The decellularized extracellular matrix (dECM) is capable of promoting stem cell proliferation, migration, adhesion, and differentiation. It is a promising biomaterial for application and clinical translation in the field of periodontal tissue engineering as it most effectively preserves the complex array of ECM components as they are in native tissue, providing ideal cues for regeneration and repair of damaged periodontal tissue. dECMs of different origins have different advantages and characteristics in promoting the regeneration of periodontal tissue. dECM can be used directly or dissolved in liquid for better flowability.
- periodontal regeneration
- decellularized extracellular matrix
- decellularized cell sheet
1. Introduction
2. dECM Derived from Different Sources
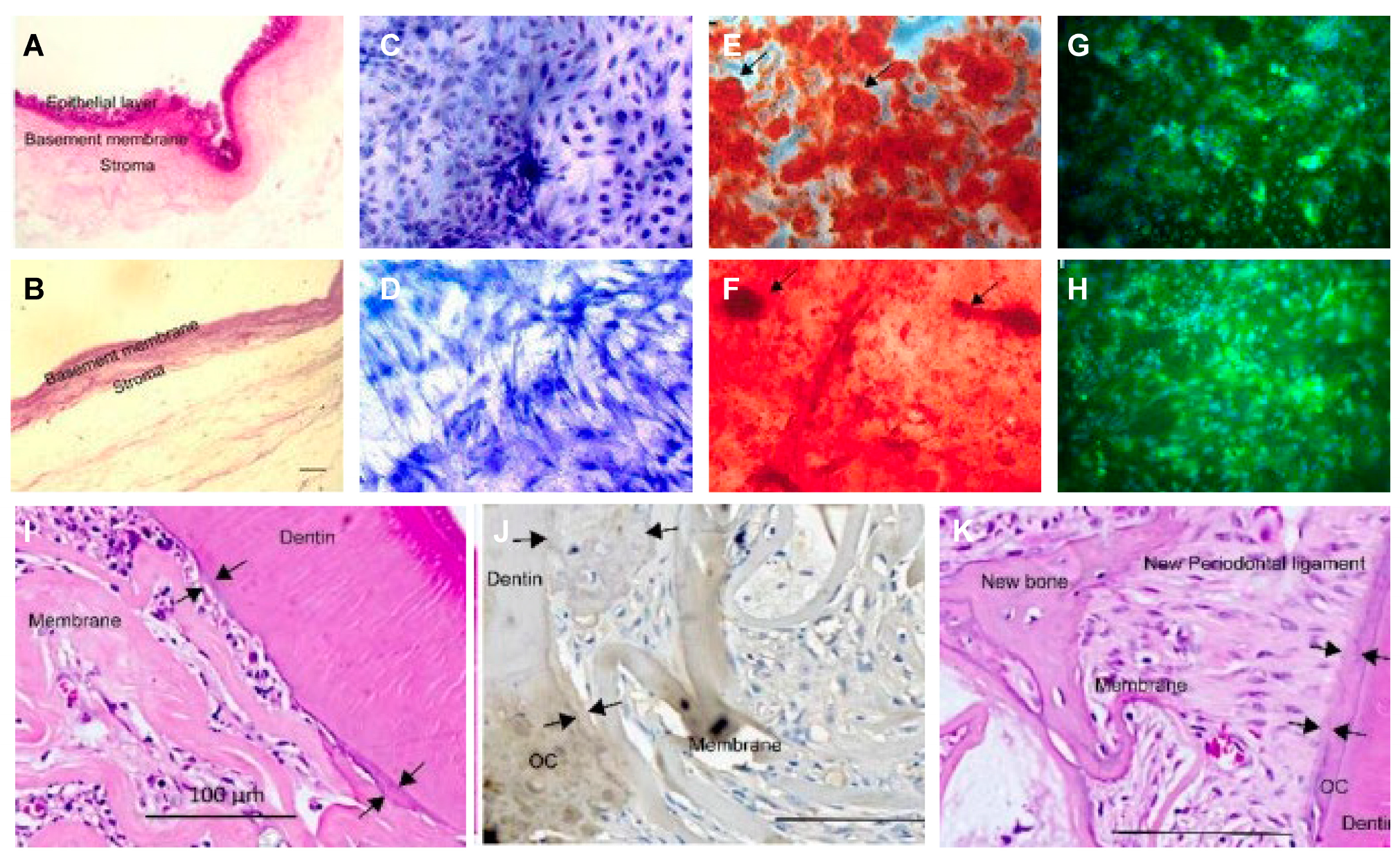
2.1. (Stem) Cell-Derived dECM (Decellularized Cell Sheet)
- (1)
-
Periodontal ligament (stem) cell sheets
- (2)
-
BMC/BMSC sheet:
- (3)
-
Urogenic mesenchymal (stem) cell sheets:
2.2. Tissue-Derived Extracellular Matrix for Periodontal Tissue Engineering Constructs
 : MSCs around T-dECM(dPDL).
: MSCs around T-dECM(dPDL).2.2.1. Human (Allogenic) Tissue Derived dECMs
- (1)
-
Dental (craniofacial)-related human tissues derived dECM
- (2)
-
Non-dental-related tissue-derived dECM
- a.
-
Human amnion dECM
- b.
-
Human umbilical vein dECM
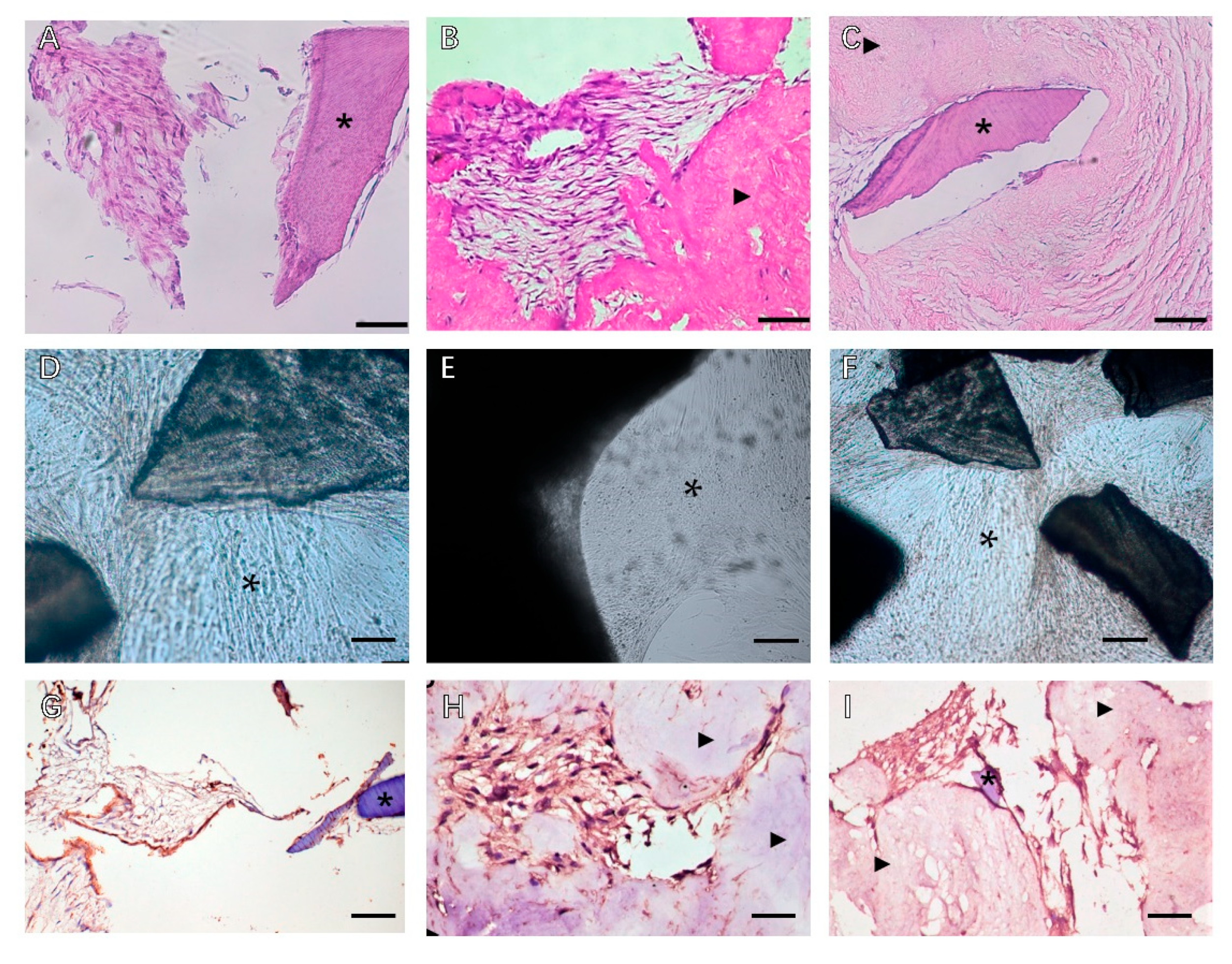
2.2.2. Heterogenous Tissue-Derived dECMs
- (1)
-
Heterogenous dental (craniofacial)-related tissues derived from dECM
- a.
-
Decellularized porcine dental matrix
- b.
-
Decellularized matrix of dog periodontal ligament
- c.
-
Decellularized rat mandible matrix
- (2)
-
Heterogenous, non-dental-related tissue-derived dECM
- a.
-
SIS
- b.
-
Decellularized Amnion
- c.
-
Decellularized pericardium
- d.
-
To sum up, decellularization of natural tissues to produce extracellular matrix is a promising method for 3D scaffolding and for investigating cell-ECM interaction during regeneration of target tissue [3][48]. The fate and behavior of mesenchymal stem cells are influenced by the stem cell niches ideal biochemical and physical cues. Ana Rita Pereira et al. compared the biological behaviors of BMSCs when exposed to C-dECM and T-dECM, and better outcomes were observed in 3D decellularized bone tissue for greater architecture complexity and physicochemical properties [49]. To sum up, tissue-derived dECM has great potential in the context of endogenous periodontal regeneration, with a better effect on preserving the tissue niche intended for different tissues in periodontal defects.
This entry is adapted from the peer-reviewed paper 10.3390/biom13040673
References
- Cho, Y.D.; Kim, K.H.; Lee, Y.M.; Ku, Y.; Seol, Y.J. Periodontal Wound Healing and Tissue Regeneration: A Narrative Review. Pharmaceuticals 2021, 14, 456.
- Feng, Z.; Su, X.; Wang, T.; Guo, S. Identification of Biomarkers That Modulate Osteogenic Differentiation in Mesenchymal Stem Cells Related to Inflammation and Immunity: A Bioinformatics-Based Comprehensive Study. Pharmaceuticals 2022, 15, 1094.
- Liu, C.; Pei, M.; Li, Q.; Zhang, Y. Decellularized extracellular matrix mediates tissue construction and regeneration. Front. Med. 2022, 16, 56–82.
- Wen, Y.; Yang, H.; Wu, J.; Wang, A.; Chen, X.; Hu, S.; Zhang, Y.; Bai, D.; Jin, Z. COL4A2 in the tissue-specific extracellular matrix plays important role on osteogenic differentiation of pessssriodontal ligament stem cells. Theranostics 2019, 9, 4265–4286.
- Kim, B.; Ventura, R.; Lee, B.T. Functionalization of porous BCP scaffold by generating cell-derived extracellular matrix from rat bone marrow stem cells culture for bone tissue engineering. J. Tissue Eng. Regen. Med. 2018, 12, e1256–e1267.
- Xu, Y.; Xu, G.Y.; Tang, C.; Wei, B.; Pei, X.; Gui, J.C.; Min, B.H.; Jin, C.Z.; Wang, L.M. Preparation and characterization of bone marrow mesenchymal stem cell-derived extracellular matrix scaffolds. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 670–678.
- Jiang, Y.; Liu, J.M.; Huang, J.P.; Lu, K.X.; Sun, W.L.; Tan, J.Y.; Li, B.X.; Chen, L.L.; Wu, Y. Regeneration potential of decellularized periodontal ligament cell sheets combined with 15-Deoxy-Δ12,14-prostaglandin J2 nanoparticles in a rat periodontal defect. Biomed. Mater. 2021, 16, 045008.
- Hoang Thi, T.T.; Tran Nguyen, D.H.; Nguyen, D.T.D.; Nguyen, D.H.; Truong, M.D. Decellularized Porcine Epiphyseal Plate-Derived Extracellular Matrix Powder: Synthesis and Characterization. Cells Tissues Organs 2020, 209, 101–109.
- Liu, Y.; Zhang, Y.; Mei, T.; Cao, H.; Hu, Y.; Jia, W.; Wang, J.; Zhang, Z.; Wang, Z.; Le, W.; et al. hESCs-Derived Early Vascular Cell Spheroids for Cardiac Tissue Vascular Engineering and Myocardial Infarction Treatment. Adv. Sci. (Weinh) 2022, 9, e2104299.
- Xu, Y.; Zhou, J.; Liu, C.; Zhang, S.; Gao, F.; Guo, W.; Sun, X.; Zhang, C.; Li, H.; Rao, Z.; et al. Understanding the role of tissue-specific decellularized spinal cord matrix hydrogel for neural stem/progenitor cell microenvironment reconstruction and spinal cord injury. Biomaterials 2021, 268, 120596.
- Kim, H.; Jang, J.H.; Han, W.; Hwang, H.J.; Jang, J.; Kim, J.Y.; Cho, D.W. Extracellular matrix-based sticky sealants for scar-free corneal tissue reconstruction. Biomaterials 2023, 292, 121941.
- Farag, A.; Hashimi, S.M.; Vaquette, C.; Bartold, P.M.; Hutmacher, D.W.; Ivanovski, S. The effect of decellularized tissue engineered constructs on periodontal regeneration. J. Clin. Periodontol. 2018, 45, 586–596.
- Farag, A.; Hashimi, S.M.; Vaquette, C.; Volpato, F.Z.; Hutmacher, D.W.; Ivanovski, S. Assessment of static and perfusion methods for decellularization of PCL membrane-supported periodontal ligament cell sheet constructs. Arch. Oral Biol. 2018, 88, 67–76.
- Xu, F.; Zheng, Z.; Yao, M.; Zhu, F.; Shen, T.; Li, J.; Zhu, C.; Yang, T.; Shao, M.; Wan, Z.; et al. A regulatory mechanism of a stepwise osteogenesis-mimicking decellularized extracellular matrix on the osteogenic differentiation of bone marrow-derived mesenchymal stem cells. J. Mater. Chem. B 2022, 10, 6171–6180.
- Yang, X.; Xiong, X.; Zhou, W.; Feng, G.; Zhang, Y.; Dai, H.; Zhou, J. Effects of human urine-derived stem cells on the cementogenic differentiation of indirectly-cocultured periodontal ligament stem cells. Am. J. Transl. Res. 2020, 12, 361–378.
- Xiong, X.; Yang, X.; Dai, H.; Feng, G.; Zhang, Y.; Zhou, J.; Zhou, W. Extracellular matrix derived from human urine-derived stem cells enhances the expansion, adhesion, spreading, and differentiation of human periodontal ligament stem cells. Stem. Cell Res. Ther. 2019, 10, 396.
- Hoshiba, T.; Lu, H.; Yamada, T.; Kawazoe, N.; Tateishi, T.; Chen, G. Effects of extracellular matrices derived from different cell sources on chondrocyte functions. Biotechnol. Prog. 2011, 27, 788–795.
- Huang, J.P.; Wu, Y.M.; Liu, J.M.; Zhang, L.; Li, B.X.; Chen, L.L.; Ding, P.H.; Tan, J.Y. Decellularized matrix could affect the proliferation and differentiation of periodontal ligament stem cells in vitro. J. Periodontal. Res. 2021, 56, 929–939.
- Junka, R.; Zhou, X.; Wang, W.; Yu, X. Albumin-Coated Polycaprolactone (PCL)-Decellularized Extracellular Matrix (dECM) Scaffold for Bone Regeneration. ACS Appl. Bio. Mater. 2022, 5, 5634–5644.
- Ventura, R.D.; Padalhin, A.R.; Kim, B.; Park, M.; Lee, B.T. Evaluation of bone regeneration potential of injectable extracellular matrix (ECM) from porcine dermis loaded with biphasic calcium phosphate (BCP) powder. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 110, 110663.
- Gao, C.Y.; Huang, Z.H.; Jing, W.; Wei, P.F.; Jin, L.; Zhang, X.H.; Cai, Q.; Deng, X.L.; Yang, X.P. Directing osteogenic differentiation of BMSCs by cell-secreted decellularized extracellular matrixes from different cell types. J. Mater. Chem. B 2018, 6, 7471–7485.
- Safari, F.; Fani, N.; Eglin, D.; Alini, M.; Stoddart, M.J.; Baghaban Eslaminejad, M. Human umbilical cord-derived scaffolds for cartilage tissue engineering. J. Biomed. Mater. Res. A 2019, 107, 1793–1802.
- Gilbert, T.W.; Sellaro, T.L.; Badylak, S.F. Decellularization of tissues and organs. Biomaterials 2006, 27, 3675–3683.
- Crapo, P.M.; Gilbert, T.W.; Badylak, S.F. An overview of tissue and whole organ decellularization processes. Biomaterials 2011, 32, 3233–3243.
- Zhang, Y.; He, Y.; Bharadwaj, S.; Hammam, N.; Carnagey, K.; Myers, R.; Atala, A.; Van Dyke, M. Tissue-specific extracellular matrix coatings for the promotion of cell proliferation and maintenance of cell phenotype. Biomaterials 2009, 30, 4021–4028.
- Son, H.; Jeon, M.; Choi, H.J.; Lee, H.S.; Kim, I.H.; Kang, C.M.; Song, J.S. Decellularized human periodontal ligament for periodontium regeneration. PLoS ONE 2019, 14, e0221236.
- Kim, I.H.; Jeon, M.; Cheon, K.; Kim, S.H.; Jung, H.S.; Shin, Y.; Kang, C.M.; Kim, S.O.; Choi, H.J.; Lee, H.S.; et al. In Vivo Evaluation of Decellularized Human Tooth Scaffold for Dental Tissue Regeneration. Appl. Sci. 2021, 11, 8472.
- Iwasaki, K.; Peng, Y.; Kanda, R.; Umeda, M.; Ishikawa, I. Stem Cell Transplantation and Cell-Free Treatment for Periodontal Regeneration. Int. J. Mol. Sci. 2022, 23, 1011.
- Liang, J.; Yi, P.; Wang, X.; Huang, F.; Luan, X.; Zhao, Z.; Liu, C. Acellular matrix hydrogel for repair of the temporomandibular joint disc. J. Biomed. Mater. Res. B Appl. Biomater. 2020, 108, 2995–3007.
- Lee, D.J.; Miguez, P.; Kwon, J.; Daniel, R.; Padilla, R.; Min, S.; Zalal, R.; Ko, C.C.; Shin, H.W. Decellularized pulp matrix as scaffold for mesenchymal stem cell mediated bone regeneration. J. Tissue Eng. 2020, 11, 2041731420981672.
- Dziedzic, D.S.M.; Mogharbel, B.F.; Irioda, A.C.; Stricker, P.E.F.; Perussolo, M.C.; Franco, C.R.C.; Chang, H.W.; Abdelwahid, E.; de Carvalho, K.A.T. Adipose-Derived Stromal Cells and Mineralized Extracellular Matrix Delivery by a Human Decellularized Amniotic Membrane in Periodontal Tissue Engineering. Membranes 2021, 11, 606.
- Iwasaki, K.; Akazawa, K.; Nagata, M.; Komaki, M.; Honda, I.; Morioka, C.; Yokoyama, N.; Ayame, H.; Yamaki, K.; Tanaka, Y.; et al. The Fate of Transplanted Periodontal Ligament Stem Cells in Surgically Created Periodontal Defects in Rats. Int. J. Mol. Sci. 2019, 20, 192.
- Venkatesan, N.; Lavu, V.; Balaji, S.K. Clinical efficacy of amniotic membrane with biphasic calcium phosphate in guided tissue regeneration of intrabony defects- a randomized controlled clinical trial. Biomater. Res. 2021, 25, 15.
- Soldatos, N.K.; Stylianou, P.; Koidou, V.P.; Angelov, N.; Yukna, R.; Romanos, G.E. Limitations and options using resorbable versus nonresorbable membranes for successful guided bone regeneration. Quintessence Int. 2017, 48, 131–147.
- Imamura, K.; Hamada, Y.; Yoshida, W.; Murakami, T.; Nakane-Koyachi, S.; Yoshikawa, K.; Saito, A. Investigating the Effects of Dehydrated Human Amnion-Chorion Membrane on Periodontal Healing. Biomolecules 2022, 12, 857.
- Adachi, K.; Amemiya, T.; Nakamura, T.; Honjyo, K.; Kumamoto, S.; Yamamoto, T.; Bentley, A.J.; Fullwood, N.J.; Kinoshita, S.; Kanamura, N. Human periodontal ligament cell sheets cultured on amniotic membrane substrate. Oral Dis. 2014, 20, 582–590.
- Goktas, S.; Pierre, N.; Abe, K.; Dmytryk, J.; McFetridge, P.S. Cellular interactions and biomechanical properties of a unique vascular-derived scaffold for periodontal tissue regeneration. Tissue Eng. Part A 2010, 16, 769–780.
- Goktas, S.; Matuska, A.M.; Pierre, N.; Gibson, T.M.; Dmytryk, J.J.; McFetridge, P.S. Decellularization method influences early remodeling of an allogenic tissue scaffold. J. Biomed. Mater. Res. A 2014, 102, 8–16.
- Han, X.; Liao, L.; Zhu, T.; Xu, Y.; Bi, F.; Xie, L.; Li, H.; Huo, F.; Tian, W.; Guo, W. Xenogeneic native decellularized matrix carrying PPARγ activator RSG regulating macrophage polarization to promote ligament-to-bone regeneration. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 116, 111224.
- Lee, S.J.; Nah, H.; Heo, D.N.; Kim, K.-H.; Seok, J.M.; Heo, M.; Moon, H.-J.; Lee, D.; Lee, J.S.; An, S.Y.; et al. Induction of osteogenic differentiation in a rat calvarial bone defect model using an In situ forming graphene oxide incorporated glycol chitosan/oxidized hyaluronic acid injectable hydrogel. Carbon 2020, 168, 264–277.
- Nakamura, N.; Ito, A.; Kimura, T.; Kishida, A. Extracellular Matrix Induces Periodontal Ligament Reconstruction In Vivo. Int. J. Mol. Sci. 2019, 20, 3277.
- Gou, M.; Huang, Y.Z.; Hu, J.G.; Jiang, Y.L.; Zhang, X.Z.; Su, N.C.; Lei, Y.; Zhang, H.; Wang, H.; Xie, H.Q. Epigallocatechin-3-gallate Cross-Linked Small Intestinal Submucosa for Guided Bone Regeneration. ACS Biomater. Sci. Eng. 2019, 5, 5024–5035.
- Wilshaw, S.P.; Kearney, J.; Fisher, J.; Ingham, E. Biocompatibility and potential of acellular human amniotic membrane to support the attachment and proliferation of allogeneic cells. Tissue Eng. Part A 2008, 14, 463–472.
- Semyari, H.; Rajipour, M.; Sabetkish, S.; Sabetkish, N.; Abbas, F.M.; Kajbafzadeh, A.M. Evaluating the bone regeneration in calvarial defect using osteoblasts differentiated from adipose-derived mesenchymal stem cells on three different scaffolds: An animal study. Cell Tissue Bank. 2016, 17, 69–83.
- Bianchi, S.; Bernardi, S.; Simeone, D.; Torge, D.; Macchiarelli, G.; Marchetti, E. Proliferation and Morphological Assessment of Human Periodontal Ligament Fibroblast towards Bovine Pericardium Membranes: An In Vitro Study. Materials 2022, 15, 8284.
- Suzuki, M.; Kimura, T.; Yoshida, Y.; Kobayashi, M.; Hashimoto, Y.; Takahashi, H.; Shimizu, T.; Anzai, S.; Nakamura, N.; Kishida, A. In Vitro Tissue Reconstruction Using Decellularized Pericardium Cultured with Cells for Ligament Regeneration. Polymers 2022, 14, 2351.
- Suzuki, M.; Kimura, T.; Nakano, Y.; Kobayashi, M.; Okada, M.; Matsumoto, T.; Nakamura, N.; Hashimoto, Y.; Kishida, A. Preparation of mineralized pericardium by alternative soaking for soft-hard interregional tissue application. J. Biomed. Mater. Res. A 2023, 111, 198–208.
- Moffat, D.; Ye, K.; Jin, S. Decellularization for the retention of tissue niches. J. Tissue Eng. 2022, 13, 20417314221101151.
- Pereira, A.R.; Trivanović, D.; Stahlhut, P.; Rudert, M.; Groll, J.; Herrmann, M. Preservation of the naïve features of mesenchymal stromal cells in vitro: Comparison of cell- and bone-derived decellularized extracellular matrix. J. Tissue Eng. 2022, 13.
