Spontaneous intracranial hypotension (SIH) occurs due to a leakage of the cerebrospinal fluid (CSF) lowering the pressure of subarachnoid space, mostly caused by a dural breach or discogenic microspur. As a result of less support provided by CSF pressure, intracranial structures are stretched downward, leading to a constellation of more or less typical MRI findings, including venous congestion, subdural effusions, brainstem sagging and low-lying cerebellar tonsils.
- spontaneous intracranial hypotension (SIH)
- myelographic imaging techniques
1. Introduction
2. Pathophysiology
The syndrome of SIH, in general, is a consequence of spontaneous CSF leaks along the neuraxis, almost invariably from the thecal sac of the spinal column [10][11][12][15,16,17]. Spontaneous leaks from the skull base are extremely rare [10][13][15,18]. Importantly, it has a distinct pathology from postdural puncture headaches or CSF hypovolemic conditions due to postoperative CSF loss or trauma [9]. Although the exact mechanism of spontaneous CSF leaks remain unknown, it is suspected that an underlying weakness of the spinal meninges is an imperative factor [14][19]. It creates a predisposition for the development of meningeal diverticula or perineural cysts, and subsequently spontaneous dural dehiscence. The presence of calcified degenerative thoracic disc protrusions may cause trivial traumatic events leading to progressive dural tears, which can be either ventral or lateral [7][14][15][7,19,20]. The CSF–venous fistula (CVF) is an important cause of SIH, which pose a diagnostic challenge [16][21]. Another rare, but interesting cause is the “nude nerve root” phenomenon, which describes the congenital absence of the entire nerve root sleeve [14][19]. The prevalence of SIH in certain connective-tissue disorders, particularly the Marfan syndrome, the Ehlers–Danlos syndrome (type II), and autosomal dominant polycystic kidney disease (ADPKD), are presumably due to the pre-existing dural fragility [7][8][13][7,8,18]. The old theories of SIH as a condition caused by CSF hypotension have been found to be inaccurate. A series of recent studies on larger samples by Luetmer et al. (2012), Yao et al. (2016), and Kranz et al. (2017), involving 388 patients, proved that only 21% to 55% of SIH patients had a low CSF opening pressure [17][18][19][22,23,24]. Following the data, it has been postulated that the reduction in CSF volume—rather than CSF pressure—is the primary pathogenetic factor [10][13][20][15,18,25]. Kranz et al. further advocated the concept of tissue compliance that determines the physiological relationship between pressure and volume [10][15]. Compliance with regards to the CSF component is highly dynamic and variable between individuals, as it is influenced by posture (upright vs. recumbent), body habitus, and the extent of the spinal epidural venous plexus [21][22][23][26,27,28]. It has also been demonstrated that the removal of CSF (via lumbar puncture) changes the spinal compliance due to the reduced spinal CSF volume [24][29]. Considering the fact that the rate of CSF loss is also different between individuals depending on mechanical factors, this may explain why not all SIH patients will have a low CSF opening pressure, despite a common unifying problem of low CSF volume. In 2019, an international jury of experts awaiting new radiological criteria confirmed the historic radiological definition of CM1 (cerebellar tonsillar position greater than or equal to 5 mm below the level of the foramen magnum) (agreement 83.7%) [25][32]. Different mechanisms may underlie the pathogenesis of CM1, primarily the underdevelopment of the posterior fossa bony structures. Several studies have shown that many, but not all, patients with CM1 have a small posterior fossa [26][33]. Another mechanism is represented by the presence of hemodynamic alterations that increase intracranial pressure. According to some authors, the delayed opening of the membrane covering the outlet of the fourth ventricle during fetal development could cause transient obstructive hydrocephalus with a consequent hernia of the hindbrain and cerebellar tonsils [27][34]. CM1 should be differentiated from cerebellar tonsil herniation secondary to space-occupying lesions (hydrocephalus, arachnoid cysts, brain tumors), and termed ‘acquired tonsillar ectopia’ by an international jury of experts (agreement 95.8%) [25][32]. Acquired tonsillar ectopia has an identical shape to the shape of the tonsils associated with idiopathic CM1, and may also be secondary to the downward displacement of the central nervous system due to decreased intrathecal pressure (either secondary to the over-drainage of lumboperitoneal shunting or a spontaneous CSF leak) [25][27][28][32,34,35]. In the latter case, careful clinical assessment, ascertaining postural headache, and thorough radiological assessment for intracranial CSF hypotension can help differentiate acquired Chiari malformation from true Chiari I malformation, and guide appropriate treatment (see paragraph 6). Although these mechanisms that act on the normal cerebellar tonsils, causing their deformation and herniation through the foramen magnum, are well understood, there is no consensus on the pathophysiology of CM1. For example, hydrocephalus has been proposed as both an etiologic cause and a consequence of a Chiari malformation.3. Classification of SIH
Several classification systems have been proposed as guidance for clinical management, as well as for academic discussion [29][30][36,37]. The most widely used classification of SIH was introduced by Schievink et al. in 2016 [29][36]. This classification is based on the three recognized morphological types of leaks—namely the dural tear, the meningeal diverticulum, and the CSF–venous fistula (CVF)—in combination with the findings of a presence (or absence) of extradural CSF on spinal imaging [31][32][30,31] (Table 1).|
Morphological Type of Leak |
Location of Leak |
|
|---|---|---|
|
Type 1 (60% of cases) - 1a - 1b |
Dural tear Dural tear |
Ventral dura Posterolateral dura |
|
Type 2 (20% of cases) |
||
|
- 2a |
Simple single or multiple meningeal diverticula |
Lateral dura |
|
- 2b |
Complex meningeal diverticula or dural ectasia |
Lateral dura |
|
Type 3 (20% of cases) |
Direct CSF-venous fistula |
Distal nerve root sleeve |
|
Type 4 |
Indeterminate origin |
4. Clinical Presentation of SIH
In a recent meta-analysis of 1694 SIH patients by D’Antona et al., headaches were almost invariably present—being reported in 97% of patients—and in the vast majority, they were orthostatic in nature [6]. This classic headache that characteristically worsens with an upright posture was most pronounced at the occipital region, although frontal and holocephalic headaches were also common. It may be attributed to the traction of the cranial nerves and the pain-sensitive dura mater, caused by the sagging of the brain in the CSF hypovolemia [3][33][34][3,38,39]. Typically, the headache is alleviated within 15–30 min after lying in a recumbent position [5][10][5,15]. However, the posture-related component of the headache may also vanish or dampen in a chronic condition [3][35][3,40]. Traction, distortion, or compression of some of the cranial nerves, certain structures of the brain, brainstem, mesencephalon, and diencephalon are believed to be the cause of many central nervous system manifestations, as well as the various cranial nerve palsies seen in this disorder [34][39]. Common associated symptoms include nausea/vomiting, neck pain/stiffness, tinnitus, dizziness, and hearing disturbances. Apart from that, there are a myriad of less frequently reported presentations which include other visual symptoms (photophobia, diplopia, blurred vision, nystagmus, visual loss), back pain, cognitive symptoms (including cognitive impairment, behavioral changes, memory, slow thinking), ear-related symptoms (vertigo, aural fullness, hyperacusis, or unspecified), reduced level of consciousness, and movement disorders (gait disorder, ataxia, dysarthria, tremor, bradykinesia, poor balance) [6]. Other rare, but peculiar symptoms, such as galactorrhea and hyperprolactinemia, have been attributed to the stretching or distortion of the pituitary stalk and/or hypothalamic region [36][37][41,42]; meanwhile, the dilatation of the epidural venous plexus or traction and compression of nerve roots are speculated to be the cause of radicular symptoms and incontinence [38][43]. Other less common, innumerable symptoms have also been described, including dysgeusia, sleepiness, other cranial nerve palsy, fever, fatigue, vocal tics, convulsions, facial spasms/numbness/pain, and dysphagia [6].5. SIH: Diagnostic Workup and Imaging Strategy
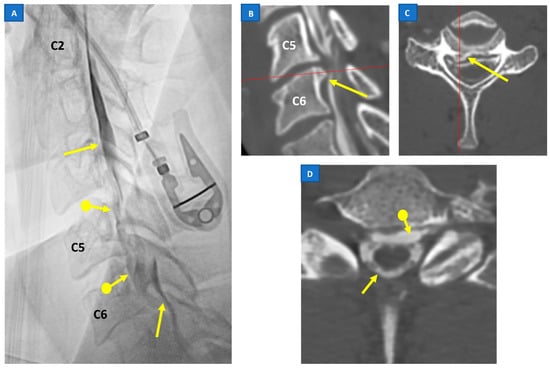
As lumbar puncture is an invasive procedure, in addition to the fact that only about half of the demographic shows a low CSF opening pressure, imaging emerges as the key aspect in the management of SIH. Furthermore, CSF analysis often exhibits considerable variability and is nonspecific for SIH [13][18]. Imaging plays a pivotal role both in confirming the diagnosis of SIH and localization of the leak point, which allows for the subsequent targeted therapy. A head MRI is the mainstay of initial imaging of SIH, as it is the most sensitive tool in detecting the signs of a CSF leak [6]. Nevertheless, while useful for confirming the diagnosis of SIH, brain MRIs are usually unable to localize the exact site and morphology of the CSF leak. Often, they need to be followed by other myelographic imaging techniques which have the advantage of depicting the direct evidence of CSF leakage (Figure 1), rather than the indirect signs seen with a cranial MRI [15][23][20,28].