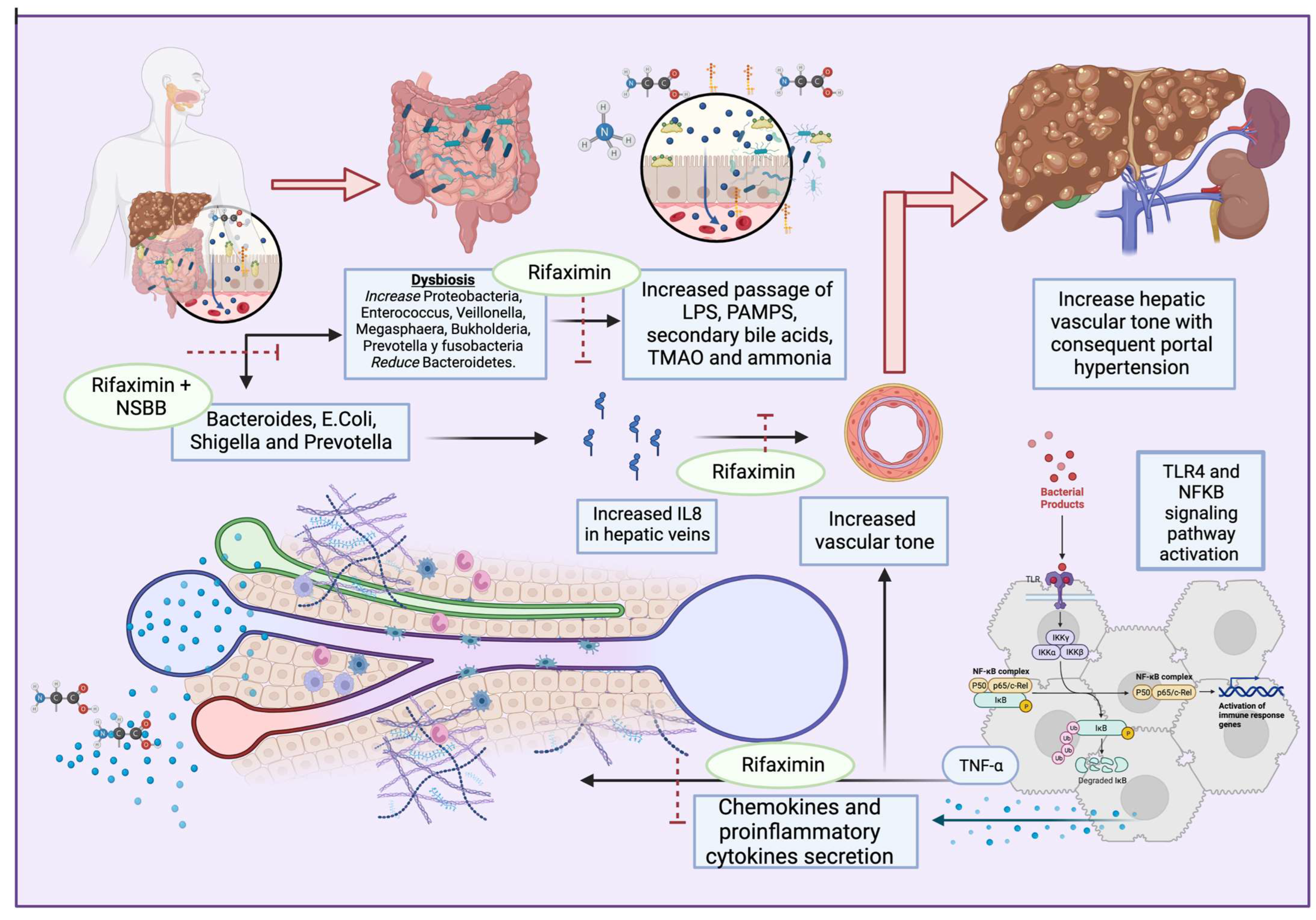
Impairments in liver function lead to different complications. As chronic liver disease progresses (CLD), hypoalbuminemia and alterations in bile acid compositions lead to changes in gut microbiota and, therefore, in the host–microbiome interaction, leading to a proinflammatory state. Alterations in gut microbiota composition and permeability, known as gut dysbiosis, have important implications in CLD; alterations in the gut–liver axis are a consequence of liver disease, but also a cause of CLD. Furthermore, gut dysbiosis plays an important role in the progression of liver cirrhosis and decompensation, particularly with complications such as hepatic encephalopathy and spontaneous bacterial peritonitis.
- dysbiosis
- gut microbiota
- liver cirrhosis
- antibiotics
- bile acids
1. Antibiotic Effects on Portal Hypertension
2. Prophylactic Antibiotic Use for Cirrhosis
3. Multidrug-Resistant Bacterial Infections in Patients with Cirrhosis and the Role of Gut Microbiota
This entry is adapted from the peer-reviewed paper 10.3390/antibiotics12101475
References
- Arab, J.P.; Martin-Mateos, R.M.; Shah, V.H. Gut-liver axis, cirrhosis and portal hypertension: The chicken and the egg. Hepatol. Int. 2018, 12 (Suppl. 1), 24–33.
- Di Tommaso, N.; Santopaolo, F.; Gasbarrini, A.; Ponziani, F.R. The Gut-Vascular Barrier as a New Protagonist in Intestinal and Extraintestinal Diseases. Int. J. Mol. Sci. 2023, 24, 1470.
- Touyz, R.M. Gut Dysbiosis–Induced Hypertension Is Ameliorated by Intermittent Fasting. Circ. Res. 2021, 128, 1255–1257.
- Li, M.; Li, K.; Tang, S.; Lv, Y.; Wang, Q.; Wang, Z.; Luo, B.; Niu, J.; Zhu, Y.; Guo, W. Restoration of the gut microbiota is associated with a decreased risk of hepatic encephalopathy after TIPS. JHEP Rep. 2022, 4, 100448.
- Lata, J.; Juránková, J.; Husová, L.; Senkyrík, M.; Díte, P.; Dastych, M.; Príbramská, V.; Kroupa, R. Variceal bleeding in portal hypertension: Bacterial infection and comparison of efficacy of intravenous and per-oral application of antibiotics–a randomized trial. Eur. J. Gastroenterol. Hepatol. 2005, 17, 1105–1110.
- Chavez-Tapia, N.C.; Barrientos-Gutierrez, T.; Tellez-Avila, F.; Soares-Weiser, K.; Mendez-Sanchez; Gluud, C.; Uribe, M.N. Meta-analysis: Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding–An updated Cochrane review. Aliment. Pharmacol. Ther. 2011, 34, 509–518.
- Zhang, H.; Gao, J. Antibiotics and probiotics on hepatic venous pressure gradient in cirrhosis: A systematic review and a meta-analysis. PLoS ONE 2022, 17, e0273231.
- Gedgaudas, R.; Bajaj, J.S.; Skieceviciene, J.; Varkalaite, G.; Jurkeviciute, G.; Gelman, S.; Valantiene, I.; Zykus, R.; Pranculis, A.; Bang, C. Circulating microbiome in patients with portal hypertension. Gut Microbes 2022, 14, 2029674.
- Mendoza, Y.P.; Rodrigues, S.G.; Bosch, J.; Berzigotti, A. Effect of poorly absorbable antibiotics on hepatic venous pressure gradient in cirrhosis: A systematic review and meta-analysis. Dig. Liver Dis. 2020, 52, 958–965.
- Lim, Y.L.; Kim, M.Y.; Jang, Y.O.; Baik, S.K.; Kwon, S.O. Rifaximin and Propranolol Combination Therapy Is More Effective than Propranolol Monotherapy for the Reduction of Portal Pressure: An Open Randomized Controlled Pilot Study. Gut Liver. 2017, 11, 702–710.
- Kemp, W.; Colman, J.; Thompson, K.; Madan, A.; Vincent, M.; Chin-Dusting, J.; Kompa, A.; Krum, H.; Roberts, S. Norfloxacin treatment for clinically significant portal hypertension: Results of a randomised double-blind placebo-controlled crossover trial. Liver Int. 2009, 29, 427–433.
- Gupta, N.; Kumar, A.; Sharma, P.; Garg, V.; Sharma, B.C.; Sarin, S.K. Effects of the adjunctive probiotic VSL#3 on portal haemodynamics in patients with cirrhosis and large varices: A randomized trial. Liver Int. 2013, 33, 1148–1157.
- Ferrarese, A.; Passigato, N.; Cusumano, C.; Gemini, S.; Tonon, A.; Dajti, E.; Marasco, G.; Ravaioli, F.; Colecchia, A. Antibiotic prophylaxis in patients with cirrhosis: Current evidence for clinical practice. World J. Hepatol. 2021, 13, 840–852.
- Gao, Y.; Qian, B.; Zhang, X.; Liu, H.; Han, T. Prophylactic antibiotics on patients with cirrhosis and upper gastrointestinal bleeding: A meta-analysis. PLoS ONE 2022, 17, e0279496.
- Tay, P.W.L.; Xiao, J.; Tan, D.J.H.; Ng, C.; Lye, Y.N.; Lim, W.H.; Teo, V.X.Y.; Heng, R.R.Y.; Heng, R.R.Y.; Lum, L.H.W.; et al. An Epidemiological Meta-Analysis on the Worldwide Prevalence, Resistance, and Outcomes of Spontaneous Bacterial Peritonitis in Cirrhosis. Front. Med. 2021, 8, 693652.
- Biggins, S.W.; Angeli, P.; Garcia-Tsao, G.; Gines, P.; Ling, S.C.; Nadim, M.K.; Wong, F.; Kim, W.R. Diagnosis, Evaluation and Management of Ascites, Spontaneous Bacterial Peritonitis and Hepatorenal Syndrome. Hepatology 2021, 74, 1014–1048.
- Yim, H.J.; Kim, T.H.; Suh, S.J.; Yim, S.Y.; Jung, Y.K.; Seo, Y.S.; Kang, S.H.; Kim, M.Y.; Baik, S.K.; Kim, H.S. Response-Guided Therapy with Cefotaxime, Ceftriaxone, or Ciprofloxacin for Spontaneous Bacterial Peritonitis: A Randomized Trial: A Validation Study of 2021 AASLD Practice Guidance for SBP. Am. J. Gastroenterol. 2023, 118, 654–663.
- Facciorusso, A.; Papagiouvanni, I.; Cela, M.; Buccino, V.R.; Sacco, R. Comparative efficacy of long-term antibiotic treatments in the primary prophylaxis of spontaneous bacterial peritonitis. Liver Int. 2019, 39, 1448–1458.
- Feuerstadt, P.; Hong, S.J.; Brandt, L.J. Chronic Rifaximin Use in Cirrhotic Patients Is Associated with Decreased Rate of C. difficile Infection. Dig. Dis. Sci. 2020, 65, 632–638.
- Pérez-Cameo, C.; Oriol, I.; Lung, M.; Lladó, L.; Dopazo, C.; Nuvials, X.; Los-Arcos, I.; Sabé, N.; Castells, L.; Len, O. Impact of Prophylactic Norfloxacin in Multidrug Resistant Bacterial Infections in the Early Liver Posttransplant Period. Exp. Clin. Transplant. 2023, 21, 236–244.
- Hurley, J.C. Selective digestive decontamination, a seemingly effective regimen with individual benefit or a flawed concept with population harm? Crit. Care 2021, 25, 323.
- Myburgh, J.; Seppelt, I.M.; Goodman, F.; Billot, L.; Correa, M.; Davis, J.S.; Gordon, A.C.; Hammond, N.E.; Iredell, J.; Li, Q. Effect of Selective Decontamination of the Digestive Tract on Hospital Mortality in Critically Ill Patients Receiving Mechanical Ventilation. JAMA 2022, 328, 1911–1921.
- Garcia-Tsao, G. Prophylactic Antibiotics in Cirrhosis: Are They Promoting or Preventing Infections? Clin. Liver Dis. 2019, 14, 98–102.
- Lutz, P.; Parcina, M.; Bekeredjian-Ding, I.; Nischalke, H.D.; Nattermann, J.; Sauerbruch, T.; Hoerauf, A.; Strassburg, C.P.; Spengler, U. Impact of Rifaximin on the Frequency and Characteristics of Spontaneous Bacterial Peritonitis in Patients with Liver Cirrhosis and Ascites. PLoS ONE 2014, 9, e93909.
- Higuera-de-la-Tijera, F.; Servín-Caamaño, A.I.; Salas-Gordillo, F.; Pérez-Hernández, J.L.; Abdo-Francis, J.M.; Camacho-Aguilera, J.; Alla, S.N.; Jiménez-Ponce, F. Primary Prophylaxis to Prevent the Development of Hepatic Encephalopathy in Cirrhotic Patients with Acute Variceal Bleeding. Can. J. Gastroenterol. Hepatol. 2018, 2018, 3015891.
- Coronel-Castillo, C.E.; Contreras-Carmona, J.; Frati-Munari, A.C.; Uribe, M.; Méndez-Sánchez, N. Eficacia de la rifaximina en los diferentes escenarios clínicos de la encefalopatía hepáticaEfficacy of rifaximin in the different clinical scenarios of hepatic encephalopathy. Rev. Gastroenterol. Mex. (Engl. Ed.) 2020, 85, 56–68.
- Ponziani, F.R.; Zocco, M.A.; D’Aversa, F.; Pompili, M.; Gasbarrini, A. Eubiotic properties of rifaximin: Disruption of the traditional concepts in gut microbiota modulation. World J. Gastroenterol. 2017, 23, 4491–4499.
- Yu, X.; Jin, Y.; Zhou, W.; Xiao, T.; Wu, Z.; Su, J.; Gao, H.; Shen, P.; Zheng, B.; Luo, Q. Rifaximin Modulates the Gut Microbiota to Prevent Hepatic Encephalopathy in Liver Cirrhosis Without Impacting the Resistome. Front. Cell. Infect. Microbiol. 2021, 11, 761192.
- Patel, V.C.; Lee, S.; McPhail, M.J.W.; Da Silva, K.; Guilly, S.; Zamalloa, A.; Witherden, E.; Støy, S.; Manakkat Vijay, G.K.; Pons, N.; et al. Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial. J. Hepatol. 2022, 76, 332–342.
- Dalbeni, A.; Mantovani, A.; Zoncapè, M.; Cattazzo, F.; Bevilacqua, M.; De Marco, L.; Paon, V.; Ieluzzi, D.; Azzini, A.M.; Carrara, E.; et al. The multi-drug resistant organisms infections decrease during the antimicrobial stewardship era in cirrhotic patients: An Italian cohort study. PLoS ONE 2023, 18, e0281813.
- Louvet, A.; Labreuche, J.; Dao, T.; Thévenot, T.; Oberti, F.; Bureau, C.; Paupard, T.; Nguyen-Khac, E.; Minello, A.; Bernard-Chabert, B.; et al. Effect of Prophylactic Antibiotics on Mortality in Severe Alcohol-Related Hepatitis: A Randomized Clinical Trial. JAMA 2023, 329, 1558–1566.
- Marciano, S.; Gutierrez-Acevedo, M.N.; Barbero, S.; Del, C.; Notar, L.; Agozino, M.; Fernandez, J.L.; Anders, M.M.; Grigera, N.; Antinucci, F.; et al. Norfloxacin prophylaxis effect on multidrug resistance in patients with cirrhosis and bacterial infections. Eur. J. Clin. Microbiol. Infect. Dis. 2023, 42, 481–491.
- Komolafe, O.; Roberts, D.; Freeman, S.C.; Wilson, P.; Sutton, A.J.; Cooper, N.J.; Pavlov, C.S.; Milne, E.J.; Hawkins, N.; Cowlin, M.; et al. Antibiotic prophylaxis to prevent spontaneous bacterial peritonitis in people with liver cirrhosis: A network meta-analysis. Cochrane Database Syst. Rev. 2020, 1, CD013125.
- Piano, S.; Singh, V.; Caraceni, P.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Mariano, M.; et al. Epidemiology and effects of bacterial infections in patients with cirrhosis worldwide. Gastroenterology 2019, 156, 1368–1380.e10.
- Fernández, J.; Prado, V.; Trebicka, J.; Amoros, A.; Gustot, T.; Wiest, R.; Deulofeu, C.; Garcia, E.; Acevedo, J.; Fuhrmann, V.; et al. Multidrug-resistant bacterial infections in patients with decompensated cirrhosis and with acute-on-chronic liver failure in Europe. J. Hepatol. 2019, 70, 398–411.
- Fernández, J.; Acevedo, J.; Castro, M.; Garcia, O.; de Lope, C.R.; Roca, D.; Pavesi, M.; Sola, E.; Moreira, L.; Silva, A.; et al. Prevalence and risk factors of infections by multiresistant bacteria in cirrhosis: A prospective study. Hepatology 2012, 55, 1551–1561.
- Kremer, W.M.; Gairing, S.J.; Kaps, L.; Ismail, E.; Kalampoka, V.; Hilscher, M.; Michel, M.; Siegel, E.; Schattenberg, J.M.; Galle, P.R.; et al. Characteristics of bacterial infections and prevalence of multidrug-resistant bacteria in hospitalized patients with liver cirrhosis in Germany. Ann. Hepatol. 2022, 27, 100719.
- Fernandez, J.; Piano, S.; Bartoletti, M.; Wey, E.Q. Management of bacterial and fungal infections in cirrhosis: The MDRO challenge. J. Hepatol. 2021, 75 (Suppl. 1), S101–S117.
- Delavy, M.; Burdet, C.; Sertour, N.; Devente, S.; Docquier, J.D.; Grall, N.; Volant, S.; Ghozlane, A.; Duval, X.; Ghozlane, A.; et al. A Clinical Study Provides the First Direct Evidence That Interindividual Variations in Fecal β-Lactamase Activity Affect the Gut Mycobiota Dynamics in Response to β-Lactam Antibiotics. mBio 2022, 13, e0288022.
- Shamsaddini, A.; Gillevet, P.M.; Acharya, C.; Fagan, A.; Gavis, E.; Sikaroodi, M.; McGeorge, S.; Khoruts, A.; Albhaisi, S.; Fuchs, M.; et al. Impact of Antibiotic Resistance Genes in Gut Microbiome of Patients with Cirrhosis. Gastroenterology 2021, 161, 508–521.e7.
