Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Microbiology
The recurrence of bacterial infectious diseases is closely associated with bacterial persisters. This subpopulation of bacteria can escape antibiotic treatment by entering a metabolic status of low activity through various mechanisms, for example, biofilm, toxin–antitoxin modules, the stringent response, and the SOS response.
- bacterial persistence
- persister formation
- single-cell techniques
1. Introduction
In 1944, Joseph Bigger reported a small number of survivors, namely persisters, for the first time when he was studying staphylococcus treated with intermittent penicillin sterilization. Unlike resistant strains, descendants of persisters are susceptible to penicillin, suggesting that survival ability is inheritable [1]. Since then, an increasing number of reports have indicated that persisters are associated with relapsing infections and can survive therapy in diseases such as tuberculosis and urinary tract infections, despite the susceptibility to antibiotics seen in clinical laboratory tests [2]. Persister is a bacteria subpopulation that grows slowly or in a dormant manner. The state of persistence can be induced by a variety of mechanisms, and their antibiotic susceptibility is generally reduced due to dormancy [3]. This feature of persisters makes them unable to be completely eliminated during antibiotic treatment, which increases the likelihood of resistance and can lead to infection recurrence [4]. It is generally believed that persisters are crucial for pathogens to survive antimicrobial chemotherapy when the host’s immune response is limited [5]. The incidence of persister infections is especially high in immunocompromised patients with the human immunodeficiency virus or those undergoing cancer chemotherapy. For example, increased numbers of persister cells of Pseudomonas aeruginosa (P. aeruginosa) are a major concern for immunocompromised and cystic fibrosis patients, leading to high morbidity and mortality [6]. However, in immunocompetent individuals in cases where the pathogen is located at sites poorly accessible by components of the immune system, persister formation is also likely to take place [5]. Consequently, the site of infection would play a role in persister formation.
With the studies of persistence, a few intracellular bacteria have recently been found to exhibit a persistent phenotype [7]. One of the most distinctive features of persistence is the biphasic killing curve resulting from the coexistence of antibiotic-susceptible and persistent cells [8]. After being exposed to antibiotics, the most susceptible bacteria are rapidly killed, while a small proportion of persisters survive longer in a non-growing state (Figure 1). Once antibiotics are removed, persisters recover to grow and exhibit similar patterns to antibiotic-susceptible bacteria [9,10]. Besides antibiotics, some other stress environments, such as acid, toxic metals, and high temperatures, can also induce persister formation [11]. Nonetheless, antibiotic-induced persistence is of more concern in the hospital setting. In the clinic, antibiotic treatment is usually administered at regular dosages and times. Therefore, the antibiotic concentration in vivo fluctuates periodically [12]. In long-term treatment patients who received periodic antibiotics of a high concentration, the proportion of persisters in isolated P. aeruginosa was 100 times higher than during the early stages of treatment. However, the minimum inhibitory concentration (MIC) did not change significantly [13]. Accordingly, the failure of antibiotic treatment may not be solely due to resistance, as persistence may also play a role.
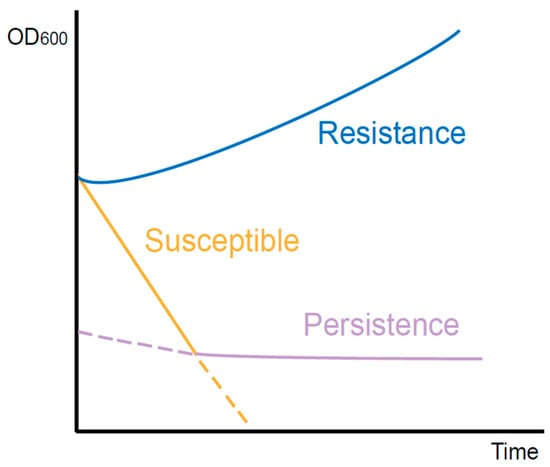
Figure 1. Killing curves of different types of bacteria during antibiotic exposure. The resistant bacteria continue to grow. The susceptible bacteria are killed quickly. However, with the existence of persisters, the curve declines slowly.
2. The Difference between Persistence and Resistance
Resistance to antibiotics is generally inherited through genetic mutations in bacteria. Despite high antibiotic concentrations, these resistant cells are still capable of dividing. The mechanisms of resistance have been deeply studied by researchers worldwide and can be categorized into three common pathways [14]. Firstly, bacteria reduce the intracellular antibiotic concentration in the way of either activating efflux pumps or decreasing the permeability of their membranes. Secondly, they actively modify the intracellular targets of antibiotics, thereby avoiding antibiotic attacks. Furthermore, by generating specific enzymes, antibiotics are directly inactivated within bacterial cells. As opposed to resistance, persistence is a heterogeneous population behavior. The vast majority of the population presents susceptibility to the stress, which is not impacted by the non-growth persister component. This susceptible feature can remain stable over generations, suggesting that all bacteria within the population have the same genetic background as persisters. Therefore, antibiotic persistence is a phenotypic change that occurs in a small proportion of cells. Compared to the stable and heritable resistance of antibiotic resisters, the ability of persisters to survive lethal antibiotics is transient and reversible [15].
Although the bacterial population containing persisters exhibited antimicrobial susceptibility, the killing curve of surviving persisters was independent of antibiotic concentration. However, the mortality rate of antibiotic-resistant bacteria was associated with antibiotic concentration when this was higher than the MIC [4]. Additionally, resistance is often specific to a certain class of drug, while persistence responds to a wide range of stimuli, including antibiotics. This reflects the differences in the underlying molecular mechanisms of the two species.
3. Research on the Mechanism of Bacterial Persistence
3.1. Biofilm
Persistence and biofilm formation have been shown to be closely related in numerous studies [16,17,18]. Bacteria attach irreversibly to the surface of inert or active entities, secrete proteins and polysaccharide matrix, and form a kind of membrane by wrapping the bacterial colonies. This membrane has strong selective permeability to nutritional and antibacterial compounds [19]. As a result, the biofilm provides shelter for potential persisters to escape antibiotics and immune molecules [12]. Existing studies have mainly emphasized the physical protection effect of biofilm. However, increasing evidence indicates that hypoxia and low nutrition in the inner biofilm also contribute to persister formation [20]. The tricarboxylic acid cycle would be downregulated in persisters inside the biofilm when exposed to antibiotic-induced oxidative stress, thereby preventing the production of reactive oxygen species, an essential component of antibiotic-induced bacterial killing [21]. A real-time impedance-based technology was used to examine the kinetics of P. aeruginosa biofilm growth under regular antibiotics [22]. The results showed that biofilm formation rate and outcome varied between different culture media. Although antibiotics can delay biofilm growth and reduce its amount, biofilm formation cannot be completely inhibited at a low antibiotic concentration. Based on these findings, a ‘fortress model’ of central persisters’ growth in the biofilm was proposed [23] (Figure 2). Nonetheless, bacteria at the periphery of the biofilm can form stronger biofilms that are resistant to antibiotics due to their easier access to nutrients than those growing in the core of the biofilm [24,25]. These studies suggest that nutrition gradients may influence the persister. However, it is still controversial whether growing at the periphery or core of the biofilm facilitates persister formation. Furthermore, the deficiency of the capsule can lead to the biofilm formation. It has been reported that in carbapenem-resistant Klebsiella pneumoniae (K. pneumoniae), the mutants that have deletions of core capsule biosynthesis genes produce more robust biofilm compared with the wild type, enhancing epithelial cell invasion and persistence in urinary tract infections [26].
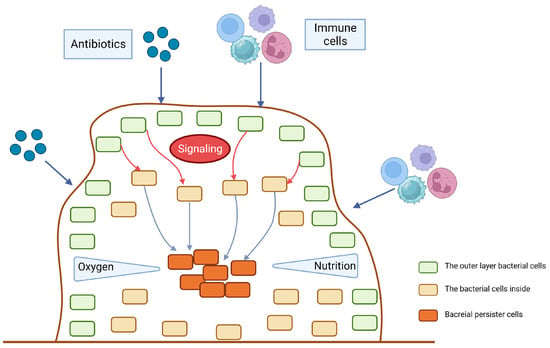
Figure 2. The fortress model. When antibiotics, immune cells or other potential environment stress start to stimulate the surface of the biofilm, the outer layer of bacteria will send signals to the bacteria inside to be alert to the bactericidal attack. The gradient of nutrition and oxygen will also contribute to the persister dormancy.
3.2. Toxin–Antitoxin Modules
Bacterial toxin–antitoxin (TA) modules extensively exist in a variety of cellular processes [27], and are composed of a toxin protein that inhibits cell growth by interfering with important metabolic activities and an antitoxin that can protect cells from toxins [3,28]. Some experiments have demonstrated that breaking the balance between the toxin and antitoxin would lead bacterial growth to a stagnant state, and then weaken the harm of antibiotics or other unfavorable circumstances, which could facilitate the survival of bacteria [13,29]. Environmental stress can induce a graded and controlled activation of toxins to help bacteria enter a transient dormancy state, which is the basis for surviving high-concentration antibiotics [30]. For example, the stress inside the host macrophages is more severe than the nutritious culture medium, providing more triggers for the TA modules’ activation [2]. To date, TA systems can be divided into eight types based on the properties and working modes of antitoxin, named type I to type VIII, following the discovery order. Type I antitoxins are small RNAs that inhibit the cognate toxin’s expression by silencing their transcript. Type II antitoxins are proteins that neutralize the cognate toxin by binding to them and forming tight complexes [31]. While type I TA modules were the first to be discovered, type II are the most abundant and diverse, occurring in the majority of bacteria and some archaea. Since the discovery of type I and type II TA modules on bacterial chromosomes, they have been recognized as beneficial factors in the face of stressful conditions including antibiotic persistence [17]. For type I TA systems, high persistence was reported to be positively correlated with the levels of ObgE and HokB. Obg is a conserved GTPase that plays an important role at the crossroads of the major cellular processes of translation and DNA replication, which are considered to be repressed in dormant persister cells. HokB, a toxin encoded by a type I toxin–antitoxin module, can provoke a collapse in the membrane potential [32]. The gene high persistence protein A (hipA)-encoding type II toxin was firstly discovered in Escherichia coli (E. coli), whose corresponding antitoxin is HipB [33,34]. It was reported that strains carrying hipA7 mutants produce persisters at a frequency of 1% compared to 10-5 in wild-type strains when exposed to ampicillin [35]. As the bacterial cell density increases, hipA7 strains also produce persistent cells at an increasing frequency. In addition, the deficiencies of more than five type II TA modules in E. coli would decrease persister formation during the exponential phase [36]. Beside the mutations on TA module components, the expression of TA modules in enriched E. coli persisters was obviously upregulated compared with normal growing bacteria [33,36]. Furthermore, the Lon protease, a kind of ATPase in E. coli, is required for the degradation of the antitoxin, and results in the accumulation of toxins to promote persister formation [29].
Current studies have been focused on Gram-negative bacteria, especially E. coli, though the study on Gram-positive bacteria is not clear. There is evidence that the absence of the TA module in Staphylococcus aureus (S. aureus) would not affect the persister level [37]. Nonetheless, it was proposed that TA modules in Gram-positive bacteria work similarly to those in Gram-negative bacteria, and take part in the host’s stress response [38].
3.3. ppGpp and Stringent Response
If cells encountered amino acid starvation, protein synthesis and other metabolic activities would be closed. This phenomenon is called the stringent response, a type of conservative and global transcriptomic adaptation to environmental pressure [39]. Many studies have confirmed that the stringent response can facilitate persister formation by lapsing into dormancy [7,40,41]. The small molecule guanosine tetraphosphate (ppGpp), controlled by Rel/Spo homolog and small alarmone synthetase proteins, is the central molecule in the stringent response [41,42]. In many biological and animal models, the bacterial mutants that cannot produce ppGpp usually show a reduced ability of persister formation [25,43,44,45]. In the stationary phase, the elevated recruitment of ppGpp to Obg GTPase results in the excessive binding of Obg to the 50S ribosome subunit, which reduces the levels of active 70S ribosomes and thereby regulates cellular functions and participates in various stress adaptions like the stringent response [32,46]. In persisters, Obg induces the expression of HokB, a membrane-targeted type I toxin, which can damage proton motion and block ATP synthesis, leading to dormancy [32]. Recent evidence has put an emphasis on ppGpp instead of TA modules in persister formation [47]. The steady state of ppGpp is maintained by RelA and SpoT, while the former is a synthase, and the latter is a hydrolase with weak synthetic activity [48,49]. It has been proven that ciprofloxacin, cefepime, colistin, and amikacin can upregulate the expression of the relA gene to help persister formation [50]. However, without the presence of ppGpp, such as relA knockout mutants, persisters still exist [51], suggesting that the mechanism needs further investigation. PhoU is another persistence-related factor. PhoU homologs have been identified as phosphate-specific transport system accessory proteins that respond to the environmental Pi level. Deletion of the PhoU1 and PhoU2 in S. aureus caused an increase in both persistence and bacterial virulence [52]. In P. aeruginosa, a phoU mutant showed increased levels of intracellular ppGpp, affected antibiotic susceptibility, and decreased growth rate [53]. Interestingly, biofilm formation was not affected by the phoU mutation.
During the stringent response, the accumulation of ppGpp results in changes in multiple metabolic pathways, involving DNA replication, nucleotide synthesis, transcription, ribosome maturation, and lipid metabolism. For example, the stringent response decreases the initiation rate of DNA replication in E. coli [54], and controls 100S ribosome formation by transcriptional regulation in multiple species [55]. rRNA synthesis and genes involved in the metabolism of macromolecules, such as phospholipids, are generally repressed, while the transcription of nutrient transporters is increased to overcome nutrient limitations [56]. In addition, due to the decreased level of lysine during fatty acid starvation, RelA is distinctly activated and induces the synthesis of ppGpp [57].
To explore the mechanism of how the stringent response increases bacterial cytotoxicity, Thomas A Hooven et al. conducted transposon sequencing and RNA sequencing analyses on Streptococcus agalactiae (GBS) with human whole blood [39]. Except in the capsular polysaccharide genes, relA was identified to be essential for GBS survival in blood. In addition to promoting the persistence of GBS in host blood, the activation of a stringent response by relA can also enhance the expression of β-hemolysin/cytolysin, a toxin required for GBS virulence [58] through an arginine-mediated metabolism pathway. At present, a small molecule inhibitor aimed at the stringent response has been developed as a new type of antibacterial, and it has demonstrated the corresponding therapeutic effects in pre-clinical tests [59,60].
3.4. SOS Response
The SOS response plays an important role in DNA repair, which is controlled by two key factors: repressor factor LexA and inducible factor RecA [61]. RecA protein is a recombinase which is important for repairing bacterial recombinational DNA [62]. The failure of damage repair by the SOS response usually leads to cell death, while successful DNA repair may eliminate the lysis function of antibiotics [63,64]. High cell density within biofilms, together with oxidative stress, triggers DNA damage and evokes the SOS response [61]. For instance, Salmonella persisters could retain the function of initiating infection recurrence via RecA-mediated DNA repair [65]. In response to the stress changes, RecA mediates global transcription by stimulating the self-lysis of LexA [62,66]. In addition, the SOS response is proven to enhance the expression of fibronectin, helping biofilm formation [67]. For resuscitation experiments, it was also observed that after the removal of ofloxacin, the SOS response continuously increased in persistent E. coli cells [68] (Figure 3).
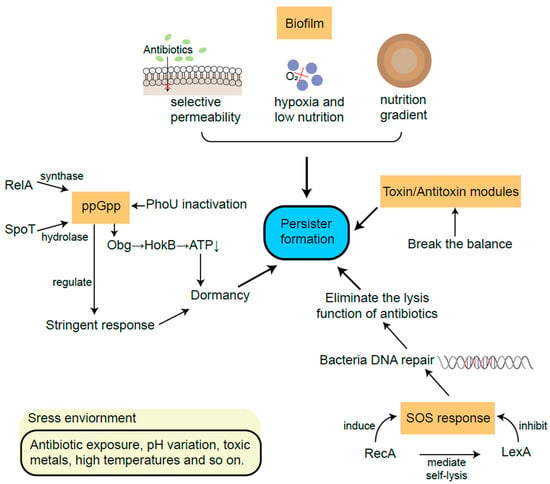
Figure 3. The main mechanisms of persister formation from biofilm, TA modules, ppGpp and SOS response.
Of the mechanisms described above, biofilm has been demonstrated in vivo in human pathology. For example, the biofilm formation of Mycobacterium tuberculosis in human lungs has been indicated to contribute to drug tolerance in experiments in animal models of infection and in the lung tissues of patients [69]. However, TA modules, the stringent response, and the SOS response have not been well elucidated in the physiopathology of specific diseases despite their documentation in vitro at the moment.
This entry is adapted from the peer-reviewed paper 10.3390/ijms241814311
This entry is offline, you can click here to edit this entry!
