Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cell Biology
Protein aggregation is one of the hallmarks of aging and aging-related diseases, especially for the neurodegenerative diseases (NDs) such as Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), Amyotrophic lateral sclerosis (ALS), and others.
- natural products
- neurodegenerative diseases
- protein aggregation
- Aβ
1. Introduction
Neurodegenerative diseases (NDs) are a heterogeneous group of disorders characterized by abnormal protein aggregation leading to the structural and functional degeneration of the central and peripheral nervous systems [1]. These diseases cause a large number of deaths and enormous medical costs worldwide, placing a heavy burden on patients, their families and society. According to the Global Alzheimer’s Disease Report, there are already more than 55 million people with Alzheimer’s disease (AD) worldwide, and this number is expected to rise to 78 million by 2030 and 152 million by 2050 [2]. Parkinson’s disease (PD) is the second most common and fastest growing ND in the world, with a global prevalence of more than 6 million people and a 2.5-fold increase from the previous generation of patients, and is expected to double again to more than 12 million by 2040 [3]. There is growing evidence that men are twice as likely as women to develop Parkinson’s disease, but women have higher mortality rates and a more rapid disease progression, placing an enormous burden on the population [4]. Huntington’s disease (HD) cases are distributed worldwide, with a prevalence of 4–10 per 100,000 in Western countries and approximately 5 per million in Asian populations [5,6]. The incidence of amyotrophic lateral sclerosis varies from country to country and region to region, from about (2–3/100,000) in Europe to about (0.7–0.8/100,000) in Asia, with huge annual treatment costs [7]. The common symptoms of these diseases are memory and cognitive impairment, as well as difficulties with speech and movement, and they tend to be more common in older people [8].
In these diseases, one or more different pathologically aggregation-prone polypeptides misfold and are packaged into large insoluble inclusion bodies. For example, the two hallmark pathological the features of AD are extracellular amyloid plaques composed of Aβ peptides and intracellular neurofibrillary tangles composed of hyperphosphorylated microtubule-associated protein tau [9,10]. PD is a movement disorder characterized by the accumulation of Lewy bodies in neurons, which are mainly composed of 𝛼-synuclein protein aggregates [11,12]. Due to CAG repeat expansion in the huntingtin (HTT) gene, the mutant Htt protein accumulates in neurons and forms deposits that produce cytotoxicity, leading to the development of HD [13]. And one of the reasons why ALS occurs is because the abnormally aggregated FUS protein state is more solidified, impairing its normal physiological function [14]. These diseases not only hinder people’s normal physical activities and increase their psychological stress, but also place a huge burden on society. However, there are no symptomatic drugs for these diseases. Therefore, finding ways to make the diseases more treatable has become a priority.
Natural products are a class of compounds isolated from plants or fungi that are biologically active and have a rich history of medicinal use [15]. In recent years, the biological activity, nutritional value, and potential health and therapeutic benefits of natural products have been intensively explored and studied [16,17]. Due to their neuroprotective effects, a variety of compounds from different sources have been proposed to have therapeutic efficacy in treating neurodegenerative diseases, and not only in alleviating their superficial symptoms [18,19,20]. Specifically, natural products can inhibit the formation of pathogenic protein aggregates and attenuate the neurotoxicity of pathogenic protein aggregates [16]. For example, natural products respond to autophagic pathways to reduce neurological damage such as oxidative stress from pathogenic protein aggregates [21,22,23]. In addition, natural products cleave β-amyloid structures to reduce aggregates formed by pathogenic proteins [24,25]. Similarly, natural products reduce levels of key enzyme activity that forms aggregates to inhibit oligomer formation [21,26,27]. Natural products offer new avenues for research into inhibiting the formation of disease-causing protein aggregates and thereby alleviating disease symptoms.
2. Natural Products Reduce Tau Aggregation by Affecting Aggregate Formation, Disaggregation, and Key Enzyme Activity
Tau is a phosphoprotein with a natively unfolded conformation that functions to stabilize microtubules in axons. Microtubules form the cytoskeleton of the cell and are essential for maintaining the structural integrity of the cell and transporting nutrients from the soma down the axon to the synaptic terminal [129,130,131,132]. In the adult human central nervous system, tau proteins exist as six heterodimers containing 0, 1, or 2 amino-terminal inserts and 3 or 4 microtubule-binding repeat (3R or 4R) domains. Those repeats, containing 31 or 32 amino acid residues, form domains that stabilize microtubules and promote microtubule assembly [133,134]. The ability of tau to bind to microtubules is also regulated by the post-translational modification of proteins, including phosphorylation, glycosylation, glycation, ubiquitination, sumoylation, and nitration [131,135]. Tau has multiple kinase phosphorylation sites and its functions are partly regulated by its phosphorylation status [136,137]. In all neurodegenerative diseases associated with the tau protein, this protein is present in a hyperphosphorylated form, which is responsible for its aggregation and leads to neuronal dysfunction and death. The aggregation of tau is a multi-step process; the initial step is the formation of the β-sheets of tau, i.e., MTBR regions of tau stacked on top of each other [138]. Then, it forms dimers and trimers, followed by small soluble oligomers. These small soluble oligomers form twisted tau filaments called PHFs, which subsequently form neurofibrillary tangles (NFTs) [139]. Tau-associated diseases are known as tauopathies and include Alzheimer’s disease (AD), progressive supranuclear palsy (PSP), Pick’s disease, frontotemporal dementia (FTD), corticobasal degeneration, and variants of Parkinson’s disease (PD) and Lewy body dementia (LBD), for which NFTs are a common histopathological marker [135,140,141]. In addition, tau oligomers exhibit toxic effects in tauopathies prior to the formation of NFTs and are capable of potentiating neuronal damage, leading to neurodegeneration and traumatic brain injury [142]. Current drug strategies targeting the tau protein can be summarized as an inhibition of tau aggregation, inhibition of tau phosphorylation, reduction in tau levels and tau immunization [143]. Here, we review some of the compounds that have been shown to affect tau proteins.
In mouse cortical neuronal cells expressing induced wild-type tau and in primary cortical neurons, Fistein significantly reduced phosphorylated tau levels, which was highly dependent on TFEB and Nrf2 activation and occurred via selective autophagy by its cargo receptors [144]. Tau K18 is a widely used model for full-length tau proteins, as they exhibit very similar physiological and pathological functions [145]. In vitro, Fisetin has been shown to limit the extent of tau K18-protofibril formation by inhibiting tau K18 aggregation (Figure 2), resulting in shorter and thinner tau protofibrils. In HEK293/tau441, treatment with Fisetin reduced tau oligomers and significantly decreased the ratio of insoluble-to-soluble tau protein [82]. And treatment with Fisetin (20 mg/kg, i.p., 2 weeks) significantly reduced p-tau levels at Ser413 induced by Aβ(1–42) injection (i.c.v.) in the hippocampus of mice [146].
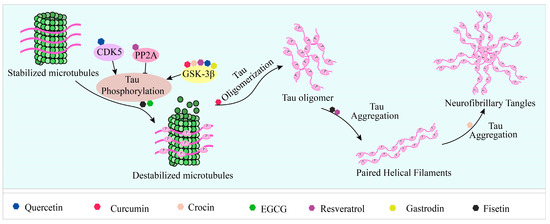
Figure 2. Natural products reduce tau aggregation, inhibit hyperphosphorylation, or act on formation processes. During the multistep process of tau aggregation, fisetin and EGCG reduce the phosphorylation level of tau. Curcumin, crocin, gastrodin, quercetin, and resveratrol can inhibit GSK3β activity and thus tau hyperphosphorylation. In addition, resveratrol and quercetin can inhibit tau phosphorylation by activating PP2A and inhibiting CDK5 activity, respectively. During the formation of tau oligomers, curcumin can inhibit its oligomerization. Fisetin and resveratrol can inhibit the accumulation of oligomers into PHFs, and curcumin can inhibit the further formation of NFTs from PHFs.
Crocin has been shown to inhibit neuronal death [147,148], protect rats from brain ischemia/reperfusion injury, and enhance long-term potentiation, learning, recognition and memory [83,149,150]. In vitro, crocin inhibited the conversion of tau protein into more aggregated conformations during the fibrillation process by binding to its intermediate structures and inhibited 50% of tau aggregates at a dose of 100 µg/mL [151]. In rats, co-treatment with 25 mg/kg crocin significantly reversed the level of acrolein-induced phosphorylation of tau in the cerebral cortex by attenuating the active forms of ERK and JNK kinases [152]. GSK-3β is the most important protein kinase that regulates tau phosphorylation, when it is overactivated, tau is hyperphosphorylated. In PC12-htau cells, tau is hyperphosphorylated at Thr231 and Ser199/Ser202 compared to PC12 cells. In PC12-htau it has been shown that trans-Crocin 4 decreases the amount and phosphorylation of tau at the pThr231 and pSer199/Ser202 epitopes, and inhibits the active forms of GSK3β and ERK1/2 kinases [153].
Resveratrol (RES) has pharmacological properties with antioxidant, anti-inflammatory, hepatoprotective, anti-diabetic, and anti-tumor effects [154,155]. It is believed to have therapeutic potential in the treatment of neurodegenerative diseases. For example, treatment with RES reduced tau phosphorylation in the hippocampus of diabetic mice fed a high-fat diet, resulting in improved memory impairment [156]. An in vitro ThT fluorescence assay showed that RES inhibited tau aggregation, resulting in the formation of smaller aggregates rather than long fibers. Moreover, it prevented extracellular tau oligomers from binding to N2a cells, reduced tau propagation, and decreased the levels of phosphorylated tau and tau oligomers in the brains of PS19 mice [58]. In addition to GSK-3β, calmodulin-dependent protein kinase II (CaMKII) and phosphoserine/phosphothreonine protein phosphatase-2A (PP2A) are also important enzymes involved in the regulation of tau protein hyperphosphorylation [157,158,159,160,161]. RES inhibited formaldehyde-induced increasing phosphorylation of GSK-3β and CaMKII protein levels to prevent tau protein hyperphosphorylation, thereby protecting N2a cells from formaldehyde-induced damage [162]. PP2A dephosphorylates tau, preventing its microtubule dissociation and PHF formation. MID1 is a negative regulator of PP2A and mediates the ubiquitin-specific degradation of PP2A. The loss of its function results in increased PP2A protein levels and activity [163]. Both in vitro and in vivo, RES treatment destabilized the ubiquitin ligase MID1 and its mRNA, which directly interfered with the MID1–α4–PP2A degradation complex by decreasing MID1 protein expression, leading to an increase in microtubule-associated PP2A activity and the time- and dose- dependent dephosphorylation of tau [164]. Similarly, in the brain of CdCl2-treated rats, trans-resveratrol inhibited tau phosphorylation by activating PP2A and inhibiting GSK3β activity. In particular, the inhibition of GSK3β activity was mediated by AMPK-induced activation of the PI3K/Akt signaling pathway [165]. In addition, RES inhibited alum-induced tau hyperphosphorylation at the Ser396 site in rat hippocampal slices by decreasing ERK1/2 activation and increasing GSK-3β Ser9 phosphorylation [166]. In optic nerve head astrocytes (ONHAs) undergoing oxidative stress, pretreatment with resveratrol not only increased cell viability, but also reduced the levels of activated caspases and dephosphorylation of the tau protein at Ser422, thereby reducing caspase-mediated tau cleavage and neurogenic fiber tangle (NFT) formation [167].
As mentioned above, quercetin, curcumin, and EGCG exerted potent neuroprotective effects in inhibiting Aβ formation and attenuating Aβ toxicity. In addition to this, they also show protective effects in terms of lowering tau phosphorylation levels and reducing the levels of aggregated tau. Quercetin-3-O-glucuronide (Q3G), a major quercetin metabolite in human plasma, has been reported to have potential neuroprotective effects [168]. Pretreatment with 10 µM quercetin or Q3G inhibited okadaic acid (OA)-induced phosphorylation of the tau protein in SH-SY5Y. An oral administration of quercetin also effectively attenuated overexpression of the tau protein phosphorylation in the hippocampus of mice during HFD feeding. Further experiments demonstrated that this was due to the activation of AMPK and inhibition of GSK3β activation by enhancing phosphorylation at the Ser 9 residue [169]. Cell cycle protein-dependent kinase 5 (CDK5) is one of the kinases that affect tau phosphorylation, and overactivated CDK5 activity leads to an abnormal phosphorylation of tau [170]. Quercetin inhibited CDK5 activity, blocked the Ca2+–calpain–p25–CDK5 signaling pathway, and inhibited tau phosphorylation at four sites (Ser396, Ser199, Thr205, and Thr231), thus exhibiting significant neuroprotective effects on OA-induced Ht22 cells [171]. In vitro, quercetin was shown through ThT fluorometry to inhibit tau fibrillization and disassemble pre-formed aggregates of the tau protein [65]. Curcumin has long been shown to inhibit GSK-3β activity and prevent tau hyperphosphorylation, thereby protecting SH-SY5Y from Aβ-induced mitochondrial dysfunction [172,173]. In vitro, curcumin has been shown to inhibit the formation of tau β-sheets, inhibit tau fibrillation, and degrade formed tau filaments, thereby reducing the level of aggregated tau, with 20 µM curcumin leading to 75 ± 10% disaggregation of tau aggregates [51]. As for EGCG, in vitro, it blocked K18ΔK280 aggregation and inhibited the formation of potentially proteotoxic oligomeric tau species [174]. In primary neurons, phospho-tau (p-S396/404, p-S262, and p-T231) and total tau levels decreased after 24 h of 50 µM EGCG treatment, but mRNA levels of tau were not affected. This suggests that the reduction in tau was due to clearance rather than transcriptional repression [175]. Other studies have also shown that EGCG binds tau in its phosphorylation region with an affinity of the same order of magnitude as kinases (0.5 mM), preventing it from contacting the protein and thus playing a key role in preventing tau aggregation [73].
In addition to the compounds listed above, there are also many potential therapeutic agents in tauopathies. Gastrodin reduced tau phosphorylation levels of Ser396, Ser199, and Thr231, and inhibited GSK3β kinase activity levels in the brains of APP/PS1 transgenic mice [76]. Morin, a natural bioflavonoid, reduces tau hyperphosphorylation by inhibiting GSK3β activity and the CDK5 signaling pathway in mice [176,177]. The monoterpene 1,8-cineole (CIN), present in many plant essential oils, attenuated the abnormal phosphorylation levels of the tau protein at the thr205, thr181, and ser396 sites induced by AGEs in vitro and in vivo [178]. Macelignan, a sort of lignan derived from Myristica fragrans mace, reduced tau phosphorylation in tau-overexpressing cells and primary neurons of 3× AD-transgene mice. It also promoted PP2A activity in tau-overexpressing cells [126]. In addition, plant-derived nobiletin, beta boswellic acid, huperzine A, and caffeine exhibited the inhibition of tau hyperphosphorylation in different mouse models, respectively [179,180,181,182]. Isobavachalcone is the main component extracted from Psoralea corylifolia. In vitro, isobavachalcone can inhibit heparin-induced tau K18 aggregation and break down mature fibrils into shorter and smaller fibrils or short fragments. Furthermore, in N2a cells, it reduced the proportion of apoptosis caused by phosphatidylserine-induced tau K18 oligomer, from 40% to 10%. It also reduced the level of tau phosphorylation by regulating the levels of GSK3β and PP2A [183]. Limonoids (nimbin and salannin), isolated from neem fruit, were able to inhibit hTau40w aggregation and instead form thin, short, fragile tau fragments [184].
3. Natural Products Inhibit, Degrade, and Remodel α-Syn Fibrils to Reduce Accumulation and Toxicity
Alpha-synuclein (α-Syn) is an intrinsically disordered protein [185] that is abundant in the central nervous system [186] and transforms into cross-β-sheets rich amyloid by self-assembly under physiological conditions via partially folded intermediates and soluble oligomers [187]. Some aggregated species of α-Syn formed along the fibrillation are highly toxic and capable of interfering with the functions of different organelles such as mitochondria, endoplasmic reticulum, and plasma membrane [188,189,190]. Furthermore, it may increase oxidative stress, causing severe damages in dopaminergic cells [191,192]. Therefore, molecules that inhibit α-synuclein fibrillization and stabilize it in a non-toxic state can serve as therapeutic molecules that both prevent the accumulation of aggregated α-syn and maintain normal physiological concentrations of α-syn [193].
Studies have identified small molecules, nanoparticles, peptides, and polymers that have the ability to inhibit α-synuclein fibril formation or destabilize preformed α-syn fibrils (Figure 3). Curcumin has been mentioned above for its significant inhibitory effect on the formation of aggregates of Aβ and tau [194,195,196,197]. Curcumin has also been shown to inhibit the aggregation of α-syn in vitro and attenuate the toxicity of α-syn oligomers in cells [52,53]. In addition, curcumin prevented lipopolysaccharide-induced increases in α-syn gene expression in rats [198]. Due to the instability of curcumin in solution, stable curcumin analogues have raised some concerns. Curcumin pyrazole and its derivative (N-(3-nitrophenylpyrazole) curcumin inhibited the aggregation, protofibrosis, and toxicity of α-syn. Through biochemical, biophysical, and cell-based assays, both have been found to exhibit significant efficacy not only in arresting fibrillization and destroying pre-formed fibrils, but also in preventing formation of the A11 conformation in proteins, which can have toxic effects [199]. EGCG is another natural product that has received particular attention for targeting α-syn fibrillization due to its high availability and low toxicity [200,201]. In vitro, EGCG effectively inhibited α-syn fibrillogenesis by binding to naturally unstructured α-syn monomers and preventing their conversion into stable, β-sheet-rich structures. Instead, it promoted the formation of a novel non-structural, non-toxic α-synuclein [66]. In the rat immortalized oligodendrocyte cell line, OLN-93, EGCG immobilized the C-terminal region, moderately reduced the degree of oligomer binding to the membrane, and inhibited the ability of pre-formed oligomers to permeabilize vesicles and induce cytotoxicity [202]. ‘Active’ oligomers (AOs), characterized as a meta-stable and β-sheet-free species, exhibit rapid self-assembly into the radiating amyloid fibrils (RAFs) on the liposome surface, leading to drastic disruption of the membrane structures [203]. EGCG suppressed the membrane-disrupting radiating amyloid fibril formation on the surface of liposomal membranes, thus protecting the cells that can be readily affected by Aos [204]. According to the results of a molecular dynamics simulation, EGCG can disrupt the β-sheet structure and reduce the β-sheet content to remodel α-syn fibrils [205,206].
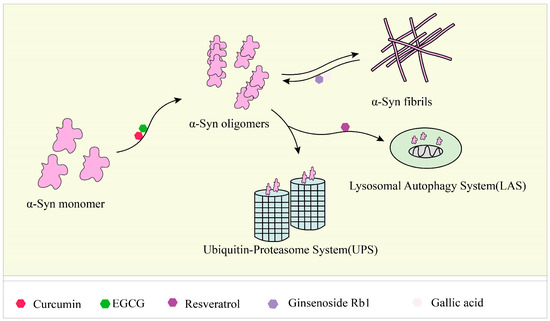
Figure 3. Responses of natural products to α-syn fibrils: inhibition, degradation, and remodeling. In the fibrosis of α-syn, curcumin and EGCG can inhibit its conversion from a monomer to an oligomer, and ginsenoside Rb1 and gallic acid can degrade the formed fibrils. Resveratrol can induce the autophagic degradation of α-syn.
There is evidence that alterations in the autophagy lysosomal pathway of α-synuclein degradation may be preferentially involved in neuronal death and contribute to the pathogenesis of PD [207,208]. RES-activated SIRT1, deacetylated microtubule-associated protein 1 light chain 3 (LC3), and caused the autophagic degradation of α-syn in dopaminergic neurons [84]. Studies have shown that ginsenoside Rb1 effectively inhibited α-syn fibrillation, with an inhibition rate of approximately 90% at 25 µM and incubation for two days. Additionally, Rb1 exhibited a strong ability to decompose preformed fibrils and inhibit the seeded polymerization of α-syn [85]. In vitro thioflavin T fluorescence assays and transmission electron microscopy imaging results showed that GA can inhibit the formation of amyloid fibrils by α-syn and disaggregate preformed α-syn amyloid fibrils. For soluble non-toxic oligomers without β-sheet content, GA can bind to them to stabilize their structure [84,86]. Triptolide (T10) is a monomeric compound isolated from Tripterygium wilfordii Hook f (TWHF). It has anti-inflammatory and anti-tumor activities, as well as neuroprotective effects [209,210]. In neuronal cells, T10 decreased the expression level of α-syn and acted as an autophagy inducer to promote the degradation of α-syn without disturbing lysosomal function [211].
In addition to the above, other compounds have been found to have effects on α-syn aggregation in vitro. For example, the components of saffron, crocin-1, crocin-2, and crocetin, inhibited α-syn aggregation, and dissociated α-syn fibrils [149]. The compounds in Rose damascena can inhibit α-syn fibrillation and oligomer toxicity [212]. In addition, the combined action of the compounds offers a new possibility. Protocatechuic acid (PCA) and hydroxytyrosol (HT) were able to reduce α-syn toxicity. When PCA (100 μM) and HT (100 μM) were used in combination, they showed a higher inhibition of α-syn protofibril formation and destabilization of α-syn fibrils, of 88% and 62%, respectively [213].
This entry is adapted from the peer-reviewed paper 10.3390/ijms241411275
This entry is offline, you can click here to edit this entry!
