The thyroglossal duct cyst (TGDC) is the most common congenital neck mass, accounting for 70–75% of all congenital neck masses. Although the Sistrunk operation has been used as a standard of treatment, it is accompanied by a considerable surgical burden, including the need for general anesthesia, a visible surgical scar on the neck surface, and postoperative complications. Ultrasound-guided ethanol ablation (US-EA) is a minimally invasive and office-based technique that is widely used as a non-surgical treatment for several benign cystic lesions, particularly benign thyroid cysts. US-EA has also been gaining popularity as a good alternative for TGDC treatment, which is associated with high feasibility, a high safety profile, and favorable treatment outcomes.
1. Introduction
The thyroglossal duct cyst (TGDC) is the most common congenital neck mass and a remnant of the thyroid anlage during embryonic development of the thyroid gland, representing more than 70–75% of congenital neck masses [
1,
2,
3,
4,
5]. Although TGDC is benign in most cases and may have minimal clinical significance, treatment is usually recommended based on various reasons, such as cosmetic issues, recurrent infections, and concerns of occult malignancy [
2,
6,
7,
8].
Most otolaryngology textbooks and studies on TGDC elucidate that the treatment of TGDC is primarily surgical, while other treatment options are rarely suggested [
1,
2,
4,
9]. In terms of surgical treatment, the Sistrunk procedure, which involves the complete excision of the TGDC and a central portion of the hyoid bone, has been considered the surgery of choice since its first introduction in 1920 [
1,
4]. Although this procedure remarkably contributed to the successful management of TGDC by reducing the recurrence rate to 1–5% from 45–55% after simple excision, it entails various surgical burdens, including the need for general anesthesia, a visible surgical scar on the neck surface, and possible postoperative complications [
1,
3,
4,
7,
10]. Particularly, given that the most common clinical presentation of TGDC is a painless neck mass, the most common rationale for TGDC treatment is the resolution of the cosmetic deformity caused by the TGDC mass; surgery may not be a patient-oriented treatment as it usually leaves postoperative surgical scars, defeating the purpose of resolving the cosmetic problems as a result of the TGDC [
2,
7].
2. Overall Practice of EA for TGDC
2.1. Pre-Procedural Evaluation
A benign TGDC must be accurately diagnosed before EA, thereby differentiating it from dermoid or lymph nodes. Moreover, possible occult malignancy from TGDC should also be considered, even though it is an extremely rare condition with an incidence rate of approximately 1–2% [
6,
17]. Ultrasonography (US) and computed tomography scans are the commonly used imaging modalities for evaluating the characteristics of TGDC. Additionally, US-guided fine-needle aspiration cytology (US-FNAC) is routinely performed to diagnose benign TGDC and rule out malignancy. In some patients, the measurement of thyroglobulin levels in the washout fluid of the FNAC needle could be helpful in differentiating thyroid follicle-containing lesions (benign TGDC or TGDC carcinoma) from other lesions (dermoid or lymph node).
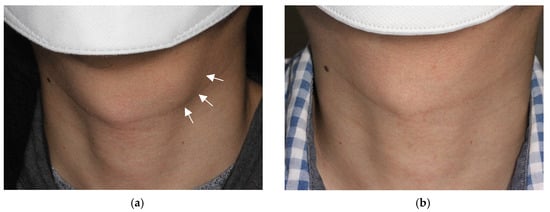
The baseline volume of TGDC is determined by measuring the diameters of the largest axis (a) and the two remaining perpendicular axes (b, c) on US. Using the formula for measuring the volume of an elliptical sphere (V = πabc/6), the volume is calculated. The volume reduction rate (VRR) is calculated as follows: VRR = (initial volume − final volume)/initial volume × 100% after treatment. The cosmetic deformity caused by TGDC is assessed using the World Health Organization (WHO) cosmetic scoring system (1, no palpable lesion; 2, with palpable lesion but no cosmetic problem; 3, lesion visible only to an experienced physician; and 4, easily visible mass) (Figure 1).
Figure 1. Photograph of an external neck with a thyroglossal duct cyst. The mass (arrows) is easily visible in the off-midline anterior neck at the hyoid level, being classified as World Health Organization (WHO) cosmetic score 4 (
a). After ethanol ablation, the mass is no longer identified on physical examination, with a classification of WHO cosmetic score 1 (
b).
2.2. Aspiration of Internal Contents and Ethanol Injection
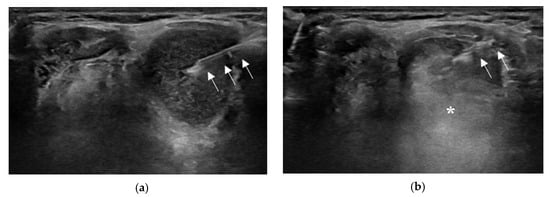
The US-EA technique is quite simple, and the procedure is generally performed in an outpatient setting. Patients are placed in a supine position with their necks extended. After the needle path is planned with the US examination, an alcohol swab is used to sterilize the skin, similar to the FNAC procedure. Local anesthesia is not mandatory because the procedure is usually completed with a single needle puncture. After the needle is inserted into the cyst under real-time US monitoring, the cystic fluid is aspirated as much as possible. Subsequently, 99% sterile ethanol is injected into the cystic cavity (Figure 2).
Figure 2. Ultrasound (US)-guided ethanol ablation procedure. The needle (arrows) is inserted into the cyst under real-time US monitoring (
a). After cystic fluid aspiration, 99% sterile ethanol is injected into the cystic cavity, which appears as a hyperechoic flush (asterisk) on real-time US (
b).
2.3. Technical Issues or Variations in EA for TGDC
2.3.1. Local Anesthesia
Of the seven studies published since 2011, only the two studies by Lee et al. and Park et al. stated that local anesthesia was performed by injecting lidocaine [
14,
16]. The two studies by Chow et al. and Ahn et al. clearly stated that local anesthesia was not used, while the remaining three studies did not include any description regarding local anesthesia use [
7,
12,
13,
15,
18].
2.3.2. Needle Size Used for EA
In EA for TGDC, 18–23-gauge needles are used, and various needle sizes can be used in a single procedure [
7,
11,
12,
13,
15,
16,
18]. An 18-gauge needle was used in the two studies by Lee et al. and Karatay et al., while an 18- or 21-gauge needle was used in the two studies by Chung et al. and Park et al. [
12,
14].
2.3.3. Amount of Ethanol Injected
Although the appropriate amount of ethanol injection has not been investigated in studies on EA for TGDC, approximately ≥50% of the aspirate volume with ≤10 mL of ethanol is usually used, similar to the EA protocol for cystic thyroid nodules [
11,
13,
14,
15,
18]. Among the seven studies on EA for TGDC, the five studies by Kim et al., Chow et al., Lee et al., Chung et al., and Park et al. used 50% or more of the aspirate volume as the lowest limit of ethanol injection, using up to 15 mL of ethanol [
13,
14,
15,
16,
18]. However, the recent two studies by Karatay et al. and Ahn et al. used a relatively small volume of ethanol, which was ≤5 mL and ≤2.5 mL, respectively [
7,
12].
2.3.4. Retention or Aspiration of Injected Ethanol
Among the seven studies on EA for TGDC published since 2011, six studies explored whether the authors used retention or aspiration of the injected ethanol [
7,
12,
13,
14,
15,
16]. The four studies by Kim et al., Lee et al., Chung et al., and Park et al. used an aspiration method that involved aspiration of the injected ethanol at the end of the procedure with 5–10 min of retention time [
13,
14,
15,
16].
2.3.5. EA for TGDC with Viscous Internal Contents
A critical factor for treatment success in EA of a benign cystic lesion is the sufficient evacuation of the internal cystic fluid. Thus, a cystic mass with viscous internal contents could provide therapeutic challenges in EA. Although the literature elucidating specifically on EA for viscous TGDC is lacking, several techniques have been used for the successful evacuation of viscous cystic fluid based on the studies on EA for viscous thyroid cyst, which include normal saline irrigation to decrease viscosity, repeated ethanol injection with an interval period to liquefy the viscous contents, use of a large-bore needle or catheter, and use of a suction pump [
13,
15,
16].
2.3.6. Number of Treatment Sessions
In the studies on EA for TGDC, from one to six treatment sessions were reported [
7,
12,
13,
14,
15,
16,
18]. The mean number of treatment sessions ranged from 1 to 1.7 in seven different studies, and multiple treatments were provided in approximately 0.0–44.4% of patients [
7,
12,
13,
14,
15,
16,
18]. In the study by Kim et al., involving 11 patients with TGDC in 2011, repeat EA was performed in approximately 27% of patients [
13].
3. EA Results for TGDC
3.1. Treatment Efficacy
The treatment efficacy after EA is usually assessed using two parameters, that is, VRR and TSR. The VRR is an objective value of the volume decrease in TGDC calculated by the following formula: (initial volume − final volume)/initial volume × 100%; the TSR is a semi-objective value defined by physicians based on the VRR, and 50% or 70% of the VRR was commonly used as cutoff values for TSR in previous studies [
7,
13,
14,
15,
16,
18,
19].
Among the seven studies published since 2011, six studies reported their treatment outcomes using VRR, and the mean or median VRR at the last follow-up was 76.6–96.4% in different studies [
7,
12,
13,
14,
15,
16]. Although the definition of TSR was different among the studies, TSR was estimated in five studies, and it ranged from 77.8% to 96.4% [
7,
13,
14,
15,
16].
3.2. Outcome-Related Factors
Outcome-related factors were only evaluated in one study [
7]. In that study, the authors assessed the treatment outcomes of EA, including the VRR, TSR, and number of treatment sessions, according to TGDC characteristics such as the initial volume, presence of septation, presence of debris, and viscosity of the cyst fluid (low: watery; intermediate: creamy; high: sticky or gelatinous). However, they did not find any between-group differences in the VRR, treatment success, or number of treatment sessions as functions of TGDC characteristics. This might be primarily attributed to the small number of cases in each subgroup. However, in contrast, this finding may indicate that EA could provide consistent treatment efficacy regardless of the various characteristics of TGDC.
3.3. Complications
In the literature on EA for benign thyroid nodules, major complications such as dysphonia and infection with/without a thyroid abscess have been reported [
20,
21,
22]. Regarding EA for TGDC, only one case of wound infection treated with surgery has been reported [
16]. In a recent systematic review that evaluated the outcomes of chemical ablation for TGDC in 82 patients with EA from four studies, major complications were not identified [
11]. Although it would not be a true complication, pain has been reported as the most common adverse presentation associated with EA.
3.4. Cost
It is easily presumed that the cost of EA should be lower than that of surgery because EA is usually performed in an office-based setting without general anesthesia. However, data remain lacking regarding the cost or cost-effectiveness of EA for TGDC. Thus far, only one study published in 2017 addressed the cost of EA in comparison with surgery [
15].
4. Summary
EA is widely used as a non-surgical, minimally invasive treatment for various disease entities. Cystic thyroid nodules are the most common candidates for EA use, and the clinical practice and detailed technique have been well established through several international guidelines and consensus statements [
23,
24,
25,
26]. Moreover, treatment efficacy and EA complications for thyroid nodules have also been comprehensively understood based on several review articles and meta-analyses [
20,
21].
4.1. Needs for Local Anesthesia
Because TGDC does not involve sensory innervation and the procedure is completed with a single needle puncture, EA for TGDC could be performed in an outpatient setting even without local anesthesia. Although Ahn et al. reported that most patients (92.9%) experienced mild-to-moderate pain during withdrawal of the inserted needle, the small amount of ethanol leakage through the needle puncture site is inevitable during needle withdrawal following ethanol injection, causing mild pain [
7]. Therefore, such pain could not be prevented by local anesthesia. Moreover, pain should not be prevented because the development of unexpected pain during ethanol injection is an important sign of inadvertent ethanol seepage, which may lead to surrounding tissue damage.
4.2. Needle Size Used for EA
Various needle sizes (18–23-gauge) have been used for EA in the literature [
7,
12,
13,
14,
15,
16,
18]. No rule or consensus exists regarding which needle size is the most optimal for EA in TGDC. The needle size should be determined and individualized based on the TGDC characteristics, particularly the volume and viscosity of the internal contents.
4.3. Amount of Ethanol Injected
The available literature and evidence discussing the appropriate amount of ethanol in EA for TGDC are limited. In 71.4% (5/7) of the studies published since 2011, at least 50% of the aspirate volume was used as the volume of the ethanol injection. Moreover, an amount of ethanol up to 90% of the aspirate volume was also reported. Indeed, there is no consensus on the appropriate amount of ethanol in EA for TGDC; thus, most studies on EA for TGDC adopted an EA protocol for cystic thyroid nodules, where the technique or practice of EA is well-established. However, even in EA for cystic thyroid nodules, the scientific background or rationale for using an ethanol volume of ≥50% of the aspirate volume has not been investigated. In fact, a recent systematic review of EA for cystic thyroid nodules involving 19 studies reported that a lower volume of ethanol injection (<50% of the initial cyst volume) was significantly associated with a higher VRR [
20].
4.4. Retention or Aspiration of Injected Ethanol
Although four out of the seven studies used aspiration methods (aspiration of injected ethanol after a short retention time), there is no consensus on whether ethanol should be fully aspirated after instillation [
13,
14,
15,
16,
24]. In the aspiration method, the retention time was 5–10 min [
13,
14,
15,
16]. Referring to the study of EA for benign thyroid cysts, aspiration of the injected ethanol is preferred, based on the theoretical rationale that the retention of the injected ethanol may increase patient inconvenience and cause complications due to possible ethanol leakage [
23,
30,
31]. The studies on EA for benign thyroid cysts by Kim et al. and Park et al. showed no difference in VRR or complications in the groups in which ethanol was retained or aspirated after injection, while other studies have suggested that the complete removal of ethanol after a short retention time decreases the rates of ethanol leakage and may increase patient satisfaction after the procedure [
24,
30,
31]. However, injected ethanol retention may be associated with better treatment outcomes because the duration of the chemical reaction would be much longer than with the aspiration method.
4.5. Number of Treatment Sessions
In contrast to surgery, EA may be associated with multiple courses of treatment. The mean number of EA sessions ranged from 1 to 1.7. Of the 206 patients from the seven studies, 41 patients (19.9%) received multiple sessions of EA for various reasons, including failure to achieve treatment success after the first session of EA, regrowth of the mass during follow-up, and prevention of possible recurrence [
7,
12,
13,
14,
15,
16,
18]. However, no study has revealed which factors are associated with the need for multiple sessions of EA to achieve treatment success, and those may involve several patient/TGDC characteristics such as age, sex, history of infection, initial volume, septation, debris, and cyst fluid viscosity.
4.6. Potential of EA as a Primary Treatment of TGDC in Terms of Feasibility, Safety, and Treatment Efficacy
EA is an office-based, minimally invasive technique that does not require anesthesia. Additionally, according to a recent study by Ahn et al., all procedures are completed within 10 min in an outpatient setting without hospitalization [
7]. Conversely, the Sistrunk operation is usually performed under general anesthesia and requires 1–2 h of surgical time. Therefore, EA may provide a higher degree of feasibility for TGDC treatment compared with the Sistrunk operation for both patients and surgeons, being less restricted by the patient’s comorbidities, treatment time, and treatment place. In terms of safety, the overall complication rate after EA is <1%, and no major complications have been reported, while the Sistrunk operation has been associated with 7.5–33% of the overall complication rate [
10,
32,
33,
34].
4.7. Practical Limitations of EA for TGDC
EA is challenging to use for complicated TGDCs, particularly TGDCs with a cutaneous fistula, because the retention of injected ethanol within the cyst is not feasible. Additionally, this technique may require general anesthesia for pediatric patients who cannot cooperate during the procedure. Given the fact that approximately 50% of TGDCs manifest in pediatric patients, additional studies involving pediatric patients should be performed for EA to be recognized as a true primary treatment for all patients with TGDC [
2,
9].
This entry is adapted from the peer-reviewed paper 10.3390/jcm12175445