certain features of BPD, including impulsivity and executive dysfunction.
-
Mood stabilization should be achieved before initiating stimulant therapy, and special caution should be taken in patients with suspected malingering behaviors.
-
Dialectical behavior therapy remains the gold standard treatment for BPD, and it has shown to be effective in mitigating certain features of ADHD as well.
This entry is adapted from the peer-reviewed paper 10.3390/brainsci13111517
This entry is offline, you can click here to edit this entry!
