Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Anesthesiology
Parkinson’s disease (PD) is the second most common inflammatory neurodegenerative disorder after dementia. Preclinical and epidemiological data strongly suggest that chronic neuroinflammation slowly induces neuronal dysfunction. Activated microglia secrete several neurotoxic substances, such as chemokines and proinflammatory cytokines, which may promote blood–brain barrier (BBB) permeabilization.
- Parkinson’s disease
- inflammatory biomarkers
- surgery
1. Introduction
Parkinson’s disease (PD) is the second most common inflammatory neurodegenerative disorder after dementia, affecting 7–10 million people worldwide [1]. About 2–3% of elderly patients (aged ≥ 65 years) are affected by PD [2]. People with PD suffer motor symptoms such as bradykinesia, rigidity, resting tremor, and postural instability. In addition, patients often complain of ‘non-motor symptoms’ such as cognitive impairment, anxiety, depression, hypothermia, constipation, bowel and rapid eye movement sleep behavior disorder, and autonomic nervous system disorders [2,3].
PD is characterized by the progressive loss of dopaminergic neurons in the substantia nigra pars compacta, the appearance of Lewy bodies (intracellular inclusions of aggregated a-synuclein), and the presence of neuroinflammation [4,5,6,7]. Although the mechanism of neuron loss in PD is unclear, inflammation and the peripheral immune system play key roles [7,8,9]. Preclinical and epidemiological data suggest that chronic neuroinflammation induces neuronal dysfunction during the asymptomatic stage of PD [6,10]. The activation of resident microglia precedes dopamine neuron loss [11,12]. Activated microglia secrete several neurotoxic substances, such as chemokines and proinflammatory cytokines, which may cause blood–brain barrier (BBB) permeabilization and subsequent infiltration of peripheral leukocytes into the central nervous system (CNS) [11,12,13].
There is currently no cure for PD to prevent PD or delay its progression, mainly due to the still limited comprehension of the events ultimately leading to neurodegeneration. Available treatments for PD are only symptomatic, aimed at relieving the loss of brain dopaminergic neurons by using levodopa (the dopamine precursor), some dopaminergic agonists, and other indirect dopaminergic agents. Surgery, including deep brain stimulation, may be considered in advanced PD patients who fail to respond to levodopa [14].
CD4+ T lymphocytes play a pivotal role in orchestrating immune responses implicated not only in the pathogenesis of inflammatory diseases, but also in host defense. CD4+ T cells include proinflammatory cells such as T helper (Th) 1 and Th17, and anti-inflammatory cells such as Th2 and T regulatory cells (Tregs) [15,16]. Interestingly, both animal models of PD and clinical studies suggest that Th1 and Th17 can be detrimental to dopamine neurons, whereas Th2 and Tregs are neuroprotective [17,18]. Indeed, the number of circulating CD4+ T cells is reduced in patients with PD [19], but the relative proportions and functional profiles of subdivided cell populations are controversial. The decrease in CD4+ T cells seen in the peripheral blood of patients with PD is mainly due to decreases in Th2, Th17, and Tregs [20,21]. As a result, Th1 T cells, the absolute numbers of which are similar to healthy controls, increase in PD patients compared to other T cells, resulting in a Th1 bias. Consequently, the production of IFN-γ and TNF-α by Th1 cell lineages increases [21]. The results of studies on the serum levels of cytokines such as IFN-γ and TNF-α secreted by Th1 T cells, IL-8 and IL-10 secreted by Th2 T cells, and IL-17 secreted by Th17 in PD patients are not uniform [19,22,23,24,25,26,27]. In addition, the relationships between serum cytokine levels and motor and non-motor symptoms of PD are controversial [19,23,26,27].
Surgical stress and anesthesia induce inflammatory responses by disturbing the balance between pro- and anti-inflammatory cytokines [28], which may exacerbate the neuroinflammatory response in PD patients. The effects of inhalational anesthetics on the inflammatory response are controversial [29,30,31,32]. Meanwhile, Shan et al. [33] reported that sevoflurane worsened the prognosis of PD in a Drosophila model. There are few studies on the effect of the immune response on PD symptoms and prognosis after surgery and anesthesia [34,35,36,37].
2. Blood Inflammatory Biomarkers in PD Patients
Only seven markers (CRP, IL-1β, IL-2, IL-6, IL-8, IFN-γ, TNF-α) were reported in more than 5 of 51 studies. The most frequently studied inflammatory biomarkers are CRP and IL-1β [26,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58]. These two biomarkers show consistently higher levels in PD patients than healthy controls. Data for IL-2, IL-6, IFN-γ, and TNF-α are controversial. Some studies report higher blood levels of these biomarkers, while others found no differences between PD patients and healthy controls, or lower levels in the former group [27,38,41,42,43,44,49,50,51,53,54,55,56,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Blood markers evaluated to date are listed in Table 1 and Figure 1.
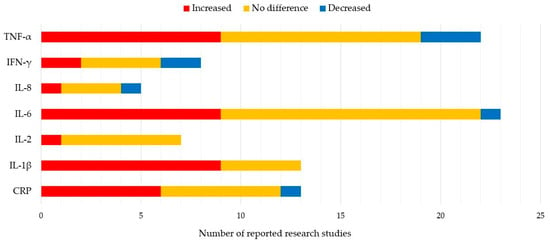
Figure 1. 7 Most reported blood biomarkers and their value relative to healthy controls.
Table 1. Blood biomarkers and their related symptoms.
| Clinical Trials | Blood Markers | Related Symptoms |
|---|---|---|
| Alrafiah et al. [55] | IL-1β, IL-6, TNF-α | |
| Andican et al. [39] | CRP, ICAM-1 | |
| Bagheri et al. [73] | CXCL 12, CXCR4 | |
| Baran et al. [46] | CRP, HMGB1 | |
| Brockmann et al. [52] | FABP, IL-10, IL-12p40, SCF, BDNF | |
| Calvani et al. [65] | MIP-1α, MIP-1β, IL-8, IL-9 | |
| Carvalho et al. [74] | S100B * | nonmotor |
| Chatterjee et al. [57] | IL-1β, NLRP3 | |
| Csencsits-Smith et al. [71] | MCP-1, IP-10, TNF-α | |
| Delgado-Alvarado et al. [62] | IL-6 * | motor, nonmotor |
| Dommershuijsen et al. [48] | CRP | |
| Dufek et al. [75] | IL-6 * | mortality |
| Dumitrescu et al. [76] | calprotectin | |
| Eidson et al. [69] | IL-8 *, IFN-γ, NGAL, TNF-α | motor, nonmotor |
| Fan et al. [58] | IL-1β *, NLRP3 | motor, nonmotor |
| Green et al. [77] | IL-6 *, IL-17A *, TNF-α, TGF-β | motor, nonmotor |
| Gupta et al. [78] | Fractakine *, 3-NT * | motor |
| Gupta et al. [27] | IL-8, TNF- α | |
| Herlofson et al. [79] | IL1-Ra *, VCAM-1 * | nonmotor |
| Hu et al. [50] | IL-1β, TNF-α | |
| Jin et al. [47] | CRP | |
| Karpenko et al. [53] | IL-1β, IL-1Ra, IL-6, IL-10 *, TNF-α * | nonmotor |
| Kim et al. [43] | CRP, IL-1β, IL-2, IL-6, IL-10 *, TNF-α | nonmotor |
| King et al. [44] | CRP, IL-2 *, IL-4, IL-6, IL-8, IL-10, IFN-γ, TNF-α | motor |
| Kouchaki et al. [72] | IL-27 *, TNF-α * | motor |
| Koziorowski et al. [49] | IL-1β, IL-6 *, IL-10, IL-12, TNF-α, NT-proCNP | motor |
| Kwiatek-Majkusiak et al. [63] | IL-6 | |
| Lerche et al. [80] | FABP *, TNF-α *, CA-125 *, BDNF* | motor, nonmotor |
| Lian et al. [56] | IL-1β, IL-6 * | motor |
| Lin et al. [66] | IL-1β, IL-2, IL-4, IL-6, IL-13, IL-18, IFN-γ, TNF-α | |
| Lindqvist et al. [26] | CRP, IL-6 *, sIL-2R, TNF-a | nonmotor |
| Mahlknecht et al. [59] | MCP-4, ICAM-1, IL-2, IL-6, Leptin, PDGF-BB, prolactin, RANTES | |
| Martin-Ruiz et al. [70] | CRP *, IL-6 *, IL-10, TNF-α | nonmotor |
| Miliukhina et al. [64] | MCP-1, IL-1β, IL-2, IL-4, IL-6, IL-10, IL-12, IL-13, IL-21, IL-23, INF-γ, TNF-α | |
| Milyukhina et al. [51] | IL-1β *, IL-6, IL-10 *, TNF-α * | nonmotor |
| Pereira et al. [81] | IL-6 * | nonmotor |
| Perner et al. [82] | VCAM-1 * | motor |
| Rathnayake et al. [67] | IL-10, IFN-γ, TNF-α | |
| Rocha et al. [54] | IL-1β, IL-2, IL-4, IL-6, IL-10, IL-17A, IFN-γ, TNF-α | |
| Rocha et al. [83] | sTNFR1 *, sTNFR2 * | nonmotor |
| Roy et al. [84] | NLRP3 | |
| Santos-Garcia et al. [45] | CRP* | motor |
| Sawada et al. [85] | CRP* | nonmotor |
| Schroder et al. [60] | IL-2, IL-4, IL-5, IL-6, IL-9, IL10, IL-13, IL-17A, IL-17F, IL-21, IL-22, IFN-γ, TNF-α, 1111, CCL17, CCL20, CXCL1, CXCL5, CXCL9, CXCL11, IL-8, IP-10, MCP-1, MIP-1α, MIP-1β, RANTES |
|
| Sun et al. [86] | C3 *, C4 | nonmotor |
| Tang et al. [61] | RANTES *, IL-6 * | motor |
| Ton et al. [38] | CRP, IL-6 | |
| Umemura et al. [87] | CRP * | motor |
| Usenko et al. [68] | MCP-1, IL-4, IL-6, IL-10*, INF-γ, TNF-α * | nonmotor |
| Vesely et al. [23] | C3 *, C4*, IL-6 * | nonmotor |
| Vesely et al. [88] | C3 * | nonmotor |
| Wang et al. [42] | CRP *, IL-1β, sIL-2R *, IL-6, IFN-γ, TNF-α* | nonmotor |
| Yang et al. [89] | IL-6, IL-10, IL-17, IL-23, TGF-β | |
| Yilmaz et al. [90] | IL-12p40 * | motor, nonmotor |
BDNF, brain-derived neurotrophic factor; C, complement; CA-125, cancer antigen 125; CCL, C-C motif chemokine; CRP, C-reactive protein; CXCL 12, C-X-C motif chemokine ligand 12; CXCR4, C-X-C chemokine receptor type 4; FABP, fatty acid-binding protein; HMGB1, high-mobility group box 1 protein; ICAM-1, intercellular adhesion molecule 1; IL1-Ra, interleukin-1 receptor antagonist; IP-10, interferon gamma-induced protein 10; IFN-γ, interferon gamma; MCP, monocyte chemoattractant protein-1; 3-NT, 3-nitrotyrosine; MIP, macrophage inflammatory protein; NGAL, neutrophil gelatinase associated lipocalin; NLRP3, NLR family pyrin domain containing 3; NT-proCNP, N-terminal pro c-type natriuretic peptide; PDGF-BB, platelet-derived growth factor-BB; RANTES, regulated upon activation, normal T-cell expressed and presumably secreted; S100B, S100 calcium binding protein B; SCF, stem cell factor; sIL-2R, soluble interleukin-2 receptors; sTNFR, soluble tumor necrosis factor receptors; TGF-β, transforming growth factor-beta; TNF-α, tumor necrosis factor alpha; VCAM-1, vascular cell adhesion protein 1; red colored, increased in Parkinson’s disease patients relative to healthy controls; blue colored, decreased in Parkinson’s disease patients relative to healthy controls; green colored, positively correlated with symptom; orange colored, negatively correlated with the symptom; *, significantly correlated with the symptom.
Although many studies have focused on proinflammatory profiles, inflammation is a balance between pro- and anti-inflammatory processes. CD4+ T lymphocytes orchestrate an effective immune response during host defense, as well as in the pathogenesis of inflammatory diseases. CD4+ T cells can select for proinflammatory phenotypes such as Th 1 and Th17 cells, as well as anti-inflammatory phenotypes such as Th2 and Tregs [15,16]. Results from animal models of PD and clinical studies suggest that Th1 and Th17 cells are detrimental to neurons, while Th2 and Tregs are neuroprotective [17,18].
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics13040693
This entry is offline, you can click here to edit this entry!
