The orthodontics field is constantly looking for innovations to improve mechanical efficiency of tooth movement and patient's quality of life during treatment. New scientific reports on phototherapy and how it can optimize different stages of corrective treatment (before, during and after treatment) are discussed. Recurrent conditions that can be treated with lasers include removal of carious tissue, dentine hypersensitivity, and temporomandibular disorders. There is evidence that laser treatment optimize recovery, enabling the individual to start orthodontic treatment sooner. Along orthodontic interventions, photobiomodulation therapy is indicated for post-activation analgesia, repairing traumatic ulcers, and accelerating tooth movement. In addition, antimicrobial photodynamic therapy is also suitable for effective decontamination of oral infections such as herpes lesions and peri-implantitis. Finally, high-intensity lasers are a powerful ally in removing brackets and restoring the red aesthetics. The use of light sources in orthodontic routines has many advantages, including simplicity of technique, ease of handling of the appliance, minimal invasiveness, and patient comfort during the procedure. It is crucial that professionals develop a critical view of technological advances to provide safe, evidence-based treatments. Laser treatment improves the patient's experience during orthodontic treatment and minimizes side effects of clinical procedures.
- orthodontics
- orthodontic practice
- laser
- high-power laser
- photobiomodulation
- antimicrobial photodynamic therapy
1. Pre-Orthodontic Treatment Care
2. Pain Control of Orthodontic Activation Responses
After orthodontic activation (OA), the periodontal ligament initiates a pro-inflammatory cascade to restore tissue dynamics. Vascular changes and the release of neurogenic and pro-inflammatory mediators may trigger local pain [16]. The gold standard for pain control after orthodontic procedures is the use of analgesic or anti-inflammatory drugs. However, not all patients accept frequent medication use, and the effects of such pharmaceuticals on tooth movement are controversial [17].
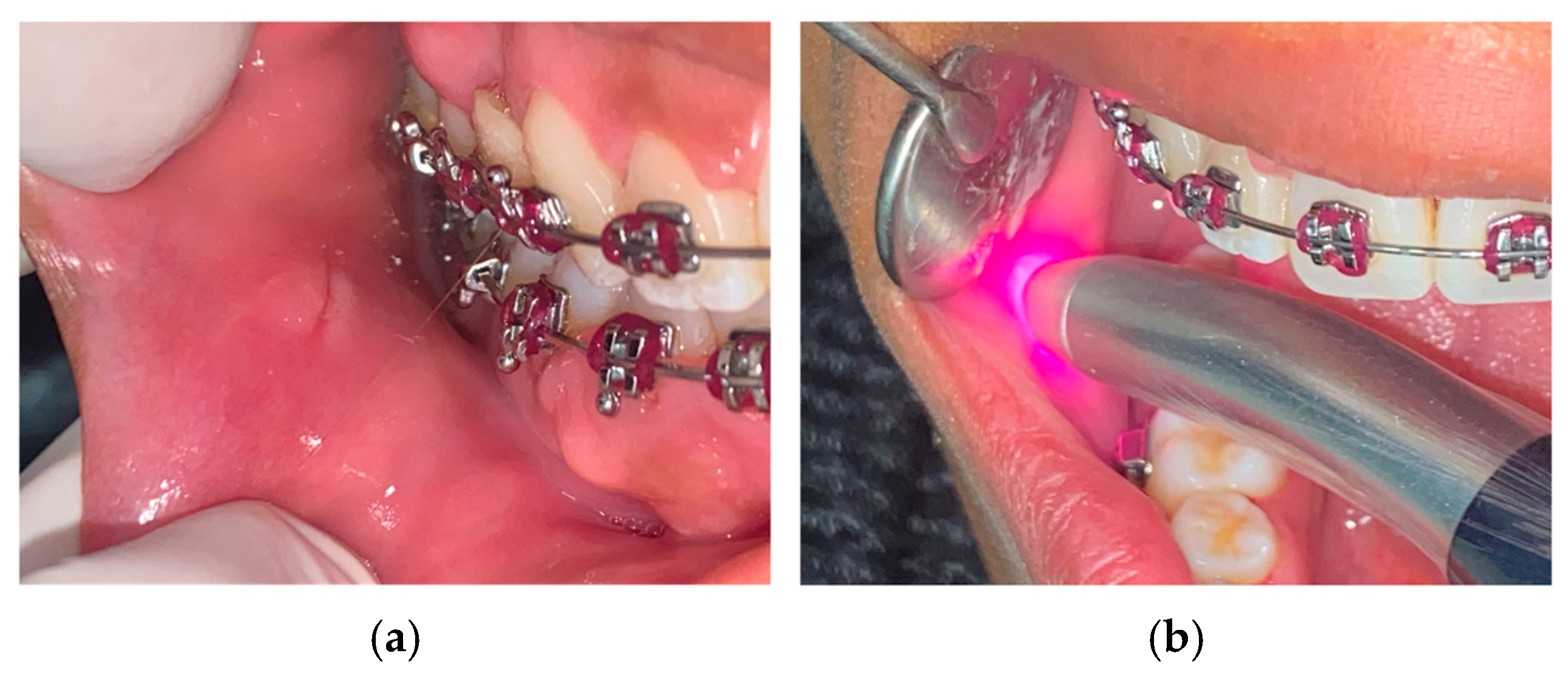
Several studies have shown that PBMT is a non-toxic and effective alternative for pain management after orthodontic activation [18][19][20][21]. With just one session of irradiation immediately after orthodontic activation (Figure 2), PBMT can significantly reduce pain sensitivity by altering the depolarization threshold of nerve endings in the periodontal ligament. It also promotes pain relief by modulating the production of pain mediators and stimulating the peripheral release of endogenous endorphins [10][22][23]. PBMT reduces the number of pain signals that reaches the brain and prevents sensitization of central neurons. Brito et al. [18] conducted a double-blind RCT and reported that patients who received irradiation after initial alignment arch placement expressed pain relief at 6, 24, 48, and 72 hours compared with controls. This analgesic effect has also been observed with the placement of interdental separators, reducing the need for medication [24][25].
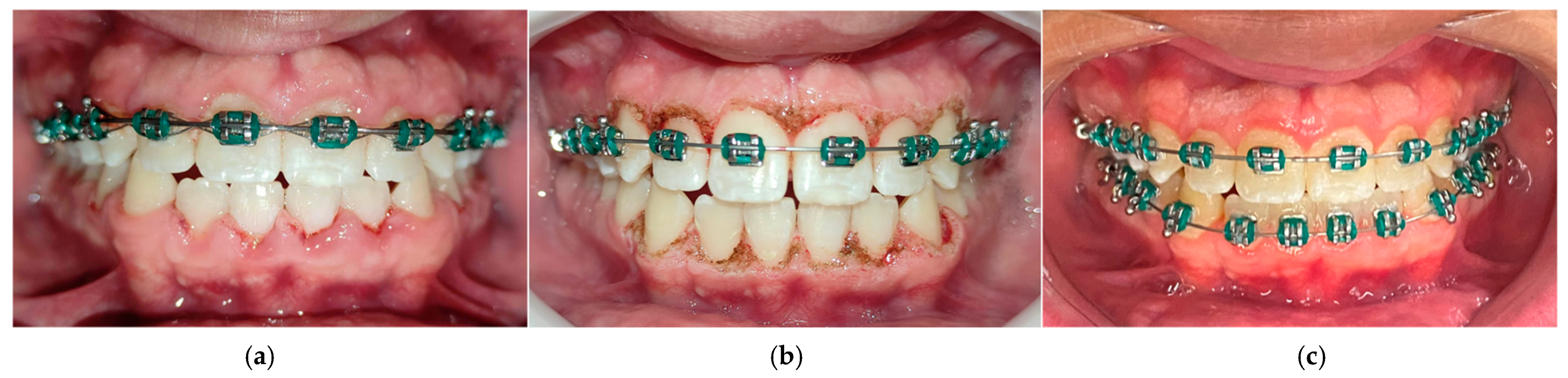
3. Photobiomodulating Tooth Movement
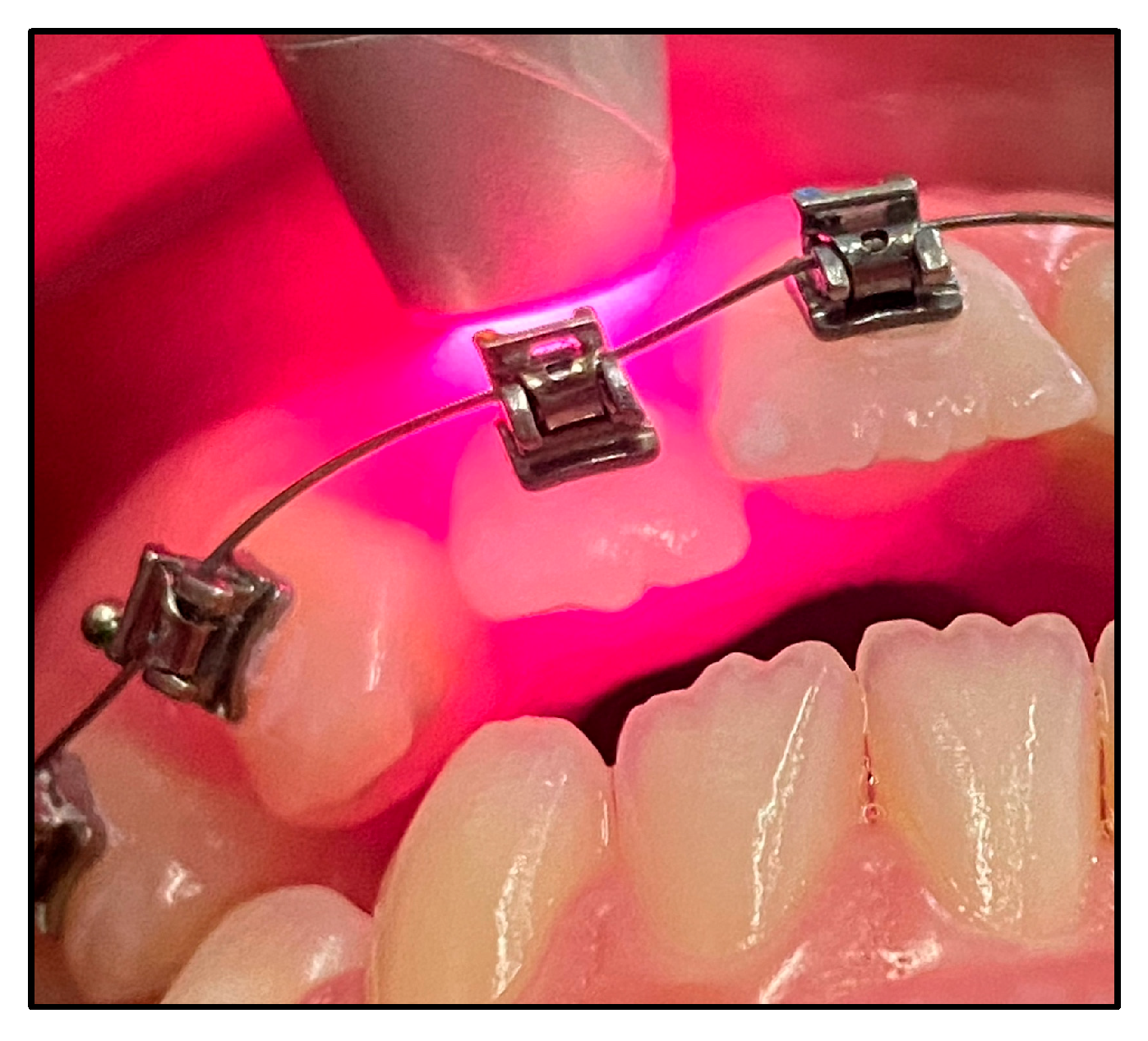
The duration of orthodontic treatment is a major concern for orthodontic professionals and patients because the appliances have a significant impact on patient quality of life related to oral health [26]. Considerable efforts have been made to develop treatments that can facilitate tooth movement, including techniques such as corticectomy and microosteoperforation. Studies conducted in animal and human models have already shown that PBMT is a promising adjunctive tool for improving tooth movement (Figure 3), demonstrating efficacy, safety, and most importantly no side effects [27][28][29][30][31][32][33][34][35].

Orthodontic mechanics is based on periodontal tissue remodeling through activation of various components such as periodontal fibroblasts, osteoblasts, osteocytes, osteoclasts and vasculature alterations. In vitro and in vivo studies suggest that PBMT promotes cell differentiation, activates osteoclasts and osteoblasts, stimulates collagen synthesis, and promotes angiogenesis, thereby creating a conducive environment for tooth migration [20].
4. Assisting Tool in Rapid Maxillary Expansion
5. Postoperative Care with Lasers
Photobiomodulation can significantly improve the postoperative phase of surgical procedures such as tooth extraction, orthognathic surgeries, or other that may lead to complications and impact the quality of life of patients.
The immediate postoperative period is usually associated with inflammatory symptoms, such as swelling, pain, and decreased mandibular function. PBMT not only modulates the inflammatory course, but also promotes analgesia, and tissue repair [45][46].
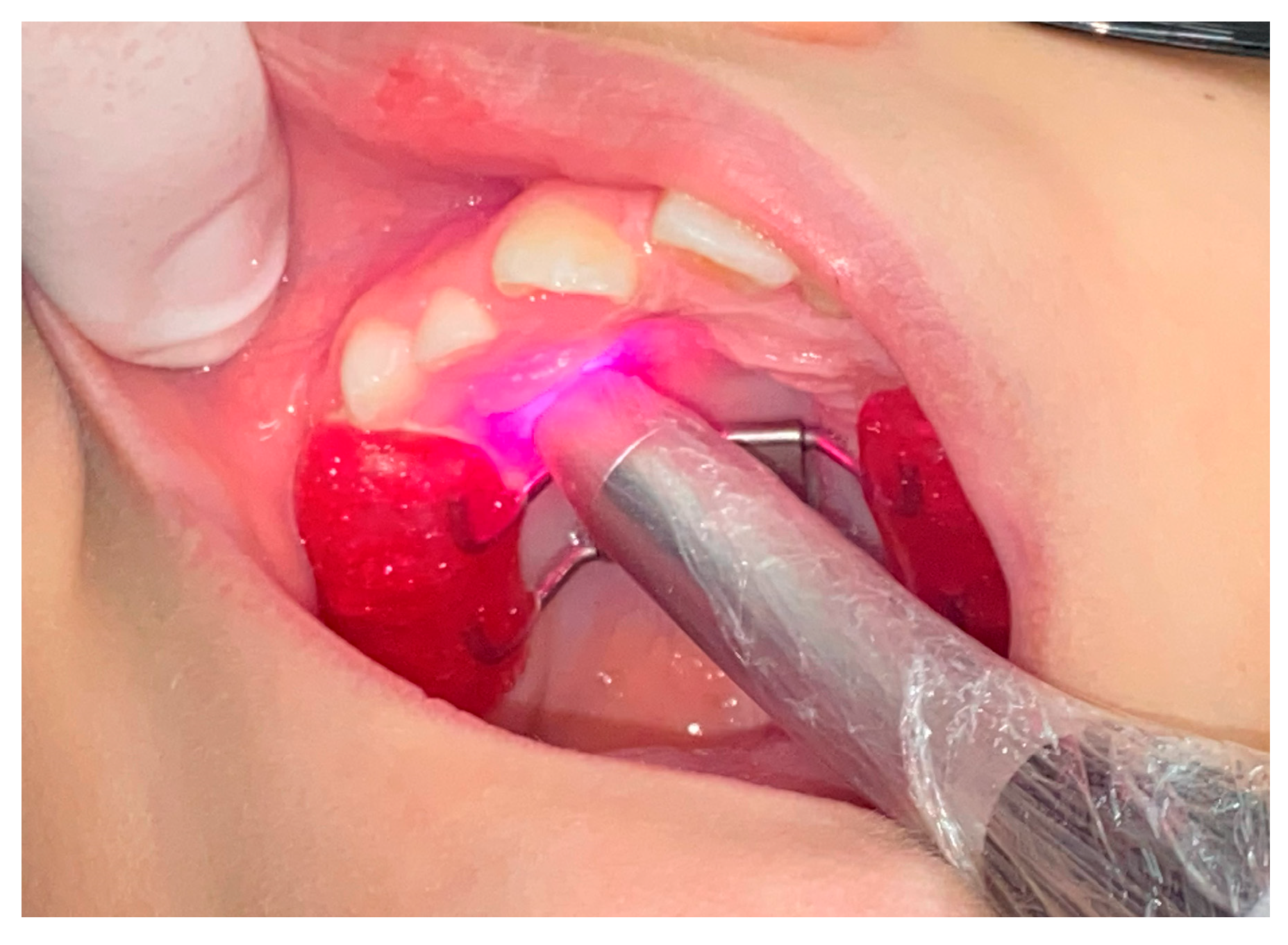
Eshghpour et al. [47] demonstrated the effectiveness of PBMT in alleviating pain and edema after the removal of impacted third molars in a split-mouth RCT (Figure 5). Domínguez Camacho et al. [48] defends that PBMT is an important adjunct to oral anti-inflammatory drugs to reduce post-surgical edema in orthognathic surgery patients. Feslihan and Eroğlu [49] states that PBMT is an alternative to corticosteroids after impacted third molar surgery, as it has similar clinical efficacy in controlling pain, swelling, and trismus. Considering the side effects of anti-inflammatory drugs, PBMT has increasing relevance to modern dentistry [50][51][52][53].
Photobiomodulation therapy is highly recommended to treat paresthesia and paralysis, one of the most persistent complications after major orofacial surgery. With the appropriate parameters, laser light helps restore neurosensory function by optimizing regeneration of peripheral axons and promoting sprouting of adjacent new nerve endings [46]. Oliveira et al. [4] noted that the success rate of PBMT in nerve repair depends on the time interval from nerve injury to initiation of treatment. Considering that the orthodontist determines the appropriate surgical time for each case during her OT, it is important that the professional also schedules PBMT sessions to ensure the patient's optimal recovery.
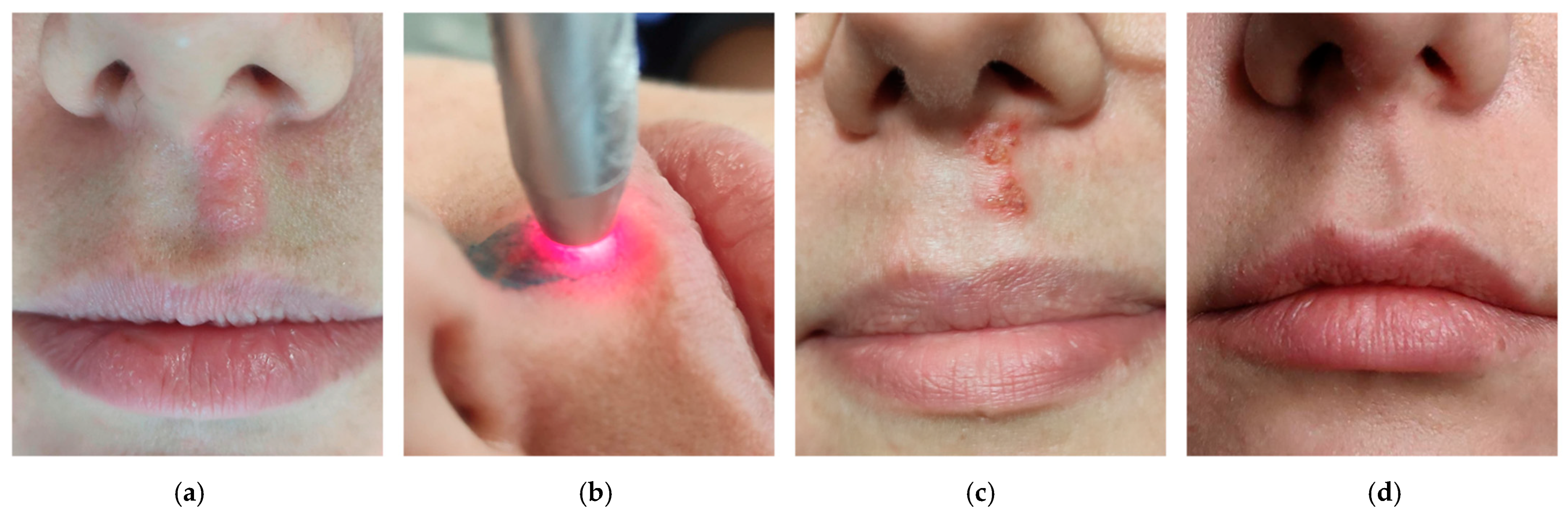
6. aPDT to Manage Infections during Orthodontic Treatment
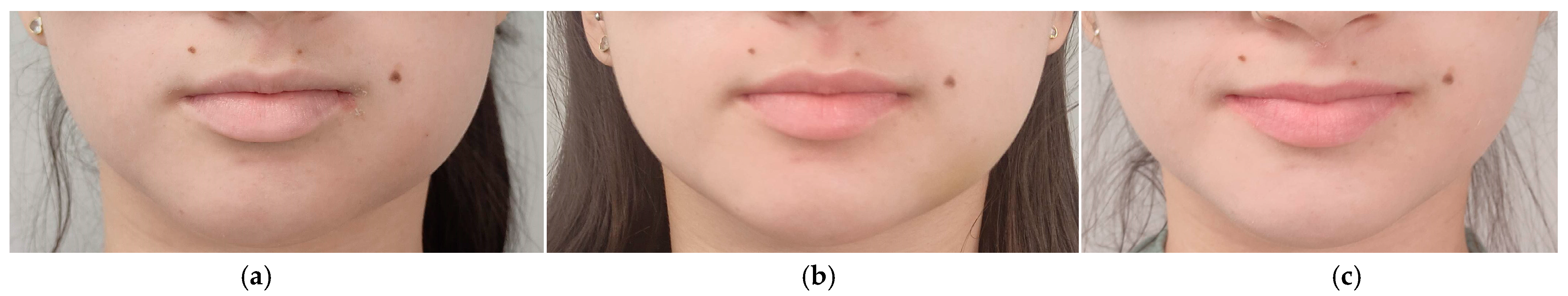
7. Soft Tissue Management with High-Intensity Lasers Complementing Orthodontic Therapy
From a minimally invasive procedure perspective, orthodontists should consider incorporating high intensity laser technology into their clinical routine. By understanding the properties of different light sources and having the appropriate technical training, orthodontists can use lasers to effectively treat both soft and hard tissue, to achieve minimal side effects and make the postoperative period more comfortable for the patient.
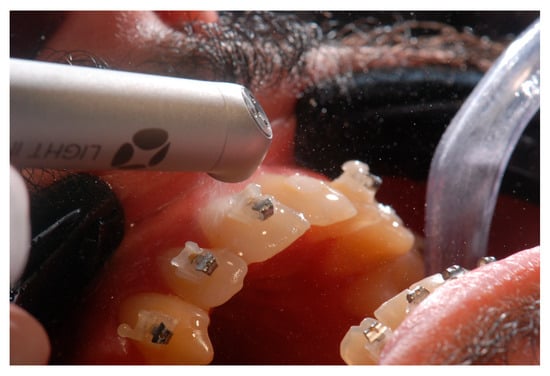
8. Braces Removal with the Touch of Light
This entry is adapted from the peer-reviewed paper 10.3390/photonics10060689
References
- Li, T.; Zhang, X.; Shi, H.; Ma, Z.; Lv, B.; Xie, M. Er:YAG laser application in caries removal and cavity preparation in children: A meta-analysis. Lasers Med. Sci. 2019, 34, 273–280.
- Cattoni, F.; Ferrante, L.; Mandile, S.; Tetè, G.; Polizzi, E.M.; Gastaldi, G. Comparison of Lasers and Desensitizing Agents in Dentinal Hypersensitivity Therapy. Dent. J. 2023, 11, 63.
- Dawdy, J.; Halladay, J.; Carrasco-Labra, A.; Araya, I.; Yanine, N.; Brignardello-Petersen, R. Efficacy of adjuvant laser therapy in reducing postsurgical complications after the removal of impacted mandibular third molars: A systematic review update and meta-analysis. J. Am. Dent. Assoc. 2017, 148, 887–902.e4.
- De Oliveira, R.F.; Da Silva, A.C.; Simões, A.; Youssef, M.N.; De Freitas, P.M. Laser Therapy in the Treatment of Paresthesia: A Retrospective Study of 125 Clinical Cases. Photomed. Laser Surg. 2015, 33, 415–423.
- Luchian, I.; Budală, D.G.; Baciu, E.-R.; Ursu, R.G.; Diaconu-Popa, D.; Butnaru, O.; Tatarciuc, M. The Involvement of Photobiology in Contemporary Dentistry—A Narrative Review. Int. J. Mol. Sci. 2023, 24, 3985.
- Kavaliauskiene, A.; Smailiene, D.; Buskiene, I.; Keriene, D. Pain and discomfort perception among patients undergoing orthodontic treatment: Results from one month follow-up study. Stomatologija 2012, 14, 118–125.
- Erdinç, A.M.E. Perception of pain during orthodontic treatment with fixed appliances. Eur. J. Orthod. 2004, 26, 79–85.
- Rakhshan, H.; Rakhshan, V. Pain and discomfort perceived during the initial stage of active fixed orthodontic treatment. Saudi Dent. J. 2015, 27, 81–87.
- Suter, V.G.A.; Sjölund, S.; Bornstein, M.M. Effect of laser on pain relief and wound healing of recurrent aphthous stomatitis: A systematic review. Lasers Med. Sci. 2017, 32, 953–963.
- Chow, R.T.; Armati, P.J. Photobiomodulation: Implications for Anesthesia and Pain Relief. Photomed. Laser Surg. 2016, 34, 599–609.
- Aggarwal, H. Efficacy of Low-Level Laser Therapy in Treatment of Recurrent Aphthous Ulcers—A Sham Controlled, Split Mouth Follow Up Study. J. Clin. Diagn. Res. 2014, 8, 218–221.
- Lalabonova, H.; Daskalov, H. Clinical assessment of the therapeutic effect of low-level laser therapy on chronic recurrent aphthous stomatitis. Biotechnol. Biotechnol. Equip. 2014, 28, 929–933.
- Parra-Moreno, F.; Egido-Moreno, S.; Schemel-Suárez, M.; González-Navarro, B.; Estrugo-Devesa, A.; López-López, J. Treatment of recurrent aphtous stomatitis: A systematic review. Med. Oral Patol. Oral Cirugía Bucal 2023, 28, e87–e98.
- Liu, H.; Tan, L.; Fu, G.; Chen, L.; Tan, H. Efficacy of Topical Intervention for Recurrent Aphthous Stomatitis: A Network Meta-Analysis. Medicina 2022, 58, 771.
- Ahmed, M.K.; Jafer, M.; Nayeem, M.; Moafa, I.H.; Quadri, M.F.A.; Gopalaiah, H. Low-Level Laser Therapy and Topical Medications for Treating Aphthous Ulcers: A Systematic Review. J. Multidiscip. Healthc. 2020, 13, 1595–1605.
- Ngan, P.; Kess, B.; Wilson, S. Perception of discomfort by patients undergoing orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 47–53.
- Bertolini, A.; Ferrari, A.; Ottani, A.; Guerzoni, S.; Tacchi, R.; Leone, S. Paracetamol: New Vistas of an Old Drug. CNS Drug Rev. 2006, 12, 250–275.
- Brito, M.H.; Nogueira, C.Q.; Cotrin, P.; Fialho, T.; Oliveira, R.C.; Oliveira, R.G.; Salmeron, S.; Valarelli, F.P.; Freitas, K.M.S.; Cançado, R.H. Efficacy of Low-Level Laser Therapy in Reducing Pain in the Initial Stages of Orthodontic Treatment. Int. J. Dent. 2022, 2022, 3934900.
- Zhi, C.; Guo, Z.; Wang, T.; Liu, D.; Duan, X.; Yu, X.; Zhang, C. Viability of Photobiomodulaton Therapy in Decreasing Orthodontic-Related Pain: A Systematic Review and Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2021, 39, 504–517.
- Camacho, A.D.; Reyes, M.B.; Cujar, S.A.V. A systematic review of the effective laser wavelength range in delivering photobiomodulation for pain relief in active orthodontic treatment. Int. Orthod. 2020, 18, 684–695.
- Cronshaw, M.; Parker, S.; Anagnostaki, E.; Lynch, E. Systematic Review of Orthodontic Treatment Management with Photobiomodulation Therapy. Photobiomodul. Photomed. Laser Surg. 2019, 37, 862–868.
- Cambier, D.; Blom, K.; Witvrouw, E.; Ollevier, G.; De Muynck, M.; Vanderstraeten, G. The Influence of Low Intensity Infrared Laser Irradiation on Conduction Characteristics of Peripheral Nerve: A Randomised, Controlled, Double Blind Study on the Sural Nerve. Lasers Med. Sci. 2000, 15, 195–200.
- Hagiwara, S.; Iwasaka, H.; Okuda, K.; Noguchi, T. GaAlAs (830 nm) low-level laser enhances peripheral endogenous opioid an-algesia in rats. Lasers Surg. Med. 2007, 39, 797–802.
- Farzan, A.; Khaleghi, K. The Effectiveness of Low-Level Laser Therapy in Pain Induced by Orthodontic Separator Placement: A Systematic Review. J. Lasers Med. Sci. 2021, 12, e29.
- Al-Jewair, T.; Farsaii, A. Low-Level Laser Therapy May Reduce Pain Associated with Orthodontic Separator Placement. J. Evid. Based Dent. Pract. 2022, 22, 101752.
- Kaklamanos, E.G.; Makrygiannakis, M.A.; Athanasiou, A.E. Oral Health-Related Quality of Life throughout Treatment with Clear Aligners in Comparison to Conventional Metal Fixed Orthodontic Appliances: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 3537.
- Sipiyaruk, K.; Chintavalakorn, R.; Saengfai, N. The protocol of low-level laser therapy in orthodontic practice: A scoping review of literature. J. Int. Soc. Prev. Community Dent. 2022, 12, 267–286.
- Demirsoy, K.K.; Kurt, G. Use of Laser Systems in Orthodontics. Turk. J. Orthod. 2020, 33, 133–140.
- AlShahrani, I.; Togoo, R.A.; Hosmani, J.; Alhaizaey, A. Photobiomodulation in acceleration of orthodontic tooth movement: A systematic review and meta analysis. Complement. Ther. Med. 2019, 47, 102220.
- Huang, T.; Wang, Z.; Li, J. Efficiency of photobiomodulation on accelerating the tooth movement in the alignment phase of orthodontic treatment—A systematic review and meta-analysis. Heliyon 2023, 9, e13220.
- Olmedo-Hernández, O.L.; Mota-Rodríguez, A.N.; Torres-Rosas, R.; Argueta-Figueroa, L. Effect of the photobiomodulation for acceleration of the orthodontic tooth movement: A systematic review and meta-analysis. Lasers Med. Sci. 2022, 37, 2323–2341.
- Yavagal, C.M.; Matondkar, S.P.; Yavagal, P.C. Efficacy of Laser Photobiomodulation in Accelerating Orthodontic Tooth Movement in Children: A Systematic Review with Meta-analysis. Int. J. Clin. Pediatr. Dent. 2021, 14 (Suppl. S1), S94–S100.
- Li, J.; Ge, X.; Guan, H.; Jia, L.; Chang, W.; Ma, W. The Effectiveness of Photobiomodulation on Accelerating Tooth Movement in Orthodontics: A Systematic Review and Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2021, 39, 232–244.
- Jedliński, M.; Romeo, U.; del Vecchio, A.; Palaia, G.; Galluccio, G. Comparison of the Effects of Photobiomodulation with Different Lasers on Orthodontic Movement and Reduction of the Treatment Time with Fixed Appliances in Novel Scientific Reports: A Systematic Review with Meta-Analysis. Photobiomodul. Photomed. Laser Surg. 2020, 38, 455–465.
- Bakdach, W.M.; Hadad, R. Effectiveness of low-level laser therapy in accelerating the orthodontic tooth movement: A systematic review and meta-analysis. Dent. Med. Probl. 2020, 57, 73–94.
- Ghaffar, Y.K.A.; El Sharaby, F.A.; Negm, I.M. Effect of low-level laser therapy on the time needed for leveling and alignment of mandibular anterior crowding. Angle Orthod. 2022, 92, 478–486.
- Zheng, J.; Yang, K. Clinical research: Low-level laser therapy in accelerating orthodontic tooth movement. BMC Oral Health 2021, 21, 324.
- Bastos, R.T.D.R.M.; Blagitz, M.N.; Aragón, M.L.S.D.C.; Maia, L.C.; Normando, D. Periodontal side effects of rapid and slow maxillary expansion: A systematic review. Angle Orthod. 2019, 89, 651–660.
- Saito, S.; Shimizu, N. Stimulatory effects of low-power laser irradiation on bone regeneration in midpalatal suture during ex-pansion in the rat. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 525–532.
- Sasaki, A.; Touma, Y.; Ishino, Y.; Tanaka, E.; Aoyama, J.; Hanaoka, K.; Watanabe, M.; Tanne, K. Linear polarized near-infrared irradiation stimulates mechanical expansion of the rat sagittal suture. Luminescence 2003, 18, 58–60.
- Cepera, F.; Torres, F.C.; Scanavini, M.A.; Paranhos, L.R.; Filho, L.C.; Cardoso, M.A.; Siqueira, D.C.; Siqueira, D.F. Effect of a low-level laser on bone regeneration after rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 444–450.
- Farzan, A.; Khaleghi, K.; Pirayesh, Z. Effect of Low-Level Laser Therapy on Bone Formation in Rapid Palatal Expansion: A Systematic Review. J. Lasers Med. Sci. 2022, 13, e13.
- Lai, P.-S.; Fierro, C.; Bravo, L.; Perez-Flores, A. Benefits of Using Low-level Laser Therapy in the Rapid Maxillary Expansion: A Systematic Review. Int. J. Clin. Pediatr. Dent. 2021, 14 (Suppl. S1), S101–S106.
- Davoudi, A.; Amrolahi, M.; Khaki, H. Effects of laser therapy on patients who underwent rapid maxillary expansion; a systematic review. Lasers Med. Sci. 2018, 33, 1387–1395.
- Albertini, R.; Villaverde, A.; Aimbire, F.; Salgado, M.; Bjordal, J.; Alves, L.; Munin, E.; Costa, M. Anti-inflammatory effects of low-level laser therapy (LLLT) with two different red wavelengths (660 nm and 684 nm) in carrageenan-induced rat paw edema. J. Photochem. Photobiol. B Biol. 2007, 89, 50–55.
- Muniz, X.C.; de Assis, A.C.C.; de Oliveira, B.S.A.; Ferreira, L.F.R.; Bilal, M.; Iqbal, H.M.N.; Soriano, R.N. Efficacy of low-level laser therapy in nerve injury repair—A new era in therapeutic agents and regenerative treatments. Neurol. Sci. 2021, 42, 4029–4043.
- Eshghpour, M.; Ahrari, F.; Takallu, M. Is Low-Level Laser Therapy Effective in the Management of Pain and Swelling After Mandibular Third Molar Surgery? J. Oral Maxillofac. Surg. 2016, 74, 1322.e1–1322.e8.
- Camacho, A.D.; Velásquez, S.A.; Marulanda, N.J.B.; Moreno, M. Photobiomodulation as oedema adjuvant in post-orthognathic surgery patients: A randomized clinical trial. Int. Orthod. 2020, 18, 69–78.
- Feslihan, E.; Eroğlu, C.N. Can Photobiomodulation Therapy Be an Alternative to Methylprednisolone in Reducing Pain, Swelling, and Trismus After Removal of Impacted Third Molars? Photobiomodul. Photomed. Laser Surg. 2019, 37, 700–705.
- de Barros, D.D.; Catão, J.S.d.S.B.; Ferreira, A.C.D.; Simões, T.M.S.; Almeida, R.D.A.C.; Catão, M.H.C.D.V. Low-level laser therapy is effective in controlling postoperative pain in lower third molar extractions: A systematic review and meta-analysis. Lasers Med. Sci. 2022, 37, 2363–2377, Erratum in Lasers Med. Sci. 2022.
- de Oliveira, F.J.D.; Brasil, G.M.L.C.; Soares, G.P.A.; Paiva, D.F.F.; Júnior, F.D.A.D.S. Use of low-level laser therapy to reduce postoperative pain, edema, and trismus following third molar surgery: A systematic review and meta-analysis. J. Cranio-Maxillofac. Surg. 2021, 49, 1088–1096.
- Hakimiha, N.; Bassir, S.H.; Romanos, G.E.; Shamshiri, A.R.; Moslemi, N. Efficacy of photobiomodulation therapy on neurosensory recovery in patients with inferior alveolar nerve injury following oral surgical procedures: A systematic review. Quintessence Int. 2021, 52, 140–153.
- Hosseinpour, S.; Tunér, J.; Fekrazad, R. Photobiomodulation in Oral Surgery: A Review. Photobiomodul. Photomed. Laser Surg. 2019, 37, 814–825.
- Ren, Y.; Jongsma, M.A.; Mei, L.; Van Der Mei, H.C.; Busscher, H.J. Orthodontic treatment with fixed appliances and biofilm formation—A potential public health threat? Clin. Oral Investig. 2014, 18, 1711–1718.
- Ozog, D.M.; Rkein, A.M.; Fabi, S.G.; Gold, M.H.; Goldman, M.P.; Lowe, N.J.; Martin, G.M.; Munavalli, G.S. Photodynamic Therapy: A Clinical Consensus Guide. Dermatol. Surg. 2016, 42, 804–827, Erratum in Dermatol. Surg. 2017, 43, 319.
- Olek, M.; Machorowska-Pieniążek, A.; Stós, W.; Kalukin, J.; Bartusik-Aebisher, D.; Aebisher, D.; Cieślar, G.; Kawczyk-Krupka, A. Photodynamic Therapy in Orthodontics: A Literature Review. Pharmaceutics 2021, 13, 720.
- Baeshen, H.A.; Alshahrani, A.; Kamran, M.A.; Alnazeh, A.A.; Alhaizaey, A.; Alshahrani, I. Effectiveness of antimicrobial photodynamic therapy in restoring clinical, microbial, proinflammatory cytokines and pain scores in adolescent patients having generalized gingivitis and undergoing fixed orthodontic treatment. Photodiagn. Photodyn. Ther. 2020, 32, 101998.
- Alshahrani, A.A.; Alhaizaey, A.; Kamran, M.A.; Alshahrani, I. Efficacy of antimicrobial photodynamic therapy against halitosis in adolescent patients undergoing orthodontic treatment. Photodiagn. Photodyn. Ther. 2020, 32, 102019.
- Eduardo, C.D.P.; Aranha, A.C.C.; Simões, A.; Bello-Silva, M.S.; Ramalho, K.M.; Esteves-Oliveira, M.; de Freitas, P.M.; Marotti, J.; Tunér, J. Laser treatment of recurrent herpes labialis: A literature review. Lasers Med. Sci. 2014, 29, 1517–1529.
- Zanella, P.A.; Onuchic, L.F.; Watanabe, E.H.; Azevedo, L.H.; Aranha, A.C.C.; Ramalho, K.M.; Eduardo, C.D.P. Photobiomodulation for Preventive Therapy of Recurrent Herpes Labialis: A 2-Year In Vivo Randomized Controlled Study. Photobiomodul. Photomed. Laser Surg. 2022, 40, 682–690.
- Woźniak, A.; Matys, J.; Grzech-Leśniak, K. Effectiveness of lasers and aPDT in elimination of intraoral halitosis: A systematic review based on clinical trials. Lasers Med. Sci. 2022, 37, 3403–3411.
- Ferrisse, T.M.; Dias, L.M.; de Oliveira, A.B.; Jordão, C.C.; Mima, E.G.D.O.; Pavarina, A.C. Efficacy of curcumin-mediated antibacterial photodynamic therapy for oral antisepsis: A systematic review and network meta-analysis of randomized clinical trials. Photodiagn. Photodyn. Ther. 2022, 39, 102876.
- Sales, L.S.; Miranda, M.L.; de Oliveira, A.B.; Ferrisse, T.M.; Fontana, C.R.; Milward, M.; Brighenti, F.L. Effect of the technique of photodynamic therapy against the main microorganisms responsible for periodontitis: A systematic review of in-vitro studies. Arch. Oral Biol. 2022, 138, 105425.
- Al-Shammery, D.; Michelogiannakis, D.; Ahmed, Z.U.; Ahmed, H.B.; Rossouw, P.E.; Romanos, G.E.; Javed, F. Scope of antimicrobial photodynamic therapy in Orthodontics and related research: A review. Photodiagn. Photodyn. Ther. 2019, 25, 456–459.
- Ahmed, A.; Fida, M.; Javed, F.; Maaz, M.; Ali, U.S. Soft tissue lasers: An innovative tool enhancing treatment outcomes in orthodontics—A narrative review. J. Pak. Med. Assoc. 2023, 73, 346–351.
- Sarver, D.M. Use of the 810 nm diode laser: Soft tissue management and orthodontic applications of innovative technology. Pract. Proced. Aesthetic Dent. PPAD 2006, 18, suppl 7–13.
- Inchingolo, A.M.; Malcangi, G.; Ferrara, I.; Viapiano, F.; Netti, A.; Buongiorno, S.; Latini, G.; Azzollini, D.; De Leonardis, N.; de Ruvo, E.; et al. Laser Surgical Approach of Upper Labial Frenulum: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 1302.
- Sadiq, M.S.K.; Maqsood, A.; Akhter, F.; Alam, M.K.; Abbasi, M.S.; Minallah, S.; Vohra, F.; Alswairki, H.J.; Abutayyem, H.; Mussallam, S.; et al. The Effectiveness of Lasers in Treatment of Oral Mucocele in Pediatric Patients: A Systematic Review. Materials 2022, 15, 2452.
- Khosraviani, F.; Ehsani, S.; Fathi, M.; Saberi-Demneh, A. Therapeutic effect of laser on pediatric oral soft tissue problems: A systematic literature review. Lasers Med. Sci. 2019, 34, 1735–1746.
- Bornstein, E.S.; Lomke, M.A. The safety and effectiveness of dental Er:YAG lasers. A literature review with specific reference to bone. Dent. Today 2003, 22, 129–133.
- Ahn, J.H.; Power, S.; Thickett, E. Application of the diode laser for soft-tissue surgery in orthodontics: Case series. J. Orthod. 2021, 48, 82–87.
- Dumbryte, I.; Vebriene, J.; Linkeviciene, L.; Malinauskas, M. Enamel microcracks in the form of tooth damage during orthodontic debonding: A systematic review and meta-analysis of in vitro studies. Eur. J. Orthod. 2018, 40, 636–648.
- Ghazanfari, R.; Nokhbatolfoghahaei, H.; Alikhasi, M. Laser-Aided Ceramic Bracket Debonding: A Comprehensive Review. J. Lasers Med. Sci. 2016, 7, 2–11.
- Stein, S.; Wenzler, J.; Hellak, A.; Schauseil, M.; Korbmacher-Steiner, H.; Braun, A. Intrapulpal Temperature Increases Caused by 445-nm Diode Laser-Assisted Debonding of Self-Ligating Ceramic Brackets During Simulated Pulpal Fluid Circulation. Photomed. Laser Surg. 2018, 36, 185–190.
- Hoteit, M.; Nammour, S.; Zeinoun, T. Evaluation of Enamel Topography after Debonding Orthodontic Ceramic Brackets by Different Er,Cr:YSGG and Er:YAG Lasers Settings. Dent. J. 2020, 8, 6.
- Mesaroș, A.; Mesaroș, M.; Buduru, S. Orthodontic Bracket Removal Using LASER-Technology—A Short Systematic Literature Review of the Past 30 Years. Materials 2022, 15, 548.
- Ajwa, N.; Alfayez, H.; Al-Oqab, H.; Melibary, R.; Alzamil, Y. The Effect of Erbium-Doped Yttrium Aluminum Garnet Laser in Debonding of Orthodontic Brackets: A Systematic Review of the Literature. Photobiomodul. Photomed. Laser Surg. 2021, 39, 725–733.
- Francisco, I.; Travassos, R.; Nunes, C.; Ribeiro, M.; Marques, F.; Pereira, F.; Marto, C.M.; Carrilho, E.; Oliveiros, B.; Paula, A.B.; et al. What Is the Most Effective Technique for Bonding Brackets on Ceramic—A Systematic Review and Meta-Analysis. Bioengineering 2022, 9, 14.
