Lung transplantation is often the only viable treatment option for a patient with end-stage lung disease. Lung transplant results have improved substantially over time, but ischemia-reperfusion injury, primary graft dysfunction, acute rejection, and chronic lung allograft dysfunction (CLAD) continue to be significant problems. Mesenchymal stromal cells (MSC) are pluripotent cells that have anti-inflammatory and protective paracrine effects and may be beneficial in solid organ transplantation.
1. Introduction
Lung transplantation is standard therapy for various end-stage lung diseases such as interstitial lung disease, obstructive lung disease, pulmonary hypertension, and cystic fibrosis. Almost 5000 lung transplants are reported annually in the International Society of Heart and Lung Transplantation Registry, and the results have improved over time [
1]. However, the median survival of lung transplant recipients is limited to less than 7 years, and the main obstacles are primary graft dysfunction (PGD), acute rejection, chronic lung allograft dysfunction (CLAD), and side-effects of immunosuppressive drugs [
2,
3,
4,
5].
Mesenchymal stromal cells (MSC) are pluripotent cells present in most adult tissues [
6,
7]. MSC therapy in solid organ transplantation has gained attraction as MSCs possess anti-inflammatory, immunomodulatory, and protective features that could theoretically be utilized to counteract non-immunological and immunological injuries related to organ transplantation [
8,
9]. In lung transplantation, MSCs have been delivered in experimental studies to the donor lung to protect the transplant against ischemia-reperfusion injury (IRI) and PGD and to induce immunomodulatory effects [
10]. In addition, small Phase 1 clinical trials have been performed in lung transplant patients with established CLAD [
11,
12,
13], and additional clinical PGD and CLAD trials are ongoing [
14].
2. Mesenchymal Stromal Cells
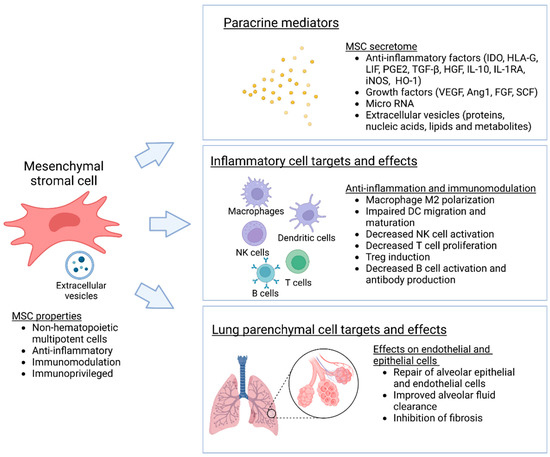
Mesenchymal stromal cells (MSC) and multipotent adult progenitor cells (MAPC) are mesenchymal, non-hematopoietic progenitor cells that are found in most tissues and are capable of self-renewal and differentiation into various types of stromal cells (
Figure 1). Resident MSCs are also present in the lung, localized in perivascular spaces, where they act as important regulators of pulmonary homeostasis and the balance between lung injury and repair [
18]. For therapeutic purposes, MSCs are commonly isolated from bone marrow, adipose tissue, the umbilical cord, and the placenta [
6,
7]. As considerable heterogeneity in cell sources, and isolation and expansion methods exist, the International Society for Cell Therapy has recommended minimal standard criteria to identify and characterize MSCs. Accordingly, MSCs should adhere to plastic in standard culture conditions, express typical stromal cell surface markers, lack expression of hematopoietic markers, and differentiate into osteoblasts, adipocytes, and chondroblasts in vitro under appropriate conditions [
19]. While MAPCs resemble MCSs, they are biologically more primitive and have greater differentiation potential than classical MSCs [
20].
Figure 1. Biological properties and effects of mesenchymal stromal cells. MSC are non-hematopoietic multipotent cells that have anti-inflammatory, immunomodulatory and protective effects mainly mediated though paracrine mechanisms.
Initially, MSCs and MAPCs were considered to result in cell replacement and renewal of damaged tissues; however, the current view is that the therapeutic effects of these cells are largely mediated by paracrine signaling, through the secretion of numerous soluble mediators, including growth factors, cytokines, and microRNA. This MSC secretome is considered to modulate inflammation and immune responses, and to stimulate innate tissue repair [
6,
21]. MSC therapies have been investigated in numerous clinical trials of cardiovascular disease, graft-versus host disease, and neurological disease, but the success has so far been variable [
7]. Several studies have also examined the use of MSC in lung disease, especially in acute respiratory distress syndrome (ARDS) [
22,
23].
3. Lung Transplant MSC Therapy
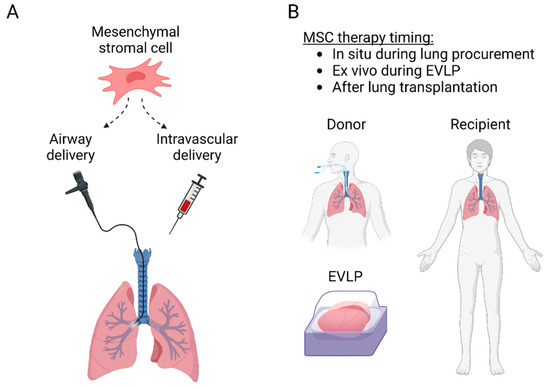
The protective anti-inflammatory and immunomodulatory properties make MSCs attractive therapeutic candidates for lung transplantation. MSCs have been delivered to the lungs through the airways or intravascularly and can be administered into the donor lung either before transplantation or to the recipient before or after transplantation (
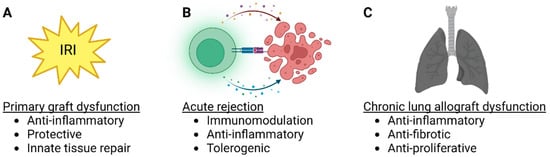
Figure 2). Most of the preclinical studies have used MSCs to inhibit IRI, while some experiments have targeted acute rejection, and some clinical trials have explored MSC therapy in patients with CLAD (
Table 1). Importantly, there is significant interaction between IRI, acute rejection, and CLAD (
Figure 3), as lung injury may trigger alloimmune responses, and various non-immunological and immunological factors participate in the development of CLAD [
5,
42].
Figure 2. (A) MSC delivery routes to the lung transplant. MSC can be administered into the lungs through the airways with a flexible bronchoscope or intravascularly either intravenously, or directly through the pulmonary artery. (B) MSC administration can be performed before transplantation in situ in the donor or ex vivo during ex vivo lung perfusion, or after transplantation to the recipient.
Figure 3. MSC therapy targets in lung transplantation. (A) Lung transplant ischemia-reperfusion injury and primary graft dysfunction, (B) acute rejection and (C) chronic lung allograft dysfunction (CLAD) are potential targets for MSC therapy. In each lung transplant pathology, possible beneficial effects of MSCs are listed.
Table 1. Lung transplant and EVLP studies with MSCs.
|
Target
|
Species
|
Model
|
MSC
|
Administration
|
Effect
|
Ref
|
|
IRI
|
Rat
|
Lung hilar clamping
|
Engineered BM-MSC (MSC-vIL-10)
|
Intravenous
|
Improved oxygenation, inflammation and permeability
|
[43]
|
|
IRI
|
Pig
|
SLTx
|
BM-MSC
|
Pulmonary artery vs. endobronchial
|
Endobronchial MSC delivery improved lung compliance
|
[44]
|
|
IRI
|
Human
|
EVLP
|
MAPC
|
Airways
|
Decreased edema and inflammation
|
[45]
|
|
IRI
|
Human
|
EVLP
|
BM-MSC
|
Intravascular
|
Restored alveolar fluid clearance
|
[46]
|
|
IRI
|
Mouse
|
SLTx
|
BM-MSC
|
Recipient intravenous
|
Decreased IRI, MSC homing preferentially into the lung transplant
|
[47]
|
|
IRI
|
Pig
|
EVLP
|
UC-MSC
|
Airway vs. intravascular, 3 different doses
|
Intravascular delivery improved MSC lung retention, optimal dose 150 × 106 MSC decreased IL-8 and increased VEGF
|
[48]
|
|
IRI
|
Mouse
|
SLTx
|
BM-MSC
|
Ex vivo pulmonary artery
|
Decreased IRI
|
[49]
|
|
IRI
|
Pig
|
SLTx
|
BM-MSC
|
Pulmonary artery vs. endobronchial
|
No short-term differences detected
|
[50]
|
|
IRI
|
Mouse
|
Lung hilar clamping and EVLP
|
Human UC-MSC vs. MSC-EVs
|
Intravascular
|
MSCs and MSC-EVs attenuate IRI
|
[51]
|
|
IRI
|
Human
|
EVLP
|
MAPC
|
Airways
|
Decreased BAL neutrophilia, TNF-α, IL-1β and IFN-γ
|
[52]
|
|
IRI
|
Pig
|
SLTx
|
BM-MSC
|
Intravenous or intrabronchial
|
Heterogenous localization, in alveoli after endobronchial and in blood vessels after intravascular administration
|
[53]
|
|
IRI
|
Rat
|
SLTx
|
BM-MSC
|
Intravenous
|
Protection against IRI
|
[54]
|
|
IRI
|
Pig
|
EVLP and SLTx
|
UC-MSC
|
Intravascular
|
Decreased IRI during EVLP and after TX
|
[55]
|
|
IRI
|
Rat
|
EVLP
|
UC-MSC
|
Intravascular
|
Improved inflammation and IRI
|
[56]
|
|
IRI
|
Rat
|
EVLP
|
BM-MSC-EVs
|
Intravascular
|
Multiple influences on pulmonary energetics, tissue integrity and gene expression
|
[30]
|
|
IRI
|
Human
|
EVLP
|
Engineered UC-MSC (MSCIL−10)
|
Intravascular
|
Safe and feasible, results in rapid IL-10 elevation
|
[40]
|
|
IRI
|
Rat
|
SLTx
|
Donor vs. recipient adipose tissue MSC
|
Intravenous
|
MSCs, regardless of their origin, exert similar immunosuppressive effects
|
[57]
|
|
IRI/
ARDS
|
Human
|
EVLP/endotoxin
|
BM-MSC
|
Airways
|
Restored alveolar fluid clearance
|
[58]
|
|
IRI/
ARDS
|
Human
|
EVLP/e.coli pneumonia
|
BM-MSC
|
Airways
|
Restored alveolar fluid clearance, reduced inflammation and increased antimicrobial activity
|
[59]
|
|
Acute rejection
|
Rat
|
SLTx
|
BM-MSC
|
1 vs. 2 recipient intravenous doses
|
Protection from acute rejection, best result with 2 recipient doses
|
[60]
|
|
Acute rejection/
CLAD
|
Mouse
|
Ortotopic tracheal Tx
|
iPSC-MSC
|
Intravascular
|
Induces immune tolerance and supports long-term graft survival
|
[61]
|
|
CLAD
|
Mouse
|
Heterotopic tracheal Tx
|
MSC (various sources)
|
Intravenous
|
Prevents airway occlusion
|
[62]
|
|
CLAD
|
Mouse
|
Ortotopic tracheal Tx
|
BM-MSC
|
Intravenous
|
Prevents airway occlusion through macrophage cytokines
|
[63]
|
|
CLAD
|
Mouse
|
Heterotopic tracheal Tx
|
BM-MSC
|
Local vs. systemic vs. combination
|
Prevents airway occlusion through modulation of immune response, best effect with combination treatment
|
[64]
|
|
CLAD
|
Human
|
Clinical Tx
|
BM-MSC
|
Intravenous twice weekly for 2 weeks
|
Safe and feasible in patients with advanced CLAD
|
[13]
|
|
CLAD
|
Human
|
Clinical Tx
|
BM-MSC
|
Intravenous
|
Safe and feasible in patients with moderate CLAD
|
[12]
|
|
CLAD
|
Human
|
Clinical Tx
|
BM-MSC
|
Intravenous
|
Well tolerated in moderate-to-severe CLAD, low-dose may slow progression of CLAD in some patients
|
[11]
|
4. Strategies to Improve MSC Delivery and Therapeutic Potential
Although the lung is well accessible for MSC therapy with either airway or intravenous in vivo administration, cell delivery into an isolated donor lung during ex vivo lung perfusion (EVLP) would have several advantages.
4.1. MSC Delivery into the Donor Lung during EVLP
In EVLP, the isolated donor lung is perfused and ventilated in normothermia ex vivo (outside the body), enabling confirmation of donor lung quality before transplantation. This has revolutionized lung transplantation, as marginal donor lungs that would otherwise have been rejected from transplantation can be tested and transplanted if graft function is adequate [
93]. A landmark clinical study evaluated high-risk donor lungs during EVLP and established that transplantation of lungs that were physiologically stable during 4 h of EVLP leads to post-transplant results similar to those obtained with conventionally selected lungs [
94]. EVLP has safely and significantly increased the available pool of donor organs for transplantation, and later studies have shown that medium- and long-term lung transplant results remain excellent after EVLP evaluation [
95,
96].
EVLP has been used as a platform for cell therapy in several experimental studies using airway or intravascular delivery (
Table 1). Mordant et al. compared different MSC doses and administration routes during pig lung EVLP. Intravascular administration resulted in better MSC retention in the lung, and most of the MSCs engraftment occurred within the first minutes after pulmonary artery injection [
48]. Moreover, comparison of three different doses revealed that intravascular administration of 150 × 10
6 MSCs, the middle dose of the experiment, improved lung oxygenation and compliance. In contrast, a higher 300 × 10
6 MSCs dose temporarily increased pulmonary vascular resistance [
48], possibly related to clustering of the cells into the lung microvasculature. These results highlight the efficacy of intravascular MSC delivery but also indicate that high cell doses may result in adverse embolic effects [
48]. Interestingly, the optimal cell dose (150 × 10
6 MSCs; 5 × 10
6 per kg of animal weight) is close to the doses used in the clinical MSC CLAD studies [
11,
13,
70]. In the studies administering MSCs during EVLP, decreased proinflammatory cytokine levels and protection of the alveolar-epithelial barrier function during ischemia- or endotoxin-induced lung injury have been observed [
45,
46,
48,
52,
55,
58,
59]. Several studies have also reported that administration of MSC-derived EVs protects against lung injury [
29,
30].
4.2. Genetically Engineered MSCs
Genetic engineering of cell-based therapeutics with viral and non-viral vectors has been used to achieve modified cells with enhanced therapeutic properties. Genetic engineering modulates the MSC secretome and aims, for example, to enhance MSC migration to target sites, facilitate intrinsic repair properties, improve cell survival, or change MSCs into gene delivery vehicles [
16].
Several different genetically modified MSCs have been studied in lung injury models, and for example, MSC engineered to produce anti-inflammatory IL-10 have been beneficial in lung IRI, endotoxemia, and ARDS [
43,
97,
98]. In our recent study, we transduced human umbilical cord-derived MSC with adenoviral vectors encoding IL-10 and administered these pre-modified and cryopreserved MSC
IL−10 cells during EVLP to human lungs rejected from clinical transplantation. This rapidly elevated EVLP perfusate IL-10 levels in minutes, MSC
IL−10 cells were retained in the lung, and IL-10 was increased also in lung tissue and the airway compartment [
40]. While possible therapeutic or immunomodulatory effects of MSC
IL−10 therapy are not known yet, these results indicate that therapy with genetically modified cells during standard clinical EVLP is feasible.
This entry is adapted from the peer-reviewed paper 10.3390/bioengineering10060728