Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Otomycosis (OM) is a superficial fungal infection of the external auditory canal (EAC) with a worldwide prevalence ranging from 9% to 30%. Commonly, otomycoses are caused by Aspergillus (A.) niger complex and Candida spp. Other causative agents are yeasts of the genera Cryptococcus spp., Rhodotorula spp., Geotrichum candidum, dermatophytes (Trichophyton mentagrophytes), and non-dermatophytes molds (Fusarium spp., Penicillium spp., Mucorales fungi).
- otomycosis
- epidemiology
- etiology
- predisposing factors
1. Introduction
Otomycosis is a common superficial fungal infection that affects the external auditory canal (EAC). The infection may present as acute, subacute, or chronic, and is typically unilateral, with the bilateral form being more common in immunocompromised patients. The infection is present globally, with prevalence ranging from 9% to 30% in patients with the signs and symptoms of EAC infection [1][2][3]. The most common causative agents of otomycosis are molds of the genus Aspergillus and yeasts of the genus Candida, particularly Aspergillus (A.) niger complex and Candida (C.) albicans [4].
Recent molecular methods and analyses have revealed 28 different species of black molds within the Aspergillus niger complex, with A. tubingensis being the most common cause of otomycosis, followed by A. niger. Although rare, the species A. welwitschiae, A. awamori and A. foetidus have also been reported as the cause of this infection [5]. Accurate molecular identification of these black fungi is crucial for the development of rapid diagnostic tests for Aspergillus otomycosis, and for determining appropriate treatment for different species within this complex. Apart from the molds mentioned, species of A. flavus complex are also commonly isolated, while A. terreus, A. fumigatus, A. versicolor, and A. luchuensis are less frequent culprits [6]. In the last year, A. sydowii was identified as a potential human pathogen in immunocompromised patients, with two reported cases in which the fungi were molecularly identified from the EAC material obtained during tympanomastoidectomy [7].
In addition to C. albicans, C. parapsilosis has been established as a common cause of otomycosis, particularly in Europe, where its prevalence is high. Other Candida species such as C. lustaniae, C. guilliermondii, C. famata, C. tropicalis, C. krusei, and C. glabrata have also been isolated and identified as etiological agents of the EAC infection, although with relatively low incidence [8]. Moreover, C. auris, an emerging and highly virulent fungal pathogen, has been detected as a colonizer of EAC skin and a potential cause of the infection. This is of major concern due to its multi-drug resistance and potential for dissemination [9].
2. Treatment
The lack of official therapeutic guidelines and protocols has led to disagreement among experts on the optimal treatment for fungal infections. Moreover, the treatment duration is also undefined. Thus, careful consideration of the evidence, patient factors, and clinical judgment are crucial in determining the most appropriate approach [10][11]. Many authors believe it is necessary to identify the causative agent and choose the most effective antimycotic based on the previously determined specific sensitivity. However, other authors suggest that it is advisable to select an appropriate treatment based on the general effectiveness and characteristics of the drug, regardless of the pathogen type [12][13].
In France, nystatin is recommended as the first-line local treatment of otomycosis, typically used in combination with oxytetracycline, polymyxin B, and dexamethasone for up to 15 days [11]. Although this polyene has a wide spectrum of activity against both yeasts and molds, there are inconsistent opinions in the literature about its effectiveness against Aspergillus spp., one of the dominant causative agents in otomycosis [10][12]. On the other hand, in the USA, clotrimazole, as topical imidazole, is considered the drug of choice for the treatment of uncomplicated otomycosis [14]. Accordingly, recent research conducted in India suggests that 1% clotrimazole cream applied topically may effectively treat otomycosis [15]. However, some studies with smaller sample sizes do not classify clotrimazole as a first-choice drug due to its lesser effectiveness against Aspergillus-otomycosis [10][16][17].
Other antifungal agents, such as miconazole, bifonazole, isoconazole [18] and ciclopiroxolamine, can also be used for the treatment of otomycosis. However, in vitro studies and treatment monitoring have shown that these antifungals have an unequal effect on yeasts and molds, with miconazole being less effective against various species of the genus Candida [4][11]. Some studies have also reported good in vitro effectiveness of efinaconazole, lanoconazole, and luliconazole against Aspergillus species, but lower susceptibilities of ravuconazole were observed against A. tubingensis and A. niger, which are the most prevalent causative agents of otomycosis [19]. In a study conducted last year comparing the clinical efficacy of sertaconazole with other imidazoles, satisfactory effects were reported in patients with otomycoses, yet there was no significant difference observed compared to treatment with miconazole and clotrimazole [20].
A recent survey conducted in Russia involving over 300 patients with fungal ear infection recommended mandatory mycological control in addition to clinical examination to assess the effectiveness of therapy [21]. The results of this study revealed that terbinafine, naftifine, and chlornitrophenol were the most effective in local treatment for mold-induced otomycosis, while clotrimazole or allylamines (terbinafine and naftifine) were found to be the best choice for Candida otomycosis. It was noted that local antifungal treatments should be applied for at least 3–4 weeks with constant laboratory monitoring. Similar findings were reported in a study conducted in Serbia with an analogous design, which showed that nystatin and naftifine yielded better results in the treatment of patients with Aspergillus-otomycosis compared to clotrimazole [10].
These results support the potential effectiveness of allylamines, such as terbinafine and naftifine, in the treatment of otomycosis caused by yeasts or molds, as was also suggested in a recent study by Ting-Hua Yang, who demonstrated the non-toxicity of terbinafine to the inner ear end organs at a dosage of 0.4 mg [22].
Although various antiseptics, acidifying agents, and medications containing anti-infective agents with corticosteroids have been investigated for the treatment of otomycosis, there is insufficient evidence to support their increased efficacy compared to antimycotic drugs, as reported by Khrystyna Herasym in 2016 [23]. Moreover, extensive ear canal debridement followed by topical antifungal medications is recommended for patients with a noninvasive form of infection.
Another important fact is that antifungal ointments have distinct advantages over liquid formulations. Creams, due to their higher viscosity, remain longer on the skin’s surface and are considered safer for use in patients with perforated eardrums, as there is a lower chance of the drug entering the middle ear [24]. One recommendation for liquid formulations of antimycotics is to soak cotton wool or gauze pads in the solution and leave them in the ear canal for 5–10 min, 2–4 times a day [21]. In addition to all the described treatment modalities, it is crucial to restore the physiological conditions in the ear canal by avoiding excessive use of topical medications and protecting the ear canal from further damage, which can disrupt local homeostasis [25].
Systemic antimycotics, such as triazole antifungal drugs (fluconazole, itraconazole, voriconazole, posaconazole), may be used in severe forms of otomycosis, or when previous local therapy has been ineffective [13]. These drugs are effective against infections caused by fungi of the genera Candida and Aspergillus, and are essential in the treatment of complex forms of the disease, especially when there are complications such as mastoiditis and meningitis [26].
However, an investigation of in vitro antifungal susceptibility demonstrated that non-albicans Candida species, as causative agents of otomycosis, might have varying sensitivity in a dose-dependent manner to fluconazole (MIC = 32 mg/mL). Moreover, it was proven that C. krusei, besides fluconazole, also had lower sensitivity to itraconazole (MIC = 0.5 mg/mL) [4]. This highlights the importance of identifying specific causative agents and conducting susceptibility testing to guide the appropriate choice of systemic antifungal therapy in severe cases of otomycosis.
3. Epidemiology
From an epidemiological perspective, it can be stated that the climatic conditions of tropical and subtropical regions, characterized by long summers and rainy seasons, are the most common risk factors for the occurrence of otomycosis. A wide spectrum of different species and genera of fungi causing otomycosis has been isolated and identified in these areas. Specifically, numerous yeast and mold species have been identified in Asia [2][27][28], Africa [29], Central America [30], and South America [31] (Table 1, Figure 1). Surveys conducted in Europe have not noted any seasonal influence [4].
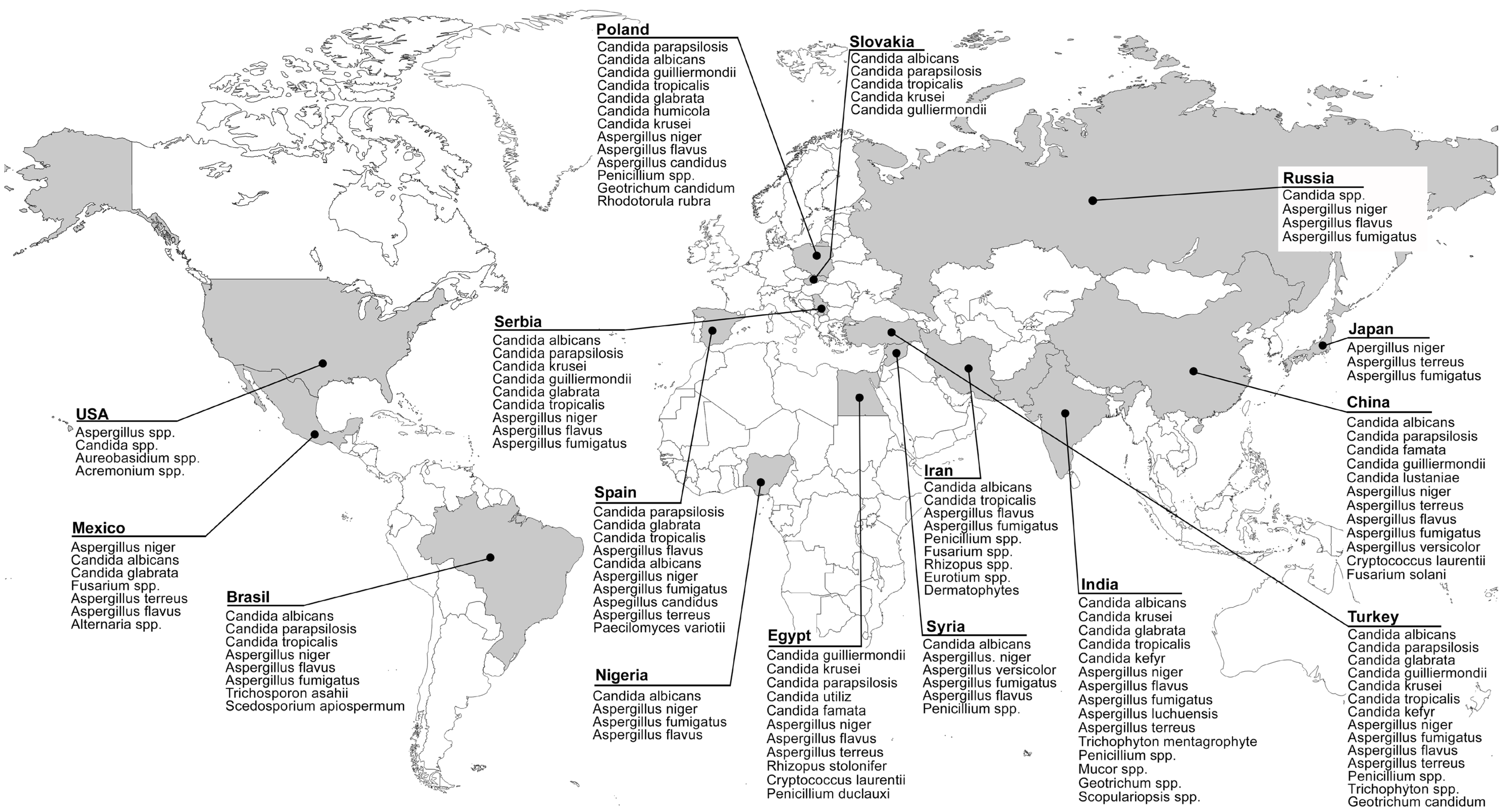
Figure 1. Distribution of otomycosis causative agents.
Table 1. Species distribution, clinical manifestations, and risk factors for otomycosis.
| Country (Sample Size *) |
Identified Fungal Species ** | Reported Signs and Symptoms *** | Predisposing Factors *** | References |
|---|---|---|---|---|
| Asia | ||||
| Japan (29 patients) |
A. niger, A. terreus, A. fumigatus | N/A | N/A | Hagiwara, S. et al. [19] |
| China (108 patients) |
A. niger, C. albicans, A. terreus, A. flavus, C. lustaniae, A. fumigatus, C. parapsilosis, C. famata, Cryptococcus laurentii, C. guilliermondii, A. versicolor, Fusarium solani | Pruritus, Otorrhea, Ear fullness, Hearing loss, Otalgia, Tinnitus | N/A | Jia, X. et al. [28] |
| India (30 patients) |
A. niger, A. flavus, C. tropicalis |
Pruritus, Otalgia, Ear fullness, Hearing loss, Otorrhea | Ear pricking with hard objects, Use of oil ear drops, Swimming or pond baths, Diabetes, Immunodeficiency | Panigrahi, M. et al. [32] |
| India (350 patients) |
A. niger, A. flavus, A. fumigatus, C. albicans, C. krusei, C. tropicalis, Penicillium spp., Mucor spp., Trichophyton mentagrophyte |
Hearing loss, Ear fullness, Pruritus, Otalgia, Otorrhea, Tinnitus | Ear pricking with hard objects, Use of oil ear drops | Agarwal, P. et al. [2] |
| India (100 patients) |
A. niger, A. flavus, A. fumigatus, C. albicans, C. tropicalis, C. glabrata,C. kefyr, Penicilium spp., Geotrichum spp., Scopulariopsis spp. |
Pruritus, Otalgia, Ear blockage, Tinnitus, Hearing loss, Otorrhea | Use of oil ear drops, Use of antibiotic or wax-dissolving ear drops, Ear pricking with hard objects, Diabetes, Swimming | Rawat, S. et al. [33] |
| India (100 patients) |
A. niger, A. fumigatus, A. flavus, Penicillium spp., C. albicans, Rhizospus spp., Chrysosporium spp. |
Pruritus, Ear fullness, Otorrhea, Otalgia, Tinnitus |
Use of oil ear drops, Ear pricking with hard objects, Use of antibiotic ear drops | Prasad, S.C. et al. [34] |
| Pakistan (180 patients) |
N/A | Hearing loss, Pruritus, Otalgia, Otorrhea, Tinnitus | N/A | Anwar, K. et al. [25] |
| Iran (129 patients) |
A. niger, A. flavus, A. fumigatus, C. albicans, Penicillium spp., Dermatophytes, C. tropicalis, Fusarium spp., Rhizopus spp., Eurotium spp. |
Pruritus, Ear fullness, Otorrhea, Otalgia | Ear pricking with hard objects, Diabetes | Kazemi, A. et al. [27] |
| Syria (70 patients) |
A. niger, C. albicans,A. versicolor, A. fumigatus, A. flavus, Penicillium spp. |
Otorrhea, Otalgia, Hearing loss | N/A | Ismail, M.T. et al. [35] |
| Turkey (87 patients) |
A. niger, A. fumigatus, A. flavus, A. terreus, C. albicans, C. tropicalis, C. kefyr |
Pruritus, Otalgia, Hearing loss, Tinnitus, Otorrhea | Wearing a traditional head covering, Swimming in the pool/sea, Spa baths, Itching on other body parts, Long-term antibiotic treatment, Rainy weather season | Ozcan, K.M. et al. [36] |
| Turkey (544 patients) |
A. niger, C. tropicalis, A. fumigatus, C. albicans, A. terreus, A. flavus, C. parapsilosis, C. glabrata, Penicillium spp., C. kefyr, C. guilliermondii, C. krusei, Trichophyton spp., Geotrichum candidum |
N/A | N/A | Değerli, K. et al. [8] |
| Africa | ||||
| Egypt (110 patients) |
A. niger, A. flavus | Pruritus, Otalgia, Hearing loss, Otorrhea | Ear canal trauma, Swimming, Use of antibiotic ear drops, Absent cerumen, Summer season | Abdelazeem, M. et al. [37] |
| Egypt (102 patients) |
A. niger, A. flavus, C. famata, A. terreus, C. parapsilosis, C. utiliz, Rhizopus stolonifer, C. guilliermondii, C. krusei, Cryptococcus laurentii, Penicillium duclauxi |
Pruritus, Otalgia, Otorrhea, Hearing loss, Tinnitus | N/A | Ali, K. et al. [29] |
| Nigeria (378 patients) |
A. niger, A. fumigatus, C. albicans, A. flavus | Pruritus, Otalgia, Tinnitus, Ear fullness, Hearing loss, Otorrhea | Ear pricking with hard objects, Long-term use of oral antibiotics, Use of antibiotic ear drops, Diabetes, Sino-nasal and nasopharyngeal malignancy, Retroviral infection | Fasunla, J. et al. [1] |
| Central America | ||||
| Mexico (40 patients) |
A. niger, C. albicans, C. glabrata, Fusarium spp., A. terreus, A. flavus, Alternaria spp. |
Pruritus, Hearing loss, Otorrhea, Otalgia | N/A | Alarid-Coronel, J. et al. [30] |
| North America | ||||
| USA (132 patients) |
Aspergillus spp. Candida spp. Aureobasidium spp. Acremonium spp. |
Otalgia, Otorrhea, Hearing loss, Ear fullness, Pruritus, Tinnitus | Diabetes, History of otologic procedures, Mastoid cavity after surgical procedure | Ho, T. et al. [38] |
| South America | ||||
| Brasil (20 patients) |
C. albicans, C. parapsilosis, A. niger, A. flavus, A. fumigatus, C. tropicalis, Trichosporon asahii, Scedosporium apiospermum |
Pruritus, Otalgia, Otorrhea, Hearing loss | Chronic otitis, Long-term antibiotic treatment, Absent cerumen, Ear pricking with hard objects | Pontes, Z.B. et al. [31] |
| Europe | ||||
| Poland (96 patients) |
C. parapsilosis, C. albicans, A. niger, A. flavus, Penicillium spp., C. guilliermondii, C. tropicalis, C. glabrata, C. humicola, C. krusei, A. candidus, Geotrichum candidum, Rhodotorula rubra |
Pruritus, Otorrhea, Ear fullness, Hearing loss, Tinnitus, Otalgia, EAC swelling and redness, Headache | N/A | Kurnatowski, P. et al. [39] |
| Slovakia (40 patients) |
C. albicans, C. parapsilosis, C. tropicalis, C. krusei, C. gulliermondii |
Burning sensation in the ear, Pruritus, Ear fullness, Hearing loss, Otalgia, Otorrhea, Tinnitus, Headache, Nausea | Swimming pool and sauna usage, Diabetes, Immunosuppressive therapy, Long-term antibiotic treatment | Dorko, E. et al. [40] |
| Spain (390 patients) |
C. parapsilosis, A. flavus, C. albicans, A. niger, A. fumigatus, A. candidus, A. terreus, C. glabrata, C. tropicalis, Paecilomyces variotii |
Pruritus, Otalgia, Hearing loss | N/A | García-Agudo, L. et al. [41] |
| Russia (331 patients) |
A. niger, A. flavus, A. fumigatus, Candida spp. | N/A | N/A | Kryukov, A.I. et al. [21] |
| Serbia (292 patients) |
A. niger, C. albicans, C. parapsilosis, A. flavus, A. fumigatus, C. krusei, C. guilliermondii, C. glabrata, C. tropicalis |
N/A | N/A | Tasić-Otašević, S. et al. [4] |
| Serbia (30 patients) |
A. niger, A. flavus | N/A | Use of antibiotic ear drops, Use of EAC hygiene pro-ducts, Headphone usage, Frequent ORL examinations and rinsing of EAC, Corticosteroid ear drop usage, Predisposing diseases | Bojanović, M. et al. [10] |
* Number of patients diagnosed with otomycosis, ** Sorted by number of isolates, *** Sorted by frequency of occurrence, N/A Not Available.
The age and gender distribution of patients with otomycosis exhibits inconsistent findings across various reports. Some studies have stated that men are more frequently affected than women [4][37], but this is not uniform in all surveys [1][38]. Similarly, the fact that people between the ages of 25 and 45 are most often affected [1][29][30][37] is accompanied by findings that the prevalence of the disease increases with ageing [4].
Risk factors for EAC fungal infection include factors that damage the mechanical barrier of the EAC skin. In this group, frequent use of headphones [10], using hard objects to scratch the ear [33][34], and injuries to the skin [37] are dominant factors. Besides damage to the skin as a mechanical barrier, factors that disturb the EAC skin microbiota and affect the reduction of cerumen [37][42] can also impair non-specific resistance. Overuse of chemicals such as soaps, shampoos, boric acid, povidone–iodine, hydrogen peroxide, and other antiseptics, as well as excessive use of antibacterial ear drops, can disrupt the balance of the microbiota in the EAC. This disruption often leads to a reduction in the number of bacteria, which in turn can result in the overgrowth of fungi and increased risk of fungal infections [2][10][33]. Additionally, the use of coconut oil [34] and mustard oil [2] as an alternate treatment or for alleviating symptoms and signs of infection has been identified as a possible risk factor for otomycosis. Furthermore, clothing habits such as wearing head coverings, e.g., a turban or veil [6][36], have been highlighted as risk factors in areas where traditional clothing is common or recommended. Frequent swimming, recreationally or professionally, as well as the use of saunas and other spa treatments, can also predispose a person to this infection.
Lastly, preexisting diseases and conditions such as diabetes [1][38], immunosuppressive therapy [40], prolonged systemic antibiotic treatment [40], a history of otologic procedures [38], retroviral infection [1], sinonasal and nasopharyngeal malignancy [1], and mastoid cavity after surgical procedures [38] may predispose a person to the development of this infection. In premature newborns, intubation, artificial ventilation, and respiratory distress have also been identified as significant risk factors for fungal infection of the EAC [40].
This entry is adapted from the peer-reviewed paper 10.3390/jof9060662
References
- Fasunla, J.; Ibekwe, T.; Onakoya, P. Otomycosis in western Nigeria. Mycoses 2008, 51, 67–70.
- Agarwal, P.; Devi, L.S. Otomycosis in a Rural Community Attending a Tertiary Care Hospital: Assessment of Risk Factors and Identification of Fungal and Bacterial Agents. J. Clin. Diagn. Res. 2017, 11, Dc14–Dc18.
- Mofatteh, M.R.; Naseripour Yazdi, Z.; Yousefi, M.; Namaei, M.H. Comparison of the recovery rate of otomycosis using betadine and clotrimazole topical treatment. Braz. J. Otorhinolaryngol. 2018, 84, 404–409.
- Tasić-Otašević, S.; Golubović, M.; Đenić, S.; Ignjatović, A.; Stalević, M.; Momčilović, S.; Bojanović, M.; Arsić-Arsenijević, V. Species distribution patterns and epidemiological characteristics of otomycosis in Southeastern Serbia. J. De Mycol. Médicale 2020, 30, 101011.
- Kamali Sarvestani, H.; Seifi, A.; Falahatinejad, M.; Mahmoudi, S. Black aspergilli as causes of otomycosis in the era of molecular diagnostics, a mini-review. J. Mycol. Med. 2022, 32, 101240.
- Aneja, K.R.; Sharma, C.; Joshi, R. Fungal infection of the ear: A common problem in the north eastern part of Haryana. Int. J. Pediatr. Otorhinolaryngol. 2010, 74, 604–607.
- Buonafina-Paz, M.D.; Santos, F.A.; Leite-Andrade, M.C.; Alves, A.I.; Bezerra, J.D.; Leal, M.C.; Robert, E.; Pape, P.L.; Lima-Neto, R.G.; Neves, R.P. Otomycosis caused by the cryptic and emerging species Aspergillus sydowii: Two case reports. Future Microbiol. 2022, 17, 1437–1443.
- Değerli, K.; Ecemiş, T.; Günhan, K.; Başkesen, T.; Kal, E. Agents of otomycosis in Manisa region, Turkey, 1995–2011. Mikrobiyol. Bul. 2012, 46, 79–84.
- Abastabar, M.; Haghani, I.; Ahangarkani, F.; Rezai, M.S.; Taghizadeh Armaki, M.; Roodgari, S.; Kiakojuri, K.; Al-Hatmi, A.M.S.; Meis, J.F.; Badali, H. Candida auris otomycosis in Iran and review of recent literature. Mycoses 2019, 62, 101–105.
- Bojanović, M.; Ignjatović, A.; Stalević, M.; Arsić-Arsenijević, V.; Ranđelović, M.; Gerginić, V.; Stojanović-Radić, Z.; Stojković, O.; Živković-Marinkov, E.; Otašević, S. Clinical Presentations, Cluster Analysis and Laboratory-Based Investigation of Aspergillus Otomycosis-A Single Center Experience. J. Fungi 2022, 8, 315.
- Chappe, M.; Vrignaud, S.; de Gentile, L.; Legrand, G.; Lagarce, F.; Le Govic, Y. Successful treatment of a recurrent Aspergillus niger otomycosis with local application of voriconazole. J. Mycol. Med. 2018, 28, 396–398.
- Munguia, R.; Daniel, S.J. Ototopical antifungals and otomycosis: A review. Int. J. Pediatr. Otorhinolaryngol. 2008, 72, 453–459.
- Lee, A.; Tysome, J.R.; Saeed, S.R. Topical azole treatments for otomycosis. Cochrane Database Syst. Rev. 2021, 5, Cd009289.
- Sander, R. Otitis externa: A practical guide to treatment and prevention. Am. Fam. Physician 2001, 63, 927–936, 941–922.
- Chavan, R.P.; Ingole, S.M.; Kanchewad Resident, G.S. Single Topical Application of 1% Clotrimazole Cream in Otomycosis. Indian J. Otolaryngol. Head Neck Surg. 2023, 75, 147–154.
- Vennewald, I.; Klemm, E. Otomycosis: Diagnosis and treatment. Clin. Dermatol. 2010, 28, 202–211.
- Antunes, J.; Mendes, N.; Adónis, C.; Freire, F. Treatment of otomycosis with clotrimazole: Results accordingly with the fungus isolated. Acta Otolaryngol. 2022, 142, 664–667.
- Gülüstan, F.; Abakay, M.A.; Demir, E. Efficacy of topical isoconazole nitrate in the treatment of otomycosis. Am. J. Otolaryngol. 2021, 42, 102961.
- Hagiwara, S.; Tamura, T.; Satoh, K.; Kamewada, H.; Nakano, M.; Shinden, S.; Yamaguchi, H.; Makimura, K. The Molecular Identification and Antifungal Susceptibilities of Aspergillus Species Causing Otomycosis in Tochigi, Japan. Mycopathologia 2019, 184, 13–21.
- Nemati, S.; Gerami, H.; Faghih Habibi, A.; Kazemnejad, E.; Shabani, N.; Aghsaghloo, V.; Montazeri, S. Sertaconazole versus Clotrimazole and Miconazole Creams in the Treatment of Otomycosis: A Placebo-Controlled Clinical Trial. Iran. J. Otorhinolaryngol. 2022, 34, 27–34.
- Kryukov, A.I.; Kunelskaya, N.L.; Kunel’skaya, V.Y.; Ivoilov, A.Y.; Turovskiy, A.B.; Shadrin, G.B.; Machulin, A.I. Otomycosis: The modern view of etiology and management. Vestn. Otorinolaringol. 2018, 83, 48–51.
- Yang, T.H.; Young, Y.H. Eradicating Otomycosis with Terbinafine Solution: Basic and Clinical Investigation. Audiol. Neurotol. 2019, 24, 183–190.
- Herasym, K.; Bonaparte, J.P.; Kilty, S. A comparison of Locacorten-Vioform and clotrimazole in otomycosis: A systematic review and one-way meta-analysis. Laryngoscope 2016, 126, 1411–1419.
- Koltsidopoulos, P.; Skoulakis, C. Otomycosis With Tympanic Membrane Perforation: A Review of the Literature. Ear Nose Throat J. 2020, 99, 518–521.
- Anwar, K.; Gohar, M.S. Otomycosis; clinical features, predisposing factors and treatment implications. Pak. J. Med. Sci. 2014, 30, 564–567.
- Hoenigl, M.; Salmanton-García, J.; Walsh, T.J.; Nucci, M.; Neoh, C.F.; Jenks, J.D.; Lackner, M.; Sprute, R.; Al-Hatmi, A.M.S.; Bassetti, M.; et al. Global guideline for the diagnosis and management of rare mould infections: An initiative of the European Confederation of Medical Mycology in cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect. Dis. 2021, 21, e246–e257.
- Kazemi, A.; Majidinia, M.; Jaafari, A.; Ayatollahi Mousavi, S.A.; Zarei Mahmoudabadi, A.; Alikhah, H. Etiologic Agents of Otomycosis in the North-Western Area of Iran. Jundishapur. J. Microbiol. 2015, 8, e21776.
- Jia, X.; Liang, Q.; Chi, F.; Cao, W. Otomycosis in Shanghai: Aetiology, clinical features and therapy. Mycoses 2012, 55, 404–409.
- Ali, K.; Hamed, M.A.; Hassan, H.; Esmail, A.; Sheneef, A. Identification of Fungal Pathogens in Otomycosis and Their Drug Sensitivity: Our Experience. Int. Arch. Otorhinolaryngol. 2018, 22, 400–403.
- Alarid-Coronel, J.; Celis-Aguilar, E.; Escobar-Aispuro, L.; Muñoz-Estrada, V. Otomycosis in immunocompetent patients: Clinical and mycological features. Our experience with 40 cases. Clin. Otolaryngol. 2018, 43, 373–377.
- Pontes, Z.B.; Silva, A.D.; Lima Ede, O.; Guerra Mde, H.; Oliveira, N.M.; Carvalho Mde, F.; Guerra, F.S. Otomycosis: A retrospective study. Braz. J. Otorhinolaryngol. 2009, 75, 367–370.
- Panigrahi, M.; Paty, B.P.; Parida, B.; Padhi, S.; Kumari Sahu, S.; Narasimham, M.V.; Mohanty, I. Clinicomycological Study of Otomycosis with Antifungal Susceptibility Testing Of Fungal Isolates. IOSR-JDMS 2019, 18, 7–12.
- Rawat, S.; Saxena, N.; Chad, A.; Garg, N.; Sharma, K. Cinicomycological study of otomycosis with antifungal drug susceptibility testing of Candida isolates using disk diffusion method in Kota region, Rajasthan. Int. J. Curr. Microbiol. App. Sci. 2017, 6, 3356–3366.
- Prasad, S.C.; Kotigadde, S.; Shekhar, M.; Thada, N.D.; Prabhu, P.; D’ Souza, T.; Prasad, K.C. Primary otomycosis in the Indian subcontinent: Predisposing factors, microbiology, and classification. Int. J. Microbiol. 2014, 2014, 636493.
- Ismail, M.T.; Al-Kafri, A.; Ismail, M. Otomycosis in Damascus, Syria: Etiology and clinical features. Curr. Med. Mycol. 2017, 3, 27–30.
- Ozcan, K.M.; Ozcan, M.; Karaarslan, A.; Karaarslan, F. Otomycosis in Turkey: Predisposing factors, aetiology and therapy. J. Laryngol. Otol. 2003, 117, 39–42.
- Abdelazeem, M.; Gamea, A.; Mubarak, H.; Elzawawy, N. Epidemiology, causative agents, and risk factors affecting human otomycosis infections. Turk. J. Med. Sci. 2015, 45, 820–826.
- Ho, T.; Vrabec, J.T.; Yoo, D.; Coker, N.J. Otomycosis: Clinical features and treatment implications. Otolaryngol. Head Neck Surg. 2006, 135, 787–791.
- Kurnatowski, P.; Filipiak, A. Otomycosis: Prevalence, clinical symptoms, therapeutic procedure. Mycoses 2001, 44, 472–479.
- Dorko, E.; Jenca, A.; Orencák, M.; Virágová, S.; Pilipcinec, E. Otomycoses of candidal origin in eastern Slovakia. Folia Microbiol. 2004, 49, 601–604.
- García-Agudo, L.; Aznar-Marín, P.; Galán-Sánchez, F.; García-Martos, P.; Marín-Casanova, P.; Rodríguez-Iglesias, M. Otomycosis due to filamentous fungi. Mycopathologia 2011, 172, 307–310.
- Lum, C.L.; Jeyanthi, S.; Prepageran, N.; Vadivelu, J.; Raman, R. Antibacterial and antifungal properties of human cerumen. J. Laryngol. Otol. 2009, 123, 375–378.
This entry is offline, you can click here to edit this entry!
