Spinal cord injury (SCI) is a profoundly debilitating yet common central nervous system condition resulting in significant morbidity and mortality rates. Major causes of SCI encompass traumatic incidences such as motor vehicle accidents, falls, and sports injuries. Treatment strategies for SCI aim to improve and enhance neurologic functionality. The ability for neural stem cells (NSCs) to differentiate into diverse neural and glial cell precursors has stimulated the investigation of stem cell scaffolds as potential therapeutics for SCI. Various scaffolding modalities including composite materials, natural polymers, synthetic polymers, and hydrogels have been explored.
1. Introduction
Spinal cord injury (SCI) is an incredibly devastating central nervous system condition resulting in significant morbidity and mortality rates worldwide. Recent estimates of traumatic SCI include about 26.5 cases per 1,000,000 citizens with greater predominance in males [
1,
2]. Approximately 50% of SCIs are cervical and result in greater mortality rates, especially in older adults [
1]. Common causes of SCI in the United States include motor vehicle accidents, sports injuries, and traumatic falls [
2]. SCI pathogenesis is hypothesized to occur in two stages—primary and secondary [
3]. Primary SCI refers to the initial mechanical injury while secondary SCI involves acute and chronic cascades of increased immune activation, neuroinflammation, and excitotoxicity [
3,
4]. Specific mechanisms of secondary SCI include lipid peroxidation, axon degeneration and demyelination, increased calcium influx, free radical formation, and pathological remodeling of the surrounding extracellular matrix [
3]. Secondary SCI is presumed to predict and influence overall SCI severity, highlighting its potential role as a target for intervention [
4]. However, continued efforts are needed to characterize the role of inflammation in SCI and whether certain cell types and molecules are beneficial or detrimental to recovery [
4].
Neural regeneration following axonal injury is a complex process involving multiple proteins, signaling molecules, and genes [
5]. Axonal regeneration begins with rapid sealing of the plasma membrane, followed by axonal growth cone formation and stabilization [
6,
7]. Regrowth is further mediated by several neurotrophic factors such as brain-derived neurotrophic factor (BDNF), neurotrophin-3 (NT3), and nerve growth factor (NGF), all of which act on tyrosine kinase receptors [
8]. Intraoperative electrical stimulation (ES) additionally has the ability to promote axonal regrowth, though the biological mechanisms remain relatively unknown.
Despite the fact that neurons in the central nervous system regenerate poorly in response to trauma, a major goal in the treatment of SCI is restoration of neurologic functioning. The current standard of care treatment for acute SCI includes pharmacologic agents such as paracetamol, weak opioids, or non-steroidal anti-inflammatory drugs [
9]. In some cases, surgical intervention such as a spinal decompression may be necessary [
9]. However, there are contradictory findings in the literature regarding the effects of surgical timing on SCI outcomes. A meta-analysis by Hsieh et al. demonstrated that early decompression within 8–12 h of SCI was associated with improvement of at least one AIS grade, regardless of spinal location or completeness of injury [
10]. Similarly, another study involving 1548 patients showed that surgery within 24 h was associated with improved recovery [
11]. However, findings by Aarabi et al. revealed the timing of surgery does not influence 6 month post-injury AIS conversion in cervical SCI patients [
12]. As such, clinical management of SCI differs with respect to individual patient differences and medical center protocols.
To improve patient outcomes in a highly individualized manner, novel treatment strategies for SCI involving use of stem cell scaffolds have been explored [
9]. Stem cell scaffolding involves the creation of a three-dimensional structure designed to imitate the extracellular matrix surrounding cells in the spinal cord [
13,
14]. By providing stem cells with a highly biocompatible environment suitable for stem cell differentiation, adhesion, and proliferation, stem cell scaffolds can theoretically be used to treat SCI [
15]. A variety of scaffolding modalities have been explored including hydrogels, natural polymers, synthetic polymers, and composites [
14,
16].
2. NSC Differentiation
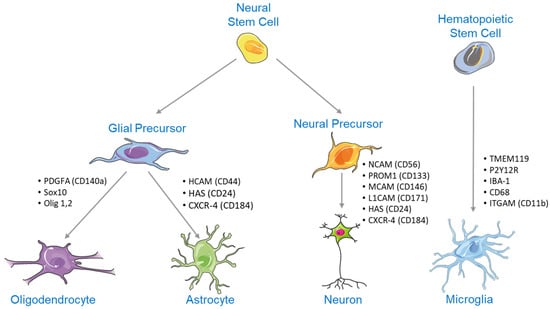
NSC differentiation begins when NSCs differentiate into neural or glial progenitor cells. Neural progenitors can then differentiate into a wide range of mature neurons, while glial progenitor cells ultimately differentiate into oligodendrocytes and astrocytes (
Figure 1) [
17,
18]. Contrastingly, microglia are of hematopoietic origin [
19]. Surface markers are seen at each stage of differentiation, and as such, can be used to determine neural cell differentiation progress [
20].
Figure 1. NSCs can differentiate into glial or neural precursors. Neural precursors develop into a wide range of mature neurons, while glial precursors form either oligodendrocytes or astrocytes. Note: This figure contains (modified) images from Servier Medical Art (
https://smart.servier.com, accessed on 13 July 2023).
NSC differentiation is regulated by a variety of signaling pathways and transcription factors that influence both embryological development and adult neural neogenesis [
21]. Specific signaling pathways highly implicated in NSC differentiation include the Notch, Wnt/β-catenin, sonic hedgehog (Shh), and bone morphogenetic protein (BMP) signaling pathways [
21].
3. Substrates Indicated for Axonal Regrowth Post-Injury
Three-dimensional (3D) axonal regrowth is a complex process that occurs after an injury involving multiple genes, signaling molecules, proteins, and extracellular environment components [
5]. For axonal regrowth to occur, the primary neural cell body must physically disconnect from its distal target [
55]. When this occurs, the remaining portion of the axon connected proximally to the neural cell body will undergo a regenerative phase, which entails the creation of the axonal growth cone. This growth cone can be described as a mobile structure that uses various growth factors and signaling molecules in the surrounding environment to guide and elongate the axon [
5].
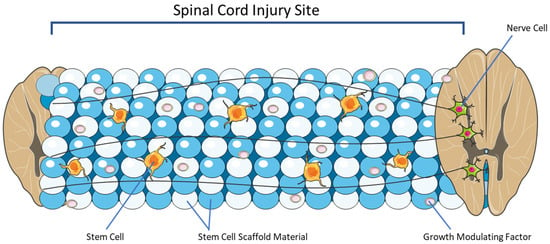
4. Overview of Stem Cell Scaffolding
The stem cell scaffold is a lab-created, three-dimensional structure designed to imitate and modulate many of the key characteristics of the naturally occurring ECM (
Figure 2) [
13,
14]. The scaffold is meant to provide an environment for stem cell differentiation, attachment, and growth [
15]. There are several broad categories of scaffolds including hydrogels, natural polymers, synthetic polymers, and composites [
14,
16]. A key feature of stem cell scaffolds is their ability to be modified for specific applications [
91]. Routes of modification that will be reviewed here include the incorporation of growth-modulating molecules, surface adhesion molecules, and electrical stimulation.
Figure 2. Stem cell scaffolds are meant to provide physical support for recovery post-SPI. They provide a matrix for growth factor release, stem cell implantation, and axonal rejuvenation. Note: This figure contains (modified) images from Servier Medical Art (
https://smart.servier.com, accessed on 13 July 2023).
One of the key purposes of a scaffold is to provide a mechanical support network for stem cells to reside within. This framework protects growing cells and axons from applied forces post-SCI [
92,
93]. The porosity or the percentage of pores per area of scaffold is a vital feature. It defines the surface area for cell attachment within the scaffold environment [
94]. Higher porosity precents have been associated with increased stem cell growth and differentiation [
95,
96]. While to our knowledge, no study has examined the ideal scaffold pore diameter for SCI repair, it is notable that spinal corticospinal tract axons are believed to range from 1 to 22 μm in diameter, with the majority of axons falling in a range of 1–4 μm. This implies that while scaffold pore diameters as low as 4 μm are large enough for the passage of most axons, the lower end of the pore diameter limit must be no less than 22 μm to accommodate all corticospinal tract axons. In addition, even more space may be required for the ideal passage of waste, nutrients, and other important axons with larger diameters such as pyramidal tract axons, purkinje cell axons, Aα sensory fibers, and Aβ sensory fibers. Conversely, increasing porosity and pore diameter has the negative effect of reducing compressive strength and elastic modulus [
97,
98,
99]. Another crucial property of a scaffold is biodegradability with minimal cytotoxic byproducts [
100]. Biodegradability allows the scaffold to be fully absorbed with time and replaced by ECM. This reduces lasting inflammation, permits further axonal and cell proliferation, and allows for the release of infused growth-modulating factors [
14,
100].
5. Emerging Pre-Clinical Studies and Their Applications for Clinical Adoption
Given the significant therapeutic potential of scaffolding for SCI, a variety of preclinical studies have investigated a diverse range of scaffolding constructs for their therapeutic potential in the treatment of SCI. Collagen is the most abundant protein in mammals primarily used to synthesize connective tissues such as skin, bone, muscles, tendons, and cartilage. Its high biocompatibility, hydrophilic nature, abundance in somatic tissues, and high degree of cellular adhesion allows it to be synthesized into scaffolds [
106]. Consequently, collagen-derived stem cell scaffolds for SCI have been studied extensively throughout the literature (
Table 1) [
128,
129,
130,
131,
132,
133,
134,
135]. Specifically, collagen-based stem cell scaffolds recruit and protect embryonic neural stem progenitor cells (NSPCs) at SCI lesions, promote neural stem cell (NSC) adhesion, proliferation, and differentiation, and improve locomotor behaviors in murine models [
128,
129]. When seeded with NSPCs, the efficacy of collagen scaffolding for SCI is enhanced through improved axonal elongation, neural regeneration at SCI lesions, enhanced NSPC differentiation, and functional integration of the regenerated cells into the preexisting neural network [
129]. This strategy has been shown to improve hindlimb motor function, nerve regeneration, and neural cell extension in rat models of complete spinal cord transection [
131].
Table 1. Summary of emerging pre-clinical studies utilizing collagen-based stem cell scaffolds for the treatment of SCI.
Collagen scaffolds for SCI can be further modified through the addition of patient-specific bone marrow mononuclear cells or mesenchymal stem cells (MSCs) [
130,
134]. In murine and canine models of complete spinal cord transection, administration of collagen scaffolds seeded with MSCs derived from neonatal umbilical cord tissue resulted in increased motor scores and reduced injury area [
130]. Consequently, a phase I clinical trial (NCT 02510365) was conducted by Deng et al. [
130] to investigate the efficacy of this scaffold in 40 patients with acute complete cervical injuries. Twelve months after transplantation of the human umbilical cord MSC collagen scaffold at the site of SCI, novel nerve fiber growth emerged and electrophysiological activity of the adjacent neurons improved [
130]. Increased daily life scores, American Spinal Injury Association scores, and bowel and urinary functioning were additionally observed [
130]. The results of this clinical trial are significant because there are few reports in the literature detailing results from humans subjects involved in clinical trials investigating the role of stem cell scaffolds as a treatment option for SCI. Furthermore, a later study by Tang et al. [
117] investigating the longitudinal effects (2–5 years) of collagen scaffolds loaded with patient-specific bone marrow mononuclear cells or human umbilical cord MSCs for SCI demonstrated similar results with improvements in bowel and bladder sensation, voluntary walking ability, and enhanced finger activity [
130,
134].
The addition of proteins expressed in MSCs can enhance the efficacy of collagen scaffolds for SCI [
128]. One study by Liu et al. [
128] investigating the effects of a linearly ordered collagen scaffold modified with N-cadherin, a protein expressed in mesenchymal cells, found that adhesion of NSPCs onto the collagen scaffold improved with the introduction of N-cadherin. When transplanted into rats with complete spinal cord transections, the N-cadherin-modified collagen scaffold recruited more NSPCs to the lesion site and consequently, LOCS-Ncad rats demonstrated significantly improved locomotor function as compared to controls [
128]. Similarly, collagen scaffolds seeded with MSCs can be further enhanced by the addition of silk fibroin or heparan sulfate [
132,
133,
135]. Silk fibroin is a natural fibrous protein found in silk and spider webs. Like collagen, silk fibroin demonstrates high biocompatibility and mechanical strength allowing for its use in adipose tissue, bone, and skin regeneration [
136]. When compared to collagen/silk scaffolds lacking MSC seeds, collagen/silk scaffolds seeded with MSCs can facilitate nerve fiber regeneration, enhance remyelination, and accelerate the establishment of synaptic connections at the injury site [
135]. As such, human umbilical cord MSCs embedded on collagen/silk fibroin scaffolds have been shown to induce functional recovery and improve locomotor behaviors in rats with complete SCIs [
133,
135]. Similarly, heparan sulfate is a polysaccharide involved in a number of biological processes including cell proliferation, inflammation, and angiogenesis [
137]. Collagen scaffolds enhanced with heparan sulfate and MSCs demonstrate significant improvements in locomotor activity, motor evoked potential, urodynamic parameters, and modulation of inflammatory cytokines in canines with complete spinal cord transections [
132].
In addition to collagen, stem cell scaffolds constructed with hydrogel have been explored as a therapeutic for SCI (
Table 2) [
138,
139,
140,
141,
142,
143]. Matrigel, a solubilized basement membrane protein composed of laminin, collagen IV, heparan sulfate proteoglycans, entactin/nidogen, and growth factors, can be employed for treatment of SCI [
144]. Matrigel has been shown to support neural stem cell survival in vitro and in vivo [
144]. When implanted into a murine model of SCI, administration of Matrigel shows slight functional repair and neural recovery, though nonsignificant [
144]. Hyaluronic acid hydrogel dotted with manganese dioxide nanoparticles has the ability to bridge nerve tissue and enhance adhesive growth of MSCs [
142]. When implanted into rats with SCIs, MSC differentiation is enhanced and motor function is significantly restored [
142]. NSCs obtained from epileptic human brain specimens seeded in PuraMatrix peptide hydrogel enhance cell survival and differentiation, reduce SCI lesion volume, and improve neurological functioning in rats with SCIs [
140]. Hydrogel enhanced with agarose, gelatin, and polypyrrole additionally improves NSPC differentiation, reduces SCI lesion volume, and provides a biocompatible microenvironment suited for tissue repair in vivo [
143]. Similarly, gelatin methacryloyl (GelMA) hydrogel constructed with decellularized spinal cord extracellular matrix-gel (DSCG) provides a robust microenvironment in vitro favoring menstrual blood-derived mesenchymal stem cells (MenSCs) adhesion, proliferation, and differentiation [
138]. DSCG/GelMA scaffolded with MenSCs improved motor function, reduces neural inflammation, and promotes neural differentiation in rats with complete spinal cord transections [
138]. The same effects are seen in murine models of SCI utilizing grooved GelMA-MXene hydrogel loaded with NSCs [
139]. Because SCI creates a pathologically inflamed microenvironment characterized by immune activation damage-associated molecular patterns and activation of immune cells that impair neurologic recovery, more modern hydrogel scaffolds aim to restore the pathological SCI microenvironment [
141]. For example, hydrogel scaffolds constructed to release interleukin-10, an anti-inflammatory cytokine, have the ability to enhance NSC differentiation, neural regeneration, and axonal growth in mice with SCIs [
141].
Table 2. Summary of emerging pre-clinical studies utilizing hydrogel-based stem cell scaffolds for the treatment of SCI.
|
Source
|
Subject
|
Stem Cell Type
|
Scaffold Material
|
Outcome
|
|
Wang et al. [144]
|
Sprague-Dawley rats
|
NSCs
|
Matrigel
|
Slight neural recovery and improved motor function
|
|
Li et al. [142]
|
Sprague-Dawley rats
|
MSCs
|
Hyaluronic acid hydrogel with manganese dioxide nanoparticles
|
Enhanced MSC growth and differentiation, restoration of locomotor function
|
|
Abdolahi et al. [140]
|
Sprague-Dawley rats
|
NSCs
|
PuraMatrix peptide hydrogel
|
Enhance NSC survival and differentiation, reduced SCI lesion volume, improved neurologic functioning
|
|
Yang et al. [143]
|
C57/BL6 mice
|
NSPCs
|
Hydrogel enhanced with agarose, gelatin, and polypyrrole
|
Enhanced NSPC differentiation, reduced SCI lesion volume
|
|
He et al. [138]
|
Sprague-Dawley rats
|
MenSCs
|
DSCG/GelMA hydrogel
|
Improved motor function, reduced inflammation, enhanced MenSC differentiation
|
|
Cai et al. [139]
|
Sprague-Dawley rats
|
NSCs
|
GelMA-MXene hydrogel
|
Improved motor function, reduced inflammation, enhanced NSC differentiation
|
|
Shen et al. [141]
|
C57/BL6 mice
|
NSCs
|
IL-10-enhanced hydrogel
|
Enhanced NSC differentiation, neural regeneration, and axonal regrowth
|
The development of 3D bioprinting technology has allowed for the refinement of stem cell scaffolds for SCI [
145]. Specifically, 3D bioprinting technology precisely enhances neural regeneration by creating biomimetic scaffolds tailored to the dimensions of the subject or patient in a time-sensitive manner [
146]. Bioprinting of a sodium alginate/gelatin scaffold loaded with NSPCs and oligodendrocytes demonstrates improved hindlimb motor function and nerve regeneration in a rodent model of SCI [
145]. Similarly, 3D bioprinted scaffolds loaded with induced pluripotent stem cells derived from urine cells have the ability to improve SCI in mice [
147]. The precision of 3D bioprinted scaffolds can additionally be enhanced with the addition of small molecules. By loading 3D bioprinted scaffolds with OSMI-4, a small molecule O-GlcNAc transferase inhibitor, differentiation of NSCs can be induced and specifically guided to the SCI lesion for more efficient SCI repair [
148]. Consequently, the OSMI-4-refined bioscaffold promoted neural regeneration and axonal growth, leading to significant motor recovery in rats with SCIs [
148]. As such, construction of stem cell scaffolds for SCI can be refined by means of 3D bioprinting.
This entry is adapted from the peer-reviewed paper 10.3390/biomechanics3030028