Microalgae and cyanobacteria could represent a potential natural alternative to antibiotic, antiviral, or antimycotic therapies, as well as a good supplement for the prevention and co-adjuvant treatment of different oral diseases.
- microalgae
- Spirulina platensis
- Chlorella vulgaris
- oral health
- antimicrobial activity
- Streptococcus mutans
1. Introduction
Today, the majority of the bioactive peptides added in well-being promoting aliments, food supplements, pharmaceutic, and cosmetic formulations are realized by chemical production or by the partial digestion of proteins derived from animals. Therefore, they are not always well-regarded by the users due to the risks related to solvent contamination or the utilization of animal-derived ingredients. Alternatively, plant and microalgae-resulting peptides are recognized as selective, useful, nontoxic and well accepted when consumed, having a significant potentiality for utilization in functional aliments, drugs, and cosmetic products. Furthermore, due to the increasing issue of the antibiotic resistance against pathogenic bacteria, research has been targeted to exploring new antibacterial compounds derived from different natural environments [1][2][3][4]. Consequently, in recent years, growing scientific interest has been centered on the study of the bioactivity of extracts derived from plant species. In particular, the focus is on food plants included in the so-called traditional medicine [5][6][7][8]. For example, polyphenols derived from some edible plants drew attention as potential sources of agents that, among the wide range of health benefits, were shown to inhibit the bacterial growth of some oral pathogens[9][10]. A recent study on a large sample of vulnerary plants from Italian areas has identified a small number of extracts that could find application for the prevention of dental caries [11]: extracts of Camelia sinensis and Plantago lanceolata, rich in flavonoids, showed inhibitory activity against the species of cariogenic Streptococci [11][12].
Functional foods are arising as a dietary resource for preventing diseases. They can be defined as technologically developed ingredients explicating specific actions on human health. In the scenario of growing promising sources of functional foods and preventive drugs, cyanobacteria and microalgae are drawing global interest, due to their content of highly valuable substances [13][14]
Cyanobacteria and microalgae are respectively prokaryotic or eukaryotic microorganisms growing through oxygenic photosynthesis. Their energetic intake requires light, carbon dioxide, water, and nutrients with phosphorus and nitrogen as major nutrients, whereas the products of metabolic activity are primarily carbohydrates, along with a surprisingly high number of chemicals, some of which are known to be useful for humans [13].
Both cyanobacteria and microalgae are widely spread in freshwater and marine ecosystems as well as on terrestrial habitats and in a wide range of extreme environments, from hot springs to barren rocks of deserts. This flexibility makes them the major producers of biomass under sustainable conditions, since they do not deprive agriculture of sources, while allowing water recycling and lowering polluting gas emissions [15]. Moreover, cyanobacteria and microalgae bring the potential to be converted into a wide range of products of economic interest, such as biofuels, cosmetics, renewable chemicals and other valuable compounds[15], animal and human food, especially as sources of proteins, lipids, and phytochemicals (Figure 1) [16].
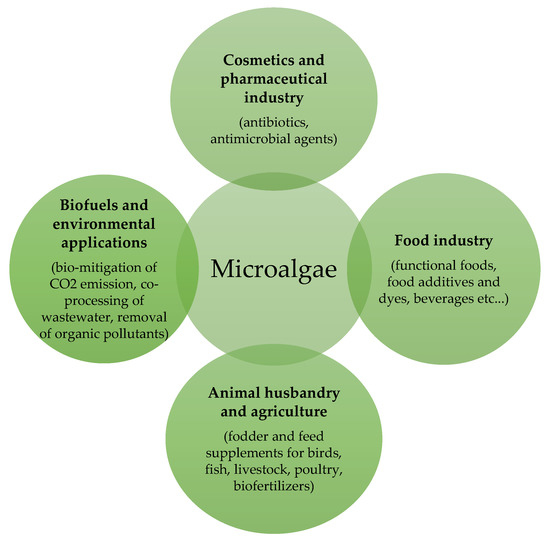
Figure 1. Application of microalgae in different fields.
2. Microalgal Effects on Oral Health
In the current scientific literature, there is still a lack of evidence about benefits derived from microalgal use in terms of treatment and the prevention of oral diseases. The collected studies mainly claim the potential role of Spirulina sp. in improving oral health.
2.1. Antiviral Activity
Herpes virus is a double-stranded DNA virus from the family of Herpesviridae. As its peculiarity, this virus does not leave the host after the first contact, settling in neural ganglion and causing a latent infection. This can take place in a variable time, depending on the type of virus and the host susceptibility. The causes that induce the reactivation of the viral activity can be temperature changes (hot/cold), traumas, fever, stress, and, above all, reduction of the host immunological response [17].
A study carried out in 2016 examined the antiviral activity of a defined S. platensis microalgal extract and of purified calcium spirulan (Ca-SP), which is a sulfated polysaccharide contained therein. Ca-SP inhibited HSV-1 infection in vitro with an effectiveness similar to that of acyclovir by blocking viral attachment and penetration into host cells. Ca-SP also impeded the entry of Kaposi sarcoma-associated herpesvirus/human herpes virus 8. Actually, in the experimental model of herpes exacerbation, the prophylactic activity of a cream containing Ca-SP and microalgae extract was greater than that of acyclovir cream. These results highlight a possible clinical use of Ca-SP containing Spirulina sp. extract for the prophylactic management of herpes labialis and indicate promising effects of Ca-SP against infections caused by other herpes viruses[18].
2.2. Oral Cancer Chemoprevention
Another interesting application for Spirulina sp. and, in particular, for the blue-green microalga S. platensis might be in oral cancer chemoprevention. Oral cancer represents 3% of all human carcinomas. Squamous cell carcinoma accounts for over 90% of the oral cancers, and others include adenocarcinoma derived from minor salivary gland, sarcoma, malignant lymphoma, and metastatic cancer. It shows a survival rate at 5 years of 51%, which is mainly due to late diagnosis in a clinical advanced stage. It is localized most frequently on the tongue, on the floor of the mouth, and on the cheek mucous, and it is mainly related to alcohol, smoking, and Human Papilloma Virus (HPV) infection [19]. Especially, smoke-related cancer is often preceded by some typical preneoplastic lesions, such as oral leucoplakia, erytroplakia, lichen planus, or persistent ulcers. Today, conventional therapy of potential pre-neoplastic conditions is mostly limited to mouth washes with antibacterial and antimycotic products in order to remove any superinfections, along with the elimination of risk factors, patient follow-up, and eventually, biopsy. On the other hand, the first choice for oral cancer treatment is still the surgical approach, causing inevitable esthetic and functional impairments [20]. Hence, there is a huge need to develop specific and less invasive strategies for oral cancer prevention and therapy.
Several experimental studies in animal models have demonstrated an inhibitory effect of S. platensis microalgae on oral carcinogenesis process. Some studies conducted on rats sustain that astaxanthin has significant preventive activities on 4-nitroquinoline-1-oxide (4-NQO)-induced tongue carcinogenesis [21]. In particular, after 8 weeks of treatment, the incidence of oral preneoplastic lesions and cell proliferation activity decreased significantly, and no oral neoplasms developed in rats fed with astaxanthin [22]. Grawish and his team carried out two experimental studies on hamsters (2008 and 2010) both aiming to investigate oral chemopreventive strategies using astaxanthin. In the first work, 30 male golden Syrian hamsters were divided into three groups: the first group had the right buccal pouch painted with 0.5% solution of 7,12-dimethylbenz[a]anthracene (DMBA), to the second group, 10 mg/daily S. platensis extract was administered, in addition to the same painting, and the last was a control group, not having painting nor S. platensis treatment. They observed moderate dysplastic changes extending into the midspinous layer in group one 7 weeks after DMBA painting, which reached half the thickness of the hyperplastic epithelium after 14 weeks. However, in group two, mild dysplastic changes were observed after 7 weeks, which were restricted to the basilar and parabasilar layers of the epithelium after 14 weeks of treatment. An overall significant difference among the three groups (p < 0.01) was indicated with one-way analysis of variance [23]. The second study from the same author confirmed these results. In particular, it focused on the proliferating cell nuclear antigen expression, showing that it was directly related to the severity of pathological alterations from normal epithelium to dysplasia and from dysplasia to squamous cell carcinoma in the study groups at the different extended periods of DMBA application and S. platensis extract administration [24].
S. platensis extracts, especially astaxanthin carotenoid, might have a big potential not only on precancerous lesions, but even on proper oral cancer. As in 1988, it was already proven that an extract of S. platensis–Dunaliella could inhibit tumor development in hamster buccal pouch [25], more recent data provided extensive evidence that dietary astaxanthin avoids the development and progression of hamster buccal pouch carcinomas through the inhibition of JAK-2/STAT-3 signaling and its downstream events [26].
Taking into account all these promising results, it can be concluded that S. platensis and, particularly, its most potent pigment, astaxanthin, plays a beneficial role in oral cancer regression and prevention, representing a potential valuable candidate for anti-cancer drug development.
2.3. Oral Antimicrobial Activity
Another property of cyanobacteria and microalgae that appears to be worthy of note for oral health implications is their antimicrobial activity. Among oral bacteria, Streptococcus mutans is a Gram-positive bacteria that is frequently found in the oral cavity’s normal flora and involved in the pathogenesis of caries [27][28]. Caries is the most common infective pathology worldwide, affecting especially that part of the population with a lower socio-economic status. It has a multifactorial pathogenesis, including diet and host susceptibility as co-factors together with the over-growing of S. mutans. S. aureus is also an abundant Gram-positive bacterium that has a strong connection with dental implant infections [29]. Enterococcus faecalis has been connected to oral infections, such as caries, endodontic infections, periodontitis, and peri-implantitis [30].
Fatty acid methyl esters (FAME) derived from lipids of microalgae are recognized as a suitable super-curator and superior anti-pathogenic. Experiments in 2018 assessed the effectiveness of FAME extracted from the microalga Scenedesmus intermedius as an antimicrobial agent against Gram-positive bacteria (S. aureus, S. mutans, and Bacillus cereus), Gram-negative bacteria (E. coli and P. aeruginosa), and fungi (Aspergillus parasiticus and C. albicans). FAME here analyzed displayed a solid antimicrobial effect at a lower MIC than those of recent reports. This result claimed that the FAME of S. intermedius has a potent antimicrobial and antioxidant activity and that it could find application as a powerful source against microbial diseases [31].
Microalgal extracts screened for their antimicrobial activities could be more effective than antibiotics and fungicides. An in vitro study in 2011 demonstrated the antimicrobial properties of Chaetoceros calcitrans, Skeletonema costatum, Chroococcus turgidus, and Nannochloropsis oceanica. Extracts exhibited inhibitory effects against S. aureus, S. pyogenes, and Bacillus subtilis. Antifungal activity was identified only in S. costatum and C. turgidus, but Aspergillus flavus and A. niger showed resistance to all the four microalgae. The highest in vitro inhibition zone was observed in acetone extract of Chlorococcum sp. against S. aureus and E. coli compared to other dried green microalgae extracts [32].
Another in vitro study in 2011 collected 46 species of freshwater cyanobacteria and selected five strains based on their growth characteristics, namely Oscillatoria latevirens, Phormidium corium, Lyngbya martensiana, Chrococcus minor, and Microcystis aeruginosa. The results clearly indicated that the acetone extracts of O. latevirens and ethanol extracts of P. corium gave the highest antimicrobial activity against S. aureus, S. mutans, and Micrococcus mutans and S. aureus, respectively. At the same time, the extract of L. martensiana had an antibacterial effect toward B. subtilis, S. aureus, and E. coli but negative effect toward S. mutans, M. mutans, and K. pneumoniae. In addition, O. latevirens, C. minor, and M. aeruginosa were shown to have antifungal activity on C. albicans. It was found that the effect of standard antibiotics was more than that of algal extracts on B. subtilis and E. coli. Meanwhile, the antibacterial potential of algal extracts on S. aureus, S. mutans, and M. mutans were even higher than those of standard antibiotics. The antimicrobial activity of these microalgae could be explained by presence of cyclic peptides, alkaloids, and lipopolysaccharides [33].
An investigation carried out in 2016 used S. platensis extract as a biomaterial for the biosynthesis of silver nanoparticles. Nanoparticles have unique biological and optical properties, which make them considered as efficient materials of the next technology generation with therapeutic and diagnostic applications. Metal nanoparticles are highly employed in a broad number of biomedical applications, especially as antimicrobials [34]. Silver ions and silver-based compounds are known bactericides, due to their large surface area that comes into contact with the microbial cells [35][36]. The application of nanoparticles in dentistry is of interest, as the oral cavity frequently comes across a superfluity of microorganisms. The results of the study suggest that the silver nanoparticles biosynthesized using S. platensis extract have good antibacterial activity against the three Gram-positive oral pathogens S. mutans, E. faecalis, and S. aureus [37].
2.4. Potential Effects in the Treatment of Periodontitis
Oral periodontitis is an inflammatory pathology affecting the supporting gum and bone tissues of the tooth. It is characterized by a cyclical evolution, alternating phases of quiescence with acute phases, which determines an irreversible loss of the clinical epithelium-connective attachment around the tooth and, as a consequence, progressive bone resorption [38]. Today, chronic periodontitis mostly requires three conventional treatment modalities: non-surgical techniques as scaling and root plaining, surgical conservative approaches for more compromised teeth and, ultimately, the extraction of hopeless teeth [39].
Several studies claim the potential clinical effectiveness of S. platensis for the treatment of oral periodontitis, which is probably due to its anti-inflammatory and antioxidant effects. Mahendra et al. in 2013 demonstrated that locally delivered S. platensis gel, along with scaling and root plaining, caused a beneficial impact in the treatment of chronic periodontitis. The efficacy of the product as a local drug delivery system in the non-surgical management of periodontitis without any side effects has been tested [40]. According to these findings, a recent pre-clinical study evaluated the effects of astaxanthin on alveolar bone loss and histopathological changes in ligature-induced periodontitis in rats. It can be suggested that astaxanthin administration may reduce alveolar bone loss by enhancing osteoblastic activity and decreasing osteoclastic action in an experimental periodontitis model [41]. The suppression effect of astaxanthin on bone loss is confirmed by Hwang et al. (2018), who studied the anti-osteoporotic effect of astaxanthin on bone mass in ovariectomized mice and its possible mechanism of action. The administration of astaxanthin (5, 10 mg/kg) for six weeks suppressed the enhancement of serum calcium, inorganic phosphorus, alkaline phosphatase, total cholesterol, and tartrate-resistant acid phosphatase activity. The bone mineral density and bone microarchitecture were improved by astaxanthin exposure [42].
Furthermore, in 2016, a study evaluated the effects of another microalgal carotenoid, fucoxanthin, on alveolar bone resorption in rats with periodontitis. Systemic fucoxanthin treatment resulted in a small reduction in tumor necrosis factor-α, interleukin-1β, and interleukin-6 levels and a significant reduction in oxidative stress index. It was noted that fucoxanthin induced a significant decrease in receptor activator of nuclear factor kappa-β ligand (RANKL) levels and a statistically non-significant elevation in osteoprotegerin and bone–alkaline phosphatase levels. There were no significant differences in alveolar bone loss levels between the case and control groups. Hence, according to this experimental study, fucoxanthin determines a limited decrease in alveolar bone resorption in rats with periodontitis [43].
Eventually, a recent work in 2018 analyzed the effects of a cyanobacterial component on the inflammation process induced by Phorphyromonas gingivalis, which is a Gram-negative bacterium co-responsible for oral periodontitis. Lipopolysaccharide (LPS) from P. gingivalis (Pg-LPS) is a key bacterial structure involved in the maintenance of a chronic pro-inflammatory environment during periodontitis. Similar to other Gram-negative LPS, Pg-LPS induces the release of pro-inflammatory cytokines through interaction with Toll-Like Receptor 4 (TLR4) and is able to stimulate negative TLR4 regulatory pathways, such as those involving microRNA (miRNA). In this work, the authors employed CyP, an LPS with TLR4-MD2 antagonist activity obtained from the cyanobacterium Oscillatoria planktothrix FP1, to study the effects on pro-inflammatory cytokine production and miRNA expression in human monocytic THP-1 cells stimulated with Pg-LPS. The results showed that CyP inhibited TNF-α, IL-1β, and IL-8 expression [44]. These outcomes could open new perspectives for innovative therapeutic approaches based on microalgal and cyanobacterial extracts for the treatment of oral periodontitis.
2.5. Control of Oral Submucous Fibrosis
A new horizon in S. platensis use can be in the management of an insidious and disabling disease affecting oral mucosa, such as Oral Submucous Fibrosis (OSMF). OSMF is a chronic progressive pathology that alters the flexibility of oral mucosa, ending in lockjaw and a higher risk of developing squamous oral cancer. It is a common condition in India and southeastern Asia, while it is infrequent in other parts of the world [45]. The results of trials of many treatment options, such as medical, physical, or surgical interventions, have suggested that combined therapies give better outcomes. A study conducted in 2019 intended to assess the effectiveness of S. platensis together with different physiotherapeutic approaches in the treatment of OSMF. After administration of S. platensis 500 mg twice a day for 3 months, all subjects have reported statistically significant amelioration in burning perception, mouth opening, tongue protrusion, and cheek flexibility. Moreover, S. platensis did not cause any considerable adverse effect [46]. Another experimental work carried out in 2013 evaluated the efficacy of the same S. platensis treatment in addition to corticosteroid injections in the treatment of oral submucous fibrosis symptoms. After 3 months of therapy, highly significant clinical improvements in mouth opening and reduction in burning perception were recorded in favor of the S. platensis group [47]. The reported effects indicate that S. platensis could be applied as an adjuvant therapy in the treatment of initial symptoms in subjects with OSF. Nevertheless, studies involving larger samples and longer follow-up are recommended in the future [48].
2.6. Salivary Secretion Improving
Salivary secretion is fundamental for the oral well-being, considering that hyposalivation compromises food chewing and swallowing, reduces mucosal immune function, increases the risk for oral diseases such as dental caries and candidiasis, and causes dysphagia, dysgeusia, and prosthetical inadaptation. Oral dryness is normally associated to aging or menopause, but it can also be caused by some pharmacological therapies, radio- and chemotherapy, or Sjogren’s syndrome. In any case, oxidative stress clearly plays a role in decreasing saliva secretion. Then, treatment with antioxidant agents, such as astaxanthin, may be beneficial [49].
Kuraji et al. (2015) estimated the effects of astaxanthin on the saliva secretory function of aging mice. The saliva flow increased in the case group 72 weeks after treatment, while that of the control decreased by half. Moreover, the submandibular glands of astaxanthin-treated mice had fewer inflammatory cells than the control did [49]. These results were corroborated by the work carried out by Yamada et al. (2010), which was structured in three parts. First, they evaluated the reactive oxygen species (ROS) scavenging capacity of astaxanthin on a human salivary gland epithelial cell line and obtained that the carotenoid partially suppressed hydrogen peroxide-induced ROS in salivary gland cells. Secondly, they examined the effects of astaxanthin on salivary secretion in a mouse model of irradiation-induced salivary gland dysfunction, resulting in the inhibition of oral dryness. Lastly, they tested astaxanthin treatment in six patients affected by Sjogren’s syndrome compared to a control group: an increase in salivary flow was detected in both groups of patients, and the level of oxidative stress marker, hexanoyil-lysine, in the saliva was decreased after astaxanthin administration [50].
According to Otsuki et al. (2016), Chlorella sp.-derived multicomponent supplementation, as well, is able to increase saliva production in subjects with lower levels of saliva secretion [51].
These results suggest that therapy with extracts derived from Spirulina sp. or Chlorella sp. has a good potential for the prevention and treatment of different clinical conditions of hyposalivation.
2.7. More Oral Benefits from Chlorella sp. and Other Algal Extracts
The long-term microalgal extract supplementation can bring several unexpected benefits to oral health.
C. vulgaris extract in conjunction with aminosulphurate (nutraceuticals) supplementation has determined a detoxification from heavy metals in subjects with long-term titanium dental implants and/or amalgam fillings compared to baseline levels and untreated controls. It is known how the accumulation of heavy metals represents a serious risk for human health. In particular, mercury toxicity can end in kidney dysfunction and neurologic anomalies. The administration of microalgae and nutraceutical supplements for 90 consecutive days reduced Hg2+, Ag, Sn, and Pb with respect to baseline levels and did not have any side effects [52].
Osteoclasts inhibition of the functionalized biosilica opens the way to interesting applications for diatom microalgae as a bioinspired mesoporous material for tissue engineering [53].
This entry is adapted from the peer-reviewed paper 10.3390/molecules25215164
References
- Mundt, S.; Kreitlow, S.; Nowotny, A.; Effmert, U. Biochemical and pharmacological investigations of selected cyanobacteria. Int. J. Hyg. Environ. Health 2001, 203, 327–334.
- Safonova, E.; Kvitko, K.; Kuschk, P.; Möder, M.; Reisser, W. Biodegradation of Phenanthrene by the Green Alga Scenedesmus obliquus ES--55. Eng. Life Sci. 2005, 5, 234–239.
- Ghasemi, Y.; Mohagheghzadeh, A.; Mohammad, H.M.; Moradian, A.; Shadman, S. Antifungal and Antibacterial Activity of the Microalgae Collected from Paddy Fields of Iran: Characterization of Antimicrobial Activity of Chroococcus disperses. J. Biol. Sci. 2007, 7, 904–910.
- Prakash, O.; Hussain, K.; Aneja, K.R.; Sharma, C. Synthesis and Antimicrobial Activity of Some New 2-(3-(4-Aryl)-1-phenyl-1H-pyrazol-4-yl) Chroman-4-ones. Indian J. Pharm. Sci. 2011, 73, 586–590.
- De Natale, A.; Pollio, A. Plants species in the folk medicine of Montecorvino Rovella (inland Campania, Italy). J. Ethnopharmacol. 2007, 109, 295–303.
- Perrin, S.; Fougnies, C.; Grill, J.P.; Jacobs, H.; Schneider, F. Fermentation of chicory fructo-oligosaccharides in mixtures of different degrees of polymerization by three strains of bifidobacteria. Can. J. Microbiol. 2002, 48, 759–763.
- Lee, M.H.; Kwon, H.A.; Kwon, D.Y.; Park, H.; Sohn, D.H.; Kim, Y.C.; Eo, S.K.; Kang, H.Y.; Kim, S.W.; Lee, J.H. Antibacterial activity of medicinal herb extracts against Salmonella. Int. J. Food Microbiol. 2006, 111, 270–275.
- Mazzanti, G. Pharmacological considerations on herbal medicine use. Ann. Ist. Super. Sanita 2005, 41, 23–26.
- Taguri, T.; Tanaka, T.; Kouno, I. Antimicrobial activity of 10 different plant polyphenols against bacteria causing food-borne disease. Biol. Pharm. Bull. 2004, 27, 1965–1969.
- Ferrazzano, G.F.; Cantile, T.; Roberto, L.; Ingenito, A.; Catania, M.R.; Roscetto, E.; Palumbo, G.; Zarrelli, A.; Pollio, A. Determination of the in vitro and in vivo antimicrobial activity on salivary Streptococci and Lactobacilli and chemical characterisation of the phenolic content of a Plantago lanceolata infusion. Biomed. Res. Int. 2015, 2015, 286817.
- Ferrazzano, G.F.; Roberto, L.; Catania, M.R.; Chiaviello, A.; De Natale, A.; Roscetto, E.; Pinto, G.; Pollio, A.; Ingenito, A.; Palumbo, G. Screening and Scoring of Antimicrobial and Biological Activities of Italian Vulnerary Plants against Major Oral Pathogenic Bacteria. Evid. Based Complement. Altern. Med. 2013, 316280, doi:10.1155/2013/316280.
- Ferrazzano, G.F.; Amato, I.; Ingenito, A.; Zarrelli, A.; Pinto, G.; Pollio, A. Plant polyphenols and their anti-cariogenic properties: A review. Molecules 2011, 16, 1486–1507.
- Galasso, C.; Gentile, A.; Orefice, I.; Ianora, A.; Bruno, A.; Noonan, D.M.; Sansone, C.; Albini, A.; Brunet, C. Microalgal Derivatives as Potential Nutraceutical and Food Supplements for Human Health: A Focus on Cancer Prevention and Interception. Nutrients 2019, 11, 6.
- Apone, F.; Barbulova, A.; Colucci, M.G. Plant and Microalgae Derived Peptides Are Advantageously Employed as Bioactive Compounds in Cosmetics. Front. Plant Sci. 2019, 10, 756.
- Camacho, F.; Macedo, A.; Malcata, F. Potential Industrial Applications and Commercialization of Microalgae in the Functional Food and Feed Industries: A Short Review. Mar. Drugs 2019, 17, 6.
- Langi, P.; Kiokias, S.; Varzakas, T.; Proestos, C. Carotenoids: From Plants to Food and Feed Industries. Methods Mol. Biol. 2018, 1852, 57–71.
- Suzich, J.B.; Cliffe, A.R. Strength in diversity: Understanding the pathways to herpes simplex virus reactivation. Virology 2018, 522, 81–91.
- Mader, J.; Gallo, A.; Schommartz, T.; Handke, W.; Nagel, C.H.; Günther, P.; Brune, W.; Reich, K. Calcium spirulan derived from Spirulina platensis inhibits herpes simplex virus 1 attachment to human keratinocytes and protects against herpes labialis. J. Allergy Clin. Immunol. 2016, 137, 197–203.
- Wong, T.; Wiesenfeld, D. Oral Cancer. Aust. Dent. J. 2018, 1, 91–99.
- Shibahara, T. Oral cancer -diagnosis and therapy-. Clin. Calcium 2017, 27, 1427–1433.
- Mori, H.; Tanaka, T.; Sugie, S.; Yoshimi, N.; Kawamori, T.; Hirose, Y.; Ohnishi, M. Chemoprevention by naturally occurring and synthetic agents in oral, liver, and large bowel carcinogenesis. J. Cell. Biochem. Suppl. 1997, 27, 35–41.
- Tanaka, T.; Makita, H.; Ohnishi, M.; Mori, H.; Satoh, K.; Hara, A. Chemoprevention of rat oral carcinogenesis by naturally occurring xanthophylls, astaxanthin and canthaxanthin. Cancer Res. 1995, 55, 4059–4064.
- Grawish, M.E. Effects of Spirulina platensis extract on Syrian hamster cheek pouch mucosa painted with 7,12-dimethylbenz[a]anthracene. Oral Oncol. 2008, 44, 956–962.
- Grawish, M.E.; Zaher, A.R.; Gaafar, A.I.; Nasif, W.A. Long-term effect of Spirulina platensis extract on DMBA-induced hamster buccal pouch carcinogenesis (immunohistochemical study). Med. Oncol. 2010, 27, 20–28.
- Schwartz, J.; Shklar, G.; Reid, S.; Trickler, D. Prevention of experimental oral cancer by extracts of Spirulina-Dunaliella algae. Nutr. Cancer. 1988, 11, 127–134.
- Kowshik, J.; Baba, A.B.; Giri, H.; Deepak Reddy, G.; Dixit, M.; Nagini, S. Astaxanthin inhibits JAK/STAT-3 signaling to abrogate cell proliferation, invasion and angiogenesis in a hamster model of oral cancer. PLoS ONE 2014, 9, 109–114.
- Azizi, A.; Aghayan, S.; Zaker, S.; Shakeri, M.; Entezari, N.; Lawaf, S. In Vitro Effect of Zingiber officinale Extract on Growth of Streptococcus mutans and Streptococcus sanguinis. Int. J. Dent. 2015, 2015, 489842.
- Zhou, Y.; Millhouse, E.; Shaw, T.; Lappin, D.F.; Rajendran, R.; Bagg, J.; Lin, H.; Ramage, G. Evaluating Streptococcus mutans Strain Dependent Characteristics in a Polymicrobial Biofilm Community. Front. Microbiol. 2018, 9, 1498.
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.L.; Cochran, D.; Sculean, A.; Canullo, L. How frequent does peri-implantitis occur? A systematic review and meta-analysis. Clin. Oral Investig. 2018, 22, 1805–1816.
- Komiyama, E.Y.; Lepesqueur, L.S.; Yassuda, C.G.; Samaranayake, L.P.; Parahitiyawa, N.B.; Balducci, I.; Koga-Ito, C.Y. Enterococcus Species in the Oral Cavity: Prevalence, Virulence Factors and Antimicrobial Susceptibility. PLoS ONE 2016, 11, e0163001.
- Davoodbasha, M.; Edachery, B.; Nooruddin, T.; Lee, S.Y.; Kim, J.W. An evidence of C16 fatty acid methyl esters extracted from microalga for effective antimicrobial and antioxidant property. Microb. Pathog. 2018, 115, 233–238.
- Uma, R.; Sivasubramanian, V.; Niranjali Devaraj, S. Preliminary phycochemical analysis and in vitro antibacterial screening of green microalgae, Desmococcus Olivaceous, Chlorococcum humicola and Chlorella vulgaris. J. Algal Biomass Utln. 2011, 2, 74–81.
- Madhumathi, V.; Deepa, P.; Jeyachandran, S.; Manoharan, C.; Vijayakumar, S. Antimicrobial Activity of Cyanobacteria Isolated from Freshwater Lake. Int. J. Microbiol. Res. 2011, 2, 213–216.
- Zarska, M.; Novotny, F.; Havel, F.; Sramek, M.; Babelova, A.; Benada, O.; Novotny, M.; Saran, H.; Kuca, K.; Musilek, K.; et al. Two-Step Mechanism of Cellular Uptake of Cationic Gold Nanoparticles Modified by (16-Mercaptohexadecyl) trimethylammonium Bromide. Bioconjug. Chem. 2016, 27, 2558–2574.
- Wei, L.; Lu, J.; Xu, H.; Patel, A.; Chen, Z.S.; Chen, G. Silver nanoparticles: Synthesis, properties, and therapeutic applications. Drug Discov. Today. 2015, 20, 595–601.
- Salaheldin, T.A.; Loutfy, S.A.; Ramadan, M.A.; Youssef, T.; Mousa, S.A. IR-enhanced photothermal therapeutic effect of graphene magnetite nanocomposite on human liver cancer HepG2 cell model. Int. J. Nanomed. 2019, 14, 4397–4412.
- Rashad, S.; El-Chaghaby, G.A.; Elchaghaby, M.A. Antibacterial activity of silver nanoparticles biosynthesized using Spirulina platensis microalgae extract against oral pathogens. Egypt. J. Aquat. Biol. Fish. 2019, 23, 261–266.
- Bosshardt, D.D. The periodontal pocket: Pathogenesis, histopathology and consequences. Periodontol. 2000 2018, 76, 43–50.
- Deas, D.E.; Moritz, A.J.; Sagun, R.S. Jr; Gruwell, S.F.; Powell, C.A. Scaling and root planing vs. conservative surgery in the treatment of chronic periodontitis. Periodontal. 2000 2016, 71, 128–139.
- Mahendra, J.; Mahendra, L.; Muthu, J.; John, L.; Romanos, G.E. Clinical effects of subgingivally delivered spirulina gel in chronic periodontitis cases: A placebo controlled clinical trial. J. Clin. Diagn. Res. 2013, 7, 2330–2333.
- Balci Yuce, H.; Lektemur Alpan, A.; Gevrek, F.; Toker, H. Investigation of the effect of astaxanthin on alveolar bone loss in experimental periodontitis. J. Periodontal Res. 2018, 53, 131–138.
- Hwang, Y.; Kwang-Jin, K.; Su-Jin, K.; Seul-Ki, M.; Seong-Gyeol, H.; Young-Jin, S.; Sung-Tae, Y. Suppression Effect of Astaxanthin on Osteoclast Formation In Vitro and Bone Loss In Vivo. Int. J. Mol. Sci. 2018, 19, 1–17.
- Kose, O.; Arabaci, T.; Yemenoglu, H.; Kara, A.; Ozkanlar, S.; Kayis, S.; Duymus, Z.Y. Influences of Fucoxanthin on Alveolar Bone Resorption in Induced Periodontitis in Rat Molars. Mar. Drugs 2016, 14, 70.
- Molteni, M.; Bosi, A.; Rossetti, C. The Effect of Cyanobacterial LPS Antagonist (CyP) on Cytokines and Micro-RNA Expression Induced by Porphyromonas gingivalis LPS. Toxins 2018, 10, 290.
- Orpha.Net. Available online: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=IT&Expert=357154 (accessed on 10 February 2019).
- Kanjani, V.; Annigeri, R.G.; Revanappa, M.M.; Rani, A. Efficacy of Spirulina along with Different Physiotherapeutic Modalities in the Management of Oral Submucous Fibrosis. Ann. Maxillofac. Surg. 2019, 9, 23–27.
- Shetty, P.; Shenai, P.; Chatra, L.; Rao, P.K. Efficacy of spirulina as an antioxidant adjuvant to corticosteroid injection in management of oral submucous fibrosis. Indian J. Dent. Res. 2013, 24, 347–350.
- Mulk, B.S.; Deshpande, P.; Velpula, N.; Chappidi, V.; Chintamaneni, R.L.; Goyal, S. Spirulina and pentoxyfilline-a novel approach for treatment of oral submucous fibrosis. J. Clin. Diagn. Res. 2013, 7, 3048–3050.
- Kuraji, M.; Matsuno, T.; Satoh, T. Astaxanthin affects oxidative stress and hyposalivation in aging mice. J. Clin. Biochem. Nutr. 2016, 59, 79–85.
- Yamada, T.; Ryo, K.; Tai, Y.; Tamaki, Y.; Inoue, H.; Mishima, K.; Tsubota, K.; Saito, I. Evaluation of Therapeutic Effects of Astaxanthin on Impairments in Salivary Secretion. J. Clin. Biochem. Nutr. 2010, 47, 130–137.
- Otsuki, T.; Shimizu, K.; Zempo-Miyaki, A.; Maeda, S. Changes in salivary flow rate following Chlorella-derived multicomponent supplementation. J. Clin. Biochem. Nutr. 2016, 59, 45–48.
- Merino, J.J.; Parmigiani-Izquierdo, J.M.; Toledano Gasca, A.; Cabaña-Muñoz, M.E. The Long-Term Algae Extract (Chlorella and Fucus sp) and Aminosulphurate Supplementation Modulate SOD-1 Activity and Decrease Heavy Metals (Hg++, Sn) Levels in Patients with Long-Term Dental Titanium Implants and Amalgam Fillings Restorations. Antioxidants 2019, 8, 101.
- Cicco, S.R.; Vona, D.; Leone, G.; De Giglio, E.; Bonifacio, M.A.; Cometa, S.; Fiore, S.; Palumbo, F.; Ragni, R.; Farinola, G.M. In vivo functionalization of diatom biosilica with sodium alendronate as osteoactive material. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 104, 109897.
