Sleep disturbances refer to a group of disturbances described as trouble falling/staying asleep, which can cause excessive drowsiness during the daytime as a result of an inadequate amount of sleep, or change in sleep quantity, quality, or timing [
23,
24,
25]. However, the sleep disturbances that were focused on in the majority of the studies were poor sleep quality and insomnia. Sleep quality that was poor in nature was assessed using the Pittsburgh sleep quality index (PSQI), and insomnia was assessed using the insomnia severity index (ISI) and the Athens insomnia scale (AIS). Many other measures were also used to report sleep disturbances. The BEARS questionnaire described bedtime problems, increased daytime sleepiness, awakening throughout the night, regularity and duration of sleep, and finally snoring. Adequate sleep, somnolence, amount of sleep obtained, snoring, and waking up with shortness of breath or with a headache were reported using the medical outcomes study sleep scale (MOS-SS). Patient’s own perceptions of sleep quality, the depth of their sleep, and restoration associated with sleep were assessed by the patient-reported outcomes measurement information system-sleep disturbance (PROMIS) questionnaire. In children, the Sleep Disturbance Scale for Children (SDSC) and the youth self-rating insomnia scale were valuable tools to measure these sleep changes [
18].
Sleep’s vital role in everyday life is well known [
23]. Sleep dysfunction has been linked to deleterious effects on mood, health, and various motor vehicle accidents [
24]. Self-reported data from various sections of society indicate high amounts of the burden of this dysfunction during the COVID-19 pandemic [
25]. The prevalence of sleep changes during the COVID-19 pandemic was estimated to be about 36% [
8,
25], with higher impact on patients infected with the COVID-19 virus [
8,
25,
26,
27,
28]. However, these numbers are variable based on several factors, as discussed below.
Studies by Ara et al. [
30], Wang et al. [
31], Czeisler et al. [
32] and Kim et al. [
33] reported that sleep disturbances are either more likely among patients more than 30 years of age or increase with age. On the contrary, studies by Beck et al. [
34], Romero-Blanco et al. [
35], Mareli et al. [
36], and Kaparounaki et al. [
37] indicate a higher prevalence of sleep disturbances among younger ages (18–34 years). It can be argued that even though sleep structure and circadian rhythm alter with age, the variability in stress related to financial, social, and emotional burdens heavily impacts various age groups differently [
17]. Moreover, as the above factors change with geographical location, cultural backgrounds and other comorbidities, inconsistency in results is expected [
17,
18].
The impact of the COVID-19 pandemic has affected sleep in various ways through cytokine release, neuro-inflammation, and other ways discussed later in this review. The psycho-sociological effects of social distancing, isolation, and quarantine measures manifested as loneliness, detachment, boredom, and loss of freedom [
7,
13,
14,
15,
16,
17]. This diminished coping mechanisms, which likely contributed to new mental health issues. As we already know, any amount of mental health concerns is an obvious link to sleep disturbances and vice-versa [
7,
13,
14,
15,
16,
17]. The increased morbidity and mortality in society further aggravated stress and led to sleep disorders.
5. Various Sleep Disorders Associated with COVID-19 Infection
Prior epidemics and pandemics have exposed the world population to stress, social confinement, limited daylight exposure, step back from normalcy, and induced sleep disturbances, which during the coronavirus period was termed the coronasomnia phenomenon. These sleep disturbances include insufficient sleep, insomnia, poor sleep quality, sleep apnea, and circadian rhythm disorders [
86]. Confinement from quarantine measures played a vital role in causing insomnia, as evidenced by studies in Europe [
6]. In Italy, anxiety from COVID-19 was associated with sleep problems [
41,
42,
87]. REM sleep disorders could be directly linked to the COVID-19 infection itself [
88].
The prevalence of insomnia was as high as 60% among COVID-19 survivors, although variable rates were noted in China (2%) [
89], Italy (40%) [
90], and Mexico (77%) [
90,
91]. These results are attributable to the neuroinflammatory changes or the stress around the pandemic. These results may be related to the duration of illness, as explained by Pedrozo-Pop et al., where insomnia was more likely in patients who experienced illness for more than 3 weeks. Moreover, insomnia was associated with increased post-traumatic stress disorder (PTSD) risk as encountered in clinical practice [
89,
92,
93].
Obstructive sleep apnea (OSA) was present in 8–21% of patients hospitalized with COVID-19 infection [
46,
94,
95,
96,
97,
98]. The results of the association between the two have been contradictory. However, the majority of studies suggest OSA as a risk factor for a complicated hospital course. The underlying inflammatory state of COVID provides a plausible explanation for this association. The hypoxemic state in OSA affects the cytokine storm, further worsening it [
89]. Hence, owing to its antioxidant, anti-inflammatory, and pro-immunity actions, melatonin can be used in the treatment of COVID-19 pneumonia, especially in OSA patients [
99,
100]. Various studies thus indicate the relationship between COVID and OSA as bidirectional and synergistic [
46,
101,
102]. However, minimal literature is available confirming this relationship and the prevalence of other sleep disorders during the COVID pandemic.
6. Poor Sleep and COVID-19
Sleep is a known factor that impacts the immune response, and evidence suggests that sleep disturbances alter the immunity to feasibly cause immunosuppression [
103,
104]. This may be from the changes in cytokine production, release, and associated cell count variability. Similarly, as studied by previous research, the COVID-19 virus alters sleep quality in hospitalized patients. However, the effect from the direct impact of the virus is ambiguous. It is hypothesized to be a result of anxiety, pain, physical discomfort, prolonged hospitalization, or polypharmacy [
105,
106]. Several studies indicate the link between poor sleep quality and slow improvement of lymphopenia in hospitalized patients and further need for ICU admissions, indicating the association between the two [
107]. Research indicates that reduced sleep duration and coexisting comorbidities are significant indicators of disease severity. Hence, while studying the impact of COVID-19 on sleep, it should be borne in mind that sleep affects COVID-19 severity, alters the clinical course of events, and impacts the clinical outcomes of COVID-19. Outpatient and hospitalized patients suffering from this infection should be notified about the importance of sleep in the recovery from infection [
108]. A particular study showed poor sleep and high-stress levels in hospitalized schizophrenic patients suspected of developing a COVID-19 infection. This indicates that treating sleep problems is imperative for recovering from mental illnesses and possibly strengthening immunity to prevent infections [
109].
Sleep manifestations such as insomnia can impose prolonged problems. Insomnia can become chronic, worsen pain syndromes and gastrointestinal disorders, and increase the risk of hypertension and heart diseases if left untreated [
28]. Recent evidence suggests that sleep loss is a potential biomarker of blood–brain barrier (BBB) leak. Possible mechanisms implicated in this process are neuroinflammation from causing loss of BBB integrity [
110] and possibly inducing infection or other mental illnesses. Sleep stands as an often-ignored entity during the other deleterious impact of COVID-19 infection. However, it remains a silent component that can cause long-term effects, making early management vital to prevent such an outcome.
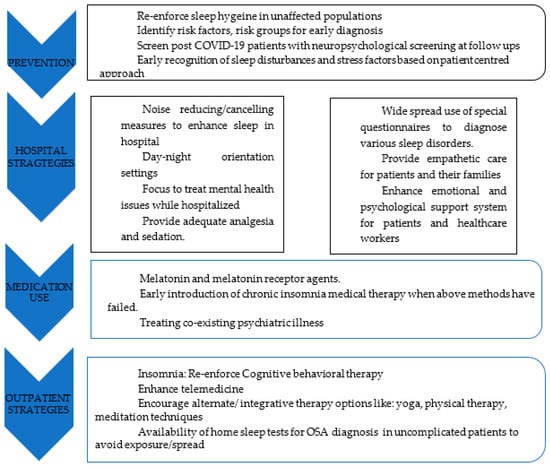
7. Management Modalities
Sleep is affected by and, in turn, also affects health and mood. Hence, it is imperative to recognize and address sleep disturbances in various population groups during the early phase of impact. This starts with identifying individual, interpersonal, professional, and community risk factors [
111]. Basic principles of sleep hygiene should be reinforced. As COVID-19 infection has been correlated to sleep disturbances, mental health problems, and stress in general, special focus on this subset of patients is much needed to reduce the burden of the already disastrous disease impact and improve prognosis [
16,
99,
106]. Often, hospitalization causes delirium and can disturb the sleep cycle. Hence, delirium management strategies such as frequent re-orientation, maintaining the sleep–wake cycle through adequate light settings, adequate pain control, and through use of circadian rhythm-maintaining medications such as melatonin [
99,
100]. The effects of ICU stay and associated trauma from mechanical ventilation can induce PTSD and aggravate sleep problems [
89,
90,
91,
92,
93]. The use of prophylactic melatonin and melatonin receptor agonists such as Ramelteon for sleep–wake cycle disorders improved the sleep of ICU patients, decreasing the delirium occurrence and duration of ICU stay [
100]. Other sleep dysfunction treatment modalities have been discussed below (
Figure 1).
Figure 1. Treatment modalities for pandemic related sleep dysfunction.
8. Novel vs. Existing Therapeutics
This work has important biomedical applications, as it provides a review on the literature surrounding actions providers can take in treating sleep disturbances. Some of these examples, as previously mentioned, include good sleep hygiene, strategies of minimizing delirium in the inpatient setting, and utilizing melatonin agonists when indicated. Other nonpharmacologic treatments classically discussed in the sleep literature include sleep diaries, sleep restriction, and other cognitive and relaxing techniques (122). Other pharmacologic therapies include benzodiazepines, non-benzodiazepine hypnotics, antihistamines, and antidepressants (122). Comparatively, our therapies discussed offer many benefits, including ease of administration (i.e., minimizing delirium via maintaining schedules, opening window blinds) and accessibility to patients (i.e., sleep hygiene is a factor patients can directly address themself). More research needs to be conducted regarding use of these alternate therapies in sleep disturbances.